|
E. Murat Tuzcu, MD - Professor of Medicine
- Department of Cardiovascular Medicine
- Cleveland Clinic Lerner College of Medicine
- Case Western Reserve University
- Vice Chairman
- Department of Cardiovascular Medicine
- Cleveland Clinic Foundation
- Cleveland, Ohio
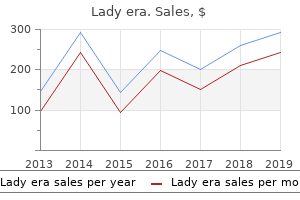
Lady era dosages: 100 mg
Lady era packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Order lady era usBilateral wrist views will indicate the presence of an axial (interosseous membrane) injury if the ulnar head is in positive variance in comparison with menopause herbal remedies order lady era from india the contralateral uninjured wrist. With the latter the surgeon can view a three-dimensional reconstruction, which is a helpful surgical planning software. An evaluation of humeral shaft bone loss is necessary in planning the implant design that might be considered. If the diploma of loss is larger than the articular condylar fragments, an implant that has the flexibility to restore humeral length will be extra acceptable. If an unreconstructable fracture of the humeral articular surfaces with out humeral shaft bone loss is encountered, an implant with the ability to resurface the articular surfaces as a hemiarthroplasty or a resurfacing ulnotrochlear substitute could be considered, however the former implantation technique should be considered an off-label and experimental procedure. Humeral shaft size loss of higher than 2 cm may be restored with implant designs with anterior flanges, particularly those with extended flanges that enable restoration of humeral length. The surgeon should assess the intramedullary canal dimensions of the humerus and ulna. Neurovascular status of the limb should be fully assessed and documented in the clinical notes. Patient positioned in a lateral decubitus place with the elbow draped over an arm help. Patient Positioning Two methods of patient positioning can be used, relying on surgeon consolation and the entry required: Supine: the arm is draped for optimum maneuverability. Lateral decubitus: the arm is positioned on an arm help, thereby minimizing the need for an assistant, however this set-up is less maneuverable. Surgical Approach Two major surgical approaches are helpful for acute complete elbow arthroplasty: Triceps-splitting method Bryan-Morrey method the triceps should be carefully managed in either approach, and it often has a skinny tendon, especially in older patients and those with rheumatoid arthritis. The triceps tendon ought to be dissected from the olecranon with a small curved scalpel blade, maintained perpendicular to the interface between the tendon and bone. Extend the incision 5 cm distal to and proximal to the prominence of the olecranon tip. With the nerve visualized and handled to security, remain within the medial gutter to lengthen the dissection distally to define the medial fracture fragment. Skin incision is posterior longitudinal, with or and not using a small diversion to avoid the "point" of the olecranon. Raising the skin should aim to keep the total thickness of the flaps by utilizing the "flat knife" technique. The medial fragment of the fracture is eliminated as soon as all the gentle tissues are launched from it, and the nerve is gently retracted to guarantee tension-free elimination. While in the lateral hall, visualize the radial head and resect enough head to forestall abutment on the prosthesis. From the lateral margin of the humeral shaft, increase the brachialis from 2 to 3 cm of the anterior surface. Preserving the integrity of the triceps insertion makes component insertion tougher. Define the medial triceps border and dissect the ulna nerve free from its connections, whereas defending it in a vessel loop. Release the triceps from the medial condylar fragments and transect the medial collateral ligament. Free the medial fragments from delicate tissue attachments and take away the medial fragments between the triceps and a gently anteriorly retracted ulnar nerve. A periosteal elevator is launched between the triceps and the humeral shaft and the two buildings are separated by sliding the elevator proximally after which distally to the level of the triceps insertion. Develop the interval between the anconeus and flexor carpi ulnaris alongside the subcutaneous border of the ulna. The triceps tendon is sharply elevated from the olecranon, in continuity with the anconeus, and subluxed laterally. Take care to release the Sharpey fibers adjacent to the bone so as to retain the flap thickness. Further access is afforded by elevating the anconeus from its ulnar attachment while maintaining its attachment distally. As the triceps is mirrored laterally, the lateral condylar fragments are recognized and removed by releasing the lateral collateral ligament and common extensor tendon. To dissect the Sharpey fibers off the ulna, the surgeon makes use of the scalpel parallel to the ulna surface and maintains the discharge instantly adjoining to the bone. Release the anterior capsule and any delicate tissue from the anterior floor of the distal humerus. Humeral canal preparation is accomplished with the canal broaches supplied with the implant system being used. The humeral component entry point, the apex of the olecranon fossa, is identified and humeral canal preparation is commenced by opening the canal with a bone nibbler or burr. The posterior flat floor of the humeral shaft is recognized and the component is aligned. Ulnar canal preparation is commenced by opening the canal at the base of the coronoid process with a drill or burr. The trajectory of the ulnar element (black ring) is prepared by rasping the entry monitor posteriorly into the ulna with a rasp or bone nibbler (gray crescent). The tip of the coronoid must be resected sufficiently to stop abutment on the humeral flange throughout full flexion. Also shown are the resections of the olecranon and the entry point for the ulnar stem insertion. The partially resected radial head is used as a bone graft for incorporation behind the humeral flange. During intramedullary preparation, the broaches must parallel the subcutaneous border of the ulna. This ensures that the track of insertion of the ulna parallels the intramedullary canal. Humeral insertion When bone loss is at or below the extent of the olecranon fossa, normal humeral insertion can happen. If bone loss happens above the olecranon fossa (greater than 2 cm), then humeral size have to be restored. When inserting the humeral component, place the bone graft behind the anterior flange. The prepared bony surfaces, with the fracture fragments removed, and just earlier than implantation. Maintain the element orientation relative to the posterior flat surface of the distal humerus. Seat the element and flange until the flange is totally engaged with the anterior cortex. The ulnar part is inserted such that the axis of rotation is recreated and the implant is perpendicular to the dorsal flat surface of the olecranon. Avoid tying the sutures immediately over the midline of the proximal ulna, which is a source of painful symptoms and will require knot removing.
Purchase 100 mg lady era free shippingThe laterally based mostly inferior flap of capsule is superior superiorly and medially and secured to the glenoid rim breast cancer hair bows discount lady era 100 mg with mastercard. The T capsulotomy is made two thirds from the highest of the capsule, with the vertical component adjoining to the glenoid rim. A deltopectoral approach to the shoulder is used and the strap muscles are retracted medially to expose the subscapularis tendon. A horizontal capsulotomy is now made in the midst of the capsule extending medial to the glenoid rim. The subscapularis is split horizontally consistent with its fibers at the junction of the higher two thirds and lower one third. The capsule is elevated off the glenoid subperiosteally to allow for superior and inferior capsular development. The laterally primarily based inferior flap is shifted superiorly and secured to the intra-articular portion of the glenoid rim utilizing transosseous sutures to try to recreate the labral "bumper. The process was designed to treat involuntary inferior and multidirectional instability of the shoulder that might not be addressed by restore of the anterior glenoid labrum alone (the Bankart procedure). The subscapularis tendon is incised about 1 to 2 cm medial to its insertion on the lesser tuberosity, leaving an adequate cuff of tissue for restore. The subscapularis consists of both a superior tendinous portion (two thirds) and inferior muscular (one third) portion. The arm ought to be able of adduction and exterior rotation throughout this inferior dissection, and great care is taken to shield the axillary nerve. By inserting traction on the capsular tag sutures in a superior and lateral path, the axillary pouch must be obliterated when an adequate amount of capsular dissection has been performed. It is necessary to release the inferior capsular attachments to the humerus, which have a broad insertion inferior to the articular floor. The medial insertion of the glenohumeral ligaments and glenoid labrum should then be assessed for avulsion or tear. Once secure fixation to bone is achieved, the capsule is shifted superiorly and laterally and the nonabsorbable sutures are passed by way of the capsule from an intraarticular to extra-articular location. A bimanual method can be used in which one needle driver is used to cross the suture and a second to "catch" the needle on the extra-articular facet. The sutures are then tied on the extra-articular facet to safe the capsule to the glenoid rim. In the inferior capsule shift process, the laterally based capsular incision is continued inferiorly utilizing tag stitches on the launched anterior capsule to apply traction. Release of the dual inferior capsular attachment, allowing an entire shift of the capsule. An anterior crimping (barrel) stitch is used to lower the redundancy of the anteroinferior capsule. Once tied, the barrel sew reduces anterior medial capsular redundancy and an anterior inferior bolster is created. The anteroinferior capsule is advanced superiorly and reattached to the capsular sleeve preserved on the humeral neck. The superior flap is sewn to the inferior flap to cut back volume and enhance strength. The rotator interval capsule is palpated between the subscapularis and supraspinatus tendons. Once the medial instability restore is full, attention is directed to lateral repair of the capsule to the remaining cuff of tissue on the humeral neck. A good basic guideline is to repair the shifted anterior capsule with the arm in 20 levels of abduction and 30 levels of external rotation. Excess tightening of the anterior capsule must be avoided to forestall the development of postcapsulorrhaphy arthropathy. In these shoulders, the capsular incision may be converted to a laterally based T capsulorrhaphy by incising the capsule between the inferior and center glenohumeral ligaments down to the glenoid rim. The inferior limb of the capsule is first repaired to its lateral insertion on the humerus. This will both scale back capsular quantity and reinforce the anterior capsuloligamentous tissues. If the rotator interval is widened or attenuated, it should be imbricated and closed using interrupted nonabsorbable sutures. The quantity of interval closure also wants to be titrated to the patient as talked about beforehand, as a end result of extra tightening of the rotator interval can lead to restriction of exterior rotation. Preoperative psychiatric analysis has been suggested however is seldom useful in screening these sufferers. With "partaking" defects, open therapy is favored over arthroscopic, and filling of the defect (autograft, allograft) may be considered. Significant defects (more than 30% of the glenoid) require a coracoid transfer (Bristow or Laterjet) procedure. These injuries are sometimes finest managed arthroscopically, and if suspected, might require diagnostic arthroscopy to verify and restore before an open incision. Passive forward elevation to one hundred ten levels and external rotation to 15 levels is begun at 10 days to 2 weeks, and is steadily increased to one hundred forty levels forward elevation and 30 degrees external rotation by 4 weeks. From 4 to 6 weeks, elevation is elevated to about one hundred sixty degrees and external rotation to forty levels. Resistive workouts are begun with the arm in neutral beneath 90 levels and progressed gradually. Full motion and energy ought to be regained earlier than contact sports activities are resumed, normally between 6 and 9 months, relying on the sport and the affected person. T-plasty outcomes: In 42 shoulders with a mean of 3 years of follow-up on this preliminary sequence, 95% of the sufferers were satisfied and there have been 4 recurrences (10%). A subsequent collection of twenty-two subluxators and 9 dislocators discovered 97% good to excellent outcomes and 94% return to sport. Nerve harm usually includes sensory perform only, and performance usually recovers spontaneously. Misplacement of labral tacks or suture anchors, both metallic and absorbable, could result in early arthrosis or arthritis. Complications because of positioning have been described including deep venous thrombosis and compression neurapraxia. Bony prominences must be nicely padded and constrictive bandaging avoided during and after surgical procedure. When it occurs, nonetheless, Propionibacterium acnes is a standard organism, and specific cultures must be requested. Neer16 reported on forty unstable shoulders that have been repaired with the anterior inferior capsular shift between 1974 and 1979, eleven of which had undergone prior procedures for glenohumeral instability. Satisfactory outcomes were achieved in all except one patient, who had postoperative subluxation of the shoulder. Although the surgical method and the extent of capsular shift could range with different surgeons, recurrence charges have ranged from 1. Long-term results of the Latarjet procedure for the remedy of anterior instability of the shoulder.
Diseases - Roussy Levy hereditary areflexic dystasia
- Sirenomelia
- Leiomyosarcoma
- Forney Robinson Pascoe syndrome
- Maghazaji syndrome
- Leukodystrophy, pseudometachromatic
- Infantile onset spinocerebellar ataxia
- Histidinuria renal tubular defect
Quality 100 mg lady eraThe reproducibility of classification of fractures of the proximal finish of the humerus breast cancer questions buy lady era cheap online. Conservative treatment of fractures and fracture-dislocations of the upper end of the humerus. Non-operative therapy of comminuted fractures of the proximal humerus in elderly sufferers. Numerous strategies of inner fixation for proximal humerus fractures have been described and reported, including cloverleaf and blade plating,1 Rush pinning,15,19 spiral pinning,18 Kirschner wire and pressure band fixation,three suture and exterior fixation,7 and intramedullary nail fixation. Various reviews have been made on the use of intramedullary nails in the proximal humerus. We choose to use an intramedullary nail that permits stable fixation of the pinnacle to the shaft of the humerus utilizing a minimally invasive rotator cuff�splitting approach (DePuy Inc. The technique for therapy of proximal humeral fractures described on this chapter includes a minimally invasive anterior acromial surgical approach, an indirect method of reduction, and a novel intramedullary rod designed to allow a wide selection of proximal interlocking configurations. Minor losses in the humeral length between the head and the deltoid insertion can alter the deltoid length�tension ratio. Vascular Supply of the Proximal Humerus the anterior and posterior humeral circumflex arteries are branches of the axillary artery. The arcuate artery, the terminal vessel of the ascending department of the anterior humeral circumflex artery, provides many of the humeral head. Avascularity of the humeral head can occur if this vessel is disrupted during a fracture of the anatomic neck. The posterior circumflex artery turns into essential in patients with proximal humerus fractures. It could be the main source of blood provide to the fractured head, so care should be taken to forestall further devascularization. Traumatic and iatrogenic vascular insult may lead to devascularization of the fracture fragments, resulting in delayed union, nonunion, and avascular necrosis. Innervation the brachial plexus is in danger in patients with upper extremity harm, and thorough neurologic evaluation is mandatory. The position of the top is higher than the tuberosities, and changes in this relationship will cause impingement. The humeral head is retroverted roughly 30 levels (range 20 to 60 degrees). The head is slightly larger than the tuberosities, barely medial and posterior to the humeral shaft, retroverted 30 levels. The lateral entry site for locking screw fixation (4�5 cm distal to the tip of the acromion) places the axillary nerve in danger. Axial load transmitted to the humerus may trigger impacted fracture in osteoporotic bone. Violent muscle contractures, as in grand mal seizures and electrical shock, are related to posterior dislocation as a outcome of overpowering inside rotators and adductors. Pathologic causes embrace tumor, a quantity of myeloma, and metastatic or metabolic problems. Osteoporosis is associated with fractures of the proximal humerus (more than some other fracture). In a three-part fracture with intact greater tuberosity, the humeral head is pulled by the supraspinatus and infraspinatus tendons; if the tendons are intact, the humeral head is externally rotated. Rotator cuff tears Neurovascular harm: axillary nerve, brachial plexus Avascular necrosis of the humeral head often results from disruption of the arcuate artery. The axillary artery also could also be broken, but much less commonly, in fracture-dislocations. In patients younger than 50 years of age, violent trauma, contact sports, and falls from heights are liable for fractures. Acute, recurrent, or chronic dislocation without major Indications Two-part proximal humerus fracture Three-part proximal humerus fracture Certain four-part proximal humerus fractures Prerequisites Shoulder table, image intensification, and skilled radiology technician Be conscious of the educational curve (do not try nailing of a four-part fracture earlier than acquiring enough experience with two- and three-part fractures). The muscular attachments of the larger and lesser tuberosities will trigger abduction, external rotation, and inside rotation, respectively. A bolster is used to elevate the shoulder from the desk and to enable shoulder extension. Extension of the shoulder is critical to expose the entry website within the humeral head. Flexion of the shoulder will result in the acromion overlying the center of the humeral head within the sagittal plane, obscuring the entry web site or errantly directing an entry angle. Anterior cutout of the nail within the head fragment can simply occur in an osteoporotic humeral head with an associated larger tuberosity fracture. Contraindication: head-splitting, comminuted displaced humeral head fragment devoid of soppy tissue attachment Preoperative Planning Successful intramedullary nailing of the proximal humerus fracture depends on constant integration between picture intensification and the surgical steps. Patient positioning on a radiolucent table will enable the surgeon to use a minimally invasive approach. Any error on the entry web site will trigger inevitable problems with the the rest of the procedure. Positioning Positioning on the desk should permit orthogonal and overhead axillary views. Intramedullary nailing for isolated surgical neck fractures may be performed fully percutaneously using many of the strategies described in the following paragraphs. However, when tuberosity reduction and fixation are required, a wider method often is critical. The timing of the open method is decided by the sequencing of head, shaft, and tuberosity fixation. In the method we describe in this chapter, head�shaft fixation is achieved percutaneously utilizing nailing and interlocking screws before tuberosity fixation. Alternatively, an open strategy with tuberosity discount and fixation could be carried out earlier than nail insertion. The wires ought to be separated by enough distance to permit insertion of the nail between them (1. The K-wires must be directed within the longest axis of the humeral head within the axial plane. Confirmation of the proper placement within the axial aircraft is done by the overhead axillary view. Then the C-arm is positioned to view the development of the pins within the coronal airplane projection. Unfortunately, with internal rotation, extension also happens within the humerus and the humeral head, depending on the gentle tissue attachments. This preliminary pin will serve to orient the humeral head, specifically the desired degree of retroversion. Image intensification can be utilized to place a K-wire by way of the top according to intramedullary axis of the humerus. To achieve fracture reduction, the joysticks in the proximal fragment should be used to rotate the head while concurrently rotating the distal shaft manually to acquire true orthogonal views of the head in reference to the shaft. Combining rotation of the pinnacle fragment (K-wires) with the shaft (arm) is used to assist in fracture reduction. Manipulation of the fracture fragments with the K-wires permits disimpaction of the fracture, bettering the varus or valgus alignment.
Order discount lady era on lineThe affected person is asked to cough women's health clinic ucf lady era 100 mg lowest price, and the clinician observes to confirm the loss of urine. If urine leakage is witnessed by the clinician, the patient is then stated to have real stress incontinence. An various is to measure the postvoid residual with an ultrasound bladder scanner. The upper limits of a standard postvoid residual have been reported as 50 to 100 mL. The purpose of the cotton swab take a look at is to diagnose a hypermobile urethra related to stress incontinence. The clinician inserts a lubricated cotton swab into the urethra to the angle of the urethrovesical junction. When the affected person strains as if urinating, the urethrovesical junction descends and the cotton swab strikes upward. As a end result, will increase in intra-abdominal stress are not transmitted equally to the bladder and urethra. Instead, will increase in intra-abdominal pressure are transmitted primarily to the bladder. Therefore, as intravesical pressures exceed intraurethral pressure, urinary stress incontinence occurs. This landmark concept proposes that the management of urethral closure is mainly the interplay of the pubourethral ligaments, suburethral vaginal hammock, and pubococcygeus muscle tissue. DeLancey introduced the hammock concept in 1994 which states that the urethra lies on the supportive layer of the endopelvic fascia and anterior vaginal wall. This supportive layer positive aspects structural help by way of its lateral attachments to the arcus tendineus fascia and levator ani muscular tissues. During a cough the urethra is compressed in opposition to this hammock-like supportive layer with a resultant improve in urethral closure pressure. In a smaller share of women, stress urinary incontinence may be due to weakness in the internal urethral sphincter often identified as intrinsic sphincter deficiency. With extra severe stress incontinence, urine leakage may happen with activities that trigger even small increases in intra-abdominal stress, corresponding to strolling standing, or altering positions. Urodynamics must be reserved for elucidating extra complicated presentations of incontinence. Lifestyle and behavioral modifications embrace weight reduction, caffeine restriction, fluid administration, bladder coaching, pelvic flooring muscle workouts (Kegel exercises), and physical therapy (biofeedback, magnetic therapy, and electrical stimulation). Bulging of anterior vaginal wall on straining indicative of posterior rotation due to defective help urethral closing pressure. Alpha-adrenergic agonists (midodrine, pseudoephedrine), beta-adrenergic receptor antagonists and agonists (clenbuterol, propranolol), tricyclic antidepressants (imipramine), and serotonergic/noradrenergic reuptake inhibitors (duloxetine) have been tried, however restricted information exists for their use. The side effects from these various medications should be weighed in opposition to the benefit. The use of systemic estrogen to deal with stress incontinence has been controversial, and in recent publications, it has not been proven to improve the symptoms and should worsen or lead to the event of stress incontinence in some ladies. Incontinence pessaries and different intravaginal devices are used to bodily elevate and help the urethra, which restores regular anatomic relationships. As a result, will increase in intra-abdominal pressures are transmitted equally to the bladder and urethra and continence is maintained. Incontinence pessaries differ from pessaries for pelvic leisure in that incontinence pessaries have added options to particularly assist the urethra. These gadgets require shut medical supervision to avoid an infection of the vaginal epithelium or injury to the vaginal tissues. Patients are often given vaginal estrogen to decrease the chance of vaginal trauma and ulceration. These embody the stomach retropubic urethropexies (Burch procedures), bladder neck slings, and tension-free midurethral slings (tension-free vaginal tape, transobturator tape). Most of the stomach procedures and bladder neck slings aim to resuspend the hypermobile urethra to its normal anatomic position. Disadvantages of surgery embrace the dangers of an invasive process and the danger of failure with resumption of signs over time. Patients with intrinsic sphincter deficiency could profit from periurethral or transurethral placement of bulking agents to enhance sphincter tone. Incontinence pessaries differ from more frequent prolapse pessaries in that the majority incontinence pessaries have a portion of the gadget particularly designed to assist the bladder neck. The sling is supporting the urethra and bladder neck and the ends are anchored to or above the rectus fascia. Neurologic issues similar to stroke, spinal twine injury, Parkinson illness, multiple sclerosis, and diabetes mellitus can even trigger detrusor overactivity (Table 19-4). Many women complain of not with the ability to reach the toilet in time or of dribbling or leaking triggered by simply seeing a bathroom. Detrusor overactivity presents with signs together with urinary urgency, frequency, and nocturia. Given the wide differential for detrusor overactivity, patients should also be asked about neurologic signs, historical past of earlier anti-incontinence surgery, and hematuria (suggestive of most cancers, stones, or infection). Urodynamic research should be reserved for circumstances resistant to initial treatment, complicated cases, or if surgery is deliberate. Surgical treatments for urgency incontinence include sacral and peripheral neuromodulation, bladder injections, and augmentation cystoplasty. Posterior tibial nerve stimulation has been permitted for urinary frequency, urinary urgency, and urgency incontinence. Rarely, augmentation cystoplasty is required in patients with extreme refractory urgency incontinence. In instances the place an underlying etiology is identified, it should be handled appropriately. Idiopathic urgency incontinence, the commonest kind, is managed with a mix of lifestyle and conduct modifications, treatment, and sometimes surgery. The most typical drugs used to deal with urgency incontinence are anticholinergic medication with antimuscarinic results (Table 19-5). Anticholinergic drugs act by rising bladder capability and lowering urgency leading to decreased incidences of incontinence and decreased voids general. The effect might take up to four weeks, and due to this fact, premature discontinuation and dose adjustments must be averted earlier than this time. Side results of anticholinergic medicine embrace dry mouth, blurred close to imaginative and prescient, tachycardia, drowsiness, decreased cognitive perform and constipation. They are contraindicated in patients with gastric retention and angle closure glaucoma. Anticholinergic drugs ought to be prevented or used with warning in sufferers with dementia, as they could worsen this condition.
Purchase genuine lady era onlineFibroids of the cervix may cause problems in being pregnant and will lead to breast cancer questions for doctor purchase online lady era hemorrhage, poor dilation of the cervix, malpresentation, or obstruction of the birth canal. When evaluating an asymptomatic cervical fibroid, the potential of cervical cancer must be ruled out, after which the fibroid could be followed with routine gynecologic care. Symptomatic fibroids may be surgically removed however, relying on their location, hysterectomy somewhat than myomectomy could additionally be required. Less frequently, cervical stenosis may result from obstruction with a neoplasm, polyp, or fibroid. However, if egress from the uterus is completely or partially blocked, oligomenorrhea, amenorrhea, dysmenorrhea, or an enlarged uterus might outcome. Cervical stenosis can also impede entry to the endocervical and endometrial canals for diagnostic and therapeutic procedures. When symptoms are current or access to the endocervical or endometrial canals are needed, cervical stenosis can be handled by gently dilating the cervix. Prolonged patency can be improved by leaving a catheter within the cervical canal for a number of days after the stenosis is relieved. These are attributable to intermittent blockage of an endocervical gland and often broaden to no more than 1 cm in diameter. Nabothian cysts are more generally present in menstruating women and are often asymptomatic. Most often, nabothian cysts are found on routine gynecologic examination and require no remedy. These cysts differ from nabothian cysts in that they have a tendency to lie deeper within the cervical stroma and on the exterior surface of the cervix. Patients with imperforate hymen and transverse vaginal septa generally present with major amenorrhea at puberty and cyclic abdominal pain. Patients are genetically female with regular ovarian function and regular secondary sexual characteristics. Vulvar itching and lesions could be secondary to a variety of atopic and atrophic skin adjustments, irritants, and allergens. Diagnosis of vulvar lesions is made by palpation, visualization, magnified vulvoscopy, and biopsy. Treatment includes hygiene practices, avoidance of irritants, and use of medium- to high-potency topical steroids. There is a limited role for vaginal estrogens and surgical procedure in the remedy of those issues. A variety of cysts can arise on the vulva and vagina from occlusion of pilosebaceous ducts, sebaceous ducts, and apocrine sweat glands. Cervical polyps and fibroids are typically benign and can be eliminated if symptomatic. Cervical stenosis could additionally be congenital or idiopathic and may outcome from scarring from infection or surgical manipulation. When symptomatic, the stenosis could be treated with gentle dilation of the cervical canal. The patient says these helped minimally however her intense pruritus has been persistent for greater than a year. She was married for 35 years but is now widowed and has not been sexually lively in 3 years. You examine her and discover a thin white atrophic epithelium and a contracted, small introitus. An area of hypopigmentation surrounds the labia and the anus in a figure-of-eight sample. Surgical excision A 26-year-old G0 patient is out there in with a problem visit for a grievance of an intermittent painless mass on her vulva near the introitus. She is having issue sitting at work, and has not been in a position to train for three days because of pain. On physical examination, she has age-appropriate breast and pubic hair growth and regular exterior genitalia. Imperforate hymen Vignette 2 Your subsequent affected person is a 65-year-old G2P2 new affected person who has been referred from her major care provider for recurrent yeast vaginitis. You get hold of a transabdominal ultrasound, which reveals a hematocolpos and hematometra. All of the above Vignette 4 Your subsequent patient is a 13-year-old adolescent lady who presents with cyclic pelvic pain. Therefore, it will not be cheap to examine fungal futures, prescribe a long course of antifungal, or to verify a fasting glucose level to search for diabetes as a cause for recurrent yeast infections. Instead, this affected person wants a vulvar biopsy to determine the source of her pruritus. She has not been sexually lively in three years and her main grievance is vulvar pruritus so is unlikely to have chlamydial an infection or gonorrhea. Lichen sclerosis is a chronic and progress benign condition characterised by vulvar irritation and epithelial thinning. Symptoms embrace intense pruritus, ache, and anogenital hypopigmentation (whitening-often in a "keyhole" trend around the perineum and anal region). When left untreated, it may end up in distortion of vulvar architecture (loss of labia minora, constriction of the introitus, fissures, labial fusion, scarring). Despite its benign nature, vulvar biopsy continues to be required to rule out underlying atypia or malignancy. Vignette 2 Question 3 Answer C: the therapy of lichen sclerosis consists of affected person training, vulvar hygiene, cessation of scratching, and high-potency topical corticosteroid use. The objective of treatment is to scale back the symptoms (itching, burning, and irritation) and to avoid progression of the illness, which may result in loss of vulvar structure, introital constriction, labial fusion, and scarring. Transverse vaginal septum is also obstructive but a standard introitus is normally identifiable. The imperforate hymen sometimes presents with a tense vaginal bulge at birth or throughout menarche. It usually seems as a midline protrusion of the anterior vaginal wall into the vagina and, if severe, via the introitus. However, these are the most typical explanation for cutaneous cysts and are typically small and solitary. Leaving the Word catheter in place for several weeks offers the brand new tract time to reepithelialize hopefully leading to a way of long-term drainage. Marsupialization is often reserved for sufferers in whom the Word catheter has failed. A transverse vaginal septum and bicornuate uterus are sometimes nonobstructing malformations. This additionally explains why these diagnoses are made comparatively later-most typically at the start of pelvic examinations (vaginal septum) or when being pregnant is desired (bicornuate uterus).
Syndromes - CT scan of the head
- Uteropelvic junction obstruction - blockage of the kidney at the point where the ureter enters the kidney
- Ask about the costs of medications you will need to take afterwards.
- Heart rhythm problem (atrial fibrillation)
- Manage how much water is in the body
- Vomiting, possibly with blood
- Congestive heart failure

Purchase lady era with mastercardImportantly womens health 9 diet buy discount lady era online, the fracture line between the higher and lesser tuberosities lies just posterior to the biceps groove. The ascending department of the anterior humeral circumflex artery provides 85% of the blood supply to the humeral head. Most proximal humerus fractures are "fractures of senescence" in older people with age-related osteopenia. They additionally happen in younger individuals as the outcomes of highenergy accidents corresponding to bike or automobile accidents. Displacement of the tuberosities, however, affects the mechanics of the rotator cuff and is very poorly tolerated. All these qualities facilitate minimally invasive reduction and fixation techniques. In youthful people, proximal humerus fractures often end result from higher-energy accidents. These fractures commonly have greater fracture fragment displacement, rotator cuff tears between the tuberosities, and disruption of the periosteal sleeve. Other essential features of the history embrace: Previous historical past of damage to the affected shoulder Previous shoulder function History of numbness or tingling in the affected extremity Rule out elbow and wrist fractures, especially in osteoporotic sufferers with injuries ensuing from a fall on an outstretched arm. Examination ought to include pores and skin integrity, presence of ecchymosis, downward carriage of shoulder girdle, and deformity according to shoulder dislocation or acromioclavicular joint separation. Possible associated vascular injury may be determined by testing radial pulse and capillary refill. A complete series with these views allows the fracture configuration to be determined in enough detail. Radiographs are used to decide whether or not the fracture is a two-, three-, or four-part fracture and to assess the diploma of displacement. Elderly people usually sustain proximal humerus fractures as the results of low-energy injuries similar to slipping and falling. These accidents usually are very amenable to minimally invasive fixation methods, as a end result of the displacement is manageable and the periosteal sleeve between fracture fragments often is undamaged. The Y lateral view often allows the examiner to detect any posterior displacement of subtle greater tuberosity fractures. The bone could not hold the pins and screws well and could also be better treated with a more stable construct. Fractures with a comminuted larger tuberosity require suture fixation through the tendon�bone junction (required open approach). Comminution of the medial calcar region leads to unstable discount of the top onto the shaft. This process must be carried out solely in sufferers committed to consistent follow-up in the postoperative period. Pin migration is feasible and must be caught early to have the ability to keep away from potential harm to thoracic constructions. The pectoralis main muscle exerts an anterior drive on the shaft, resulting in anterior displacement of the shaft relative to the humeral head. Historically, 1 cm of displacement has been used as the criterion for clinically significant tuberosity displacement. Recently, however, even 5 mm of displacement has been considered an operative indication. Patients wear a sling for two to 3 weeks or until the proximal humerus feels stable with light inner or exterior rotation of the arm. This picture should be checked earlier than prepping and draping to confirm adequate visualization. Instruments may be launched by way of this portal to lever fracture fragments or pull fragments into decreased place. By sweeping posterior and superior, the larger tuberosity and its extent of displacement may be palpated. In three- and four-part fractures, the fracture line of the greater tuberosity is reliably zero. Therefore, the reduction portal is situated at the degree of the surgical neck and 1 cm posterior to the biceps groove. The C-arm is brought in parallel to the affected person, leaving the lateral facet of the arm free for instrumentation. The affected person ought to be positioned laterally on the table such that an adequate fluoroscopic view may be obtained. The C-arm fluoroscope is placed parallel to the patient, extending over the shoulder from the cephalad course. This place leaves the lateral shoulder fully accessible for instrumentation and pin fixation. The discount portal is situated on the degree of the surgical neck fracture roughly 0. A hemostat is applied to the skin (C) after which imaged (D) to confirm that this portal will be instantly on the degree of the surgical neck fracture. A small incision is made within the pores and skin, and the deltoid is spread bluntly to keep away from injury to the underlying axillary nerve. The location of the biceps tendon is estimated based mostly on surface anatomic landmarks. Subcutaneous tissues and the deltoid muscle are unfold bluntly using a straight hemostat to keep away from harm to the axillary nerve on the deep floor of the deltoid. An axillary or scapular Y radiograph is necessary to evaluate the extent of this displacement. Longitudinal traction is utilized to the arm, and a posteriorly directed pressure is applied to the proximal shaft of the humerus. A blunt instrument can be inserted into the fracture at the surgical neck to lever the top back onto the shaft. This maneuver could be a powerful discount software, but care must be used to keep away from additional injury or fracture to the humeral head during this maneuver, especially on osteopenic sufferers. The lengthy head of the biceps tendon can turn into interposed between the fracture fragments, precluding reduction. Pins ought to be smooth to keep away from damage to soft tissue upon insertion, and terminally threaded to keep away from backing out. The pins ought to enter at completely different instructions to improve stability of fixation construct. One pin should enter lateral to the biceps in a primarily anterior-to-posterior direction. Another pin should enter further laterally in a primarily lateral-to-medial direction. Stability must be checked under fluoroscopic imaging with reside, gentle inner and external rotation. The start line for the pins is roughly 5 to 6 cm distal to the surgical neck fracture line.
Effective 100 mg lady eraReconstruction of the nail matrix in a chronic harm ought to be approached with realistic expectations menopause chills 100mg lady era visa. Reconstruction of the nail matrix after tumor excision will depend upon the amount of nail bed excised and the quantity remaining. Preoperative Planning Management of malignant tumors involving the nail mattress requires an understanding of the protected stage of amputation (usually to the extent of the more proximal joint) and the necessity for sentinel node biopsy. Use of a portion of a surgical glove as a tourniquet is discouraged due to the chance of leaving the tourniquet on the base of the digit after restore and placement of the dressing. Minimal d�bridement of the nail matrix is carried out to preserve as much of the nail bed as possible. Repair of a nail mattress avulsion and resultant proximal germinal matrix disruption might require incisions perpendicular to the curved portion of the eponychial fold for exposure. Small areas (less than 5 mm) can be left to heal by secondary intention but might result in recurrent scarring and nail deformity. Harvest split-thickness nail mattress graft from the sterile matrix of the donor digit utilizing a no. Graft is carefully harvested by inserting the blade parallel to the nail mattress and taking it thin enough so that the blade can be seen through the graft. It might develop in a dorsal path, catching on garments and requiring frequent clipping. It is important to inform the patient that a nail will no longer grow at the fingertip. Dissect to the proximal portion of the distal phalanx on the anticipated location of germinal matrix. The distal interphalangeal joint is used as a landmark to guide dissection to the extent of the germinal matrix. It could also be tough to distinguish scar from residual germinal matrix after traumatic injury. To protect length yet totally ablate the nail, a full-thickness skin graft can be used to cover the distal phalanx. The distal phalanx is a singular area where a skin graft could survive even after being placed instantly on bone with out the presence of periosteum. Right small finger after nail mattress avulsion from fingertip trauma treated with nail bed ablation. Fullthickness skin graft was placed instantly on the distal phalanx to preserve length and keep away from revision amputation. An elliptical incision was made and all residual germinal matrix was eliminated with a scalpel. If the germinal matrix remains to be current, the nail will proceed to develop but will hook without sufficient bony assist. Three remedy options exist: doing nothing, reconstruction of the nail to produce a flatter nail with or without bone graft, and revision amputation. Additional gentle tissue bulk to the volar pad could also be required to help the reconstructed nail. Through these stab incisions, create subcutaneous tunnels to the radial and ulnar eponychium using the elevator. The lateral borders of the nail are lifted from the distal phalanx in an atraumatic method with a Kleinert-Kutz elevator. The wounds are closed and the stitch is placed to maintain the nail beneath the proximal nail fold. Failure to deal with a nail mattress laceration and concomitant distal phalanx fracture as an open fracture could end in osteomyelitis. Too much rigidity on the website of nail bed restore or a lack of support from the distal phalanx may result in a hook nail deformity. Nail progress An accurate restore of the nail matrix allows the nail plate to develop out with a smooth, flat look. The sterile matrix contributes cells which might be responsible for nail adherence to the underlying nail bed. Nail bed reconstruction the aim of reconstruction is to restore the nail mattress after loss as a outcome of trauma, scarring, or excision to enable extra normal progress. Reconstruction of the sterile matrix may be achieved with a break up nail bed graft from the adjoining nail bed, an adjoining digit, or a toe. Reconstruction of the germinal matrix and sterile matrix can be achieved with a germinal matrix and sterile matrix graft from the second toe. Any suture used to maintain the nail or silicone sheet inside the fold also needs to be removed at 5 to 7 days postoperatively. Sutures positioned in the pores and skin of the hyponychium or paronychium should be removed at 10 to 14 days after restore. The fingertip splint supplies protection of the tip and can permit earlier motion of the injured digit. Hypersensitivity of the tip may be present for 1 to three months after damage, and desensitization exercises could also be essential to promote use of the affected digit. Complications or unfavorable outcomes in the persistent setting include scarring in the sterile matrix, resulting in a break up nail or nonadherent nail; scarring on the eponychial fold, which may intervene with nail plate progress; and protracted nail progress after an unsuccessful attempt at nail ablation. Anatomy and physiology of the perionychium: a evaluate of the literature and anatomic study. Fingertip accidents are widespread, accounting for 45% of emergency room hand injuries. In the setting of wounds less than 1 cm2, secondary-intention therapeutic aided by daily dressing changes truly allows for increased recovery of sensation. The use of secondary-intention therapeutic for bigger injuries includes a prolonged period of dressing modifications with related threat of an infection and unfavorable scarring. If no bone is exposed, options embrace therapeutic by secondary intention, major closure, or pores and skin grafting. Secondary-intention healing aided by daily dressing changes supplies one of the best recovery of sensation and is suitable for wounds lower than 1 cm2. This can minimize function by causing joint contracture and distal tip tenderness because of poor delicate tissue protection of the bony prominences. Sewing the volar pores and skin tightly to the distal nail may end up in a cosmetically displeasing "hook nail. The eponychial fold ought to be stented open with both trimmed and thoroughly cleansed nail or different material. With amputations by way of the germinal matrix, any remaining unrepairable matrix must be removed to stop formation of a painful nail remnant. In terms of useful end result, therapeutic by secondary intention offers equal or better results for defects lower than 1 cm in diameter. Split-thickness grafts should be used solely on the ulnar aspect of the index, middle, and ring fingers.
Purchase discount lady era on lineBlood vessels form arborizations into the dermis of the pores and skin by way of entry portals within the dermal papillae breast cancer jordans 2014 100 mg lady era amex. After application to an appropriately ready wound bed, each split- and full-thickness grafts bear a process that has been generally termed "take. Plasmatic imbibition is the process whereby vitamins and oxygen are drawn into the graft by absorption and capillary action. This early part of graft assist is followed by inosculation and capillary ingrowth. Once capillary ingrowth happens and makes contact with the vascular community inherently current inside the graft, blood flow is re-established, and the skin graft takes on a pinkish hue. The new vascular connections between graft and bed, in addition to the model new fibrous connections, solidify graft adherence. The phenomenon of primary contraction refers to the tendency of a graft to shrink on elevation from the donor website. Substantial primary contraction is more typically related to full-thickness skin grafts than with split-thickness skin grafts. It is clinically necessary to remember that the immediate and long-term elasticity of full-thickness pores and skin grafts is much larger that in split grafts. It is that this elastic property that makes full-thickness skin grafts an ideal selection for use around joints. Full-thickness grafts are probably to stay about the same dimension and, for sensible functions, present little to no secondary contraction. Full-thickness pores and skin grafts have the capability to improve their floor area with limb development over time, whereas split-thickness grafts tend to decrease in dimension by a process of contraction, or, alternatively, their size remains static. Reinnervation the restoration of sensation in skin grafts is mediated by way of each peripheral ingrowth and direct progress into the graft from the mattress. Factors affecting reinnervation of pores and skin grafts include the placement and quality of the recipient bed, as well as the choice of full- versus split-thickness pores and skin graft. Timing of recovery is variable, with some sensory restoration at between four and 6 weeks post grafting. The velocity with which sensory recovery is realized is dependent upon the accessibility of graft neural sheaths to wound bed nerve fibers. Accessibility of neural sheaths is improved in fullthickness grafts over their split-thickness counterparts, and, due to this fact, sensory recovery in full-thickness grafts is both extra rapid and more complete. Properties of Skin Grafts Skin grafts have been used to present both short-term and permanent coverage, offering the inherent benefit of safety of the host mattress from extra trauma while additionally providing an necessary barrier to infection. Split-thickness grafts tend to adhere to wound beds more simply and under antagonistic situations that might not usually assist full-thickness graft viability. This characteristic of split-thickness pores and skin grafts provides a substantial advantage in managing troublesome wounds; nevertheless, sure disadvantages can come up from their use. Once healed, split-thickness pores and skin grafts undergo secondary contraction which, under uncontrolled conditions, can result in pathologic contracture. Additional disadvantages arising from using splitthickness pores and skin grafts embrace dyschromia, poor elasticity, and decreased sturdiness when referenced towards their fullthickness counterparts. Full-thickness skin grafts embrace the full thickness of the dermis, along with the epidermis. In the preliminary phases, fullthickness pores and skin grafts tend to not present the hardy "take" typically seen with split-thickness pores and skin grafts. To ensure full-thickness graft success, their use ought to be restricted to well-vascularized recipient beds solely. Once established, full-thickness grafts supply distinct advantages; particularly, secondary contraction is way less problematic. Their thickness provides more resistance to exterior trauma and tends to be much less more likely to expertise the dyspigmentation typically associated with split-thickness grafts. Dyspigmentation the harvest of a graft disrupts its normal circulation, causing a lack of melanoblast content. After graft revascularization, the preliminary hypoxia is corrected, and the melanocyte inhabitants recovers to a traditional degree. Skin Substitutes using pores and skin substitutes for wound protection in the distal higher extremity sometimes is taken into account when the surface area involved is bigger than that which could probably be moderately covered with a full-thickness skin graft, but for which a splitthickness pores and skin graft is suboptimal, for cosmetic or useful causes. It is important to keep in mind the process whereby the graft turns into mated with the bed to obtain good end outcomes. Graft immobilization on the wound bed after placement is key to profitable adherence. Additional agents that act to prevent successful adherence embody the accumulation of subgraft hematoma or seroma in addition to shearing forces acting across the graft�wound interface. Immobilization strategies have to be directed toward the prevention of undesirable shear while offering pressure enough to minimize the buildup of fluid between graft and mattress. All efforts ought to be made to minimize the danger of an infection before graft utility by the use of d�bridement, lavage, and using each topical and systemic antibiotics, as directed by culture outcomes. Areas of pores and skin with plentiful epidermal appendages (sebaceous glands, sweat glands, and hair follicles) have inherent source tissue for re-epithelialization of those superficial wounds. If the method of re-epithelialization is complete by the tip of two weeks after the event of the initial damage, scarring at the website of injury might be minimized. Smaller wounds which are deeper and penetrate via dermis into the hypodermis could additionally be handled conservatively as nicely. Larger areas of skin loss allowed to heal by secondary intention can lead to a substantial delay in wound healing. In addition, functionally limiting contractures can develop as a byproduct of secondary intention healing. This class of dressing is efficient for superficial wounds that penetrate only to middermal levels. They rely upon retained epidermal appendages (ie, hair follicles, sebaceous and sweat glands) to accomplish the task of re-epithelialization. Deeper, full-dermal thickness areas of wounding require deeper d�bridements that typically are adopted by skin grafting or skin graft substitutes. The surgeon should confirm that all tissues throughout the potential graft mattress are viable and that bacterial growth within the wound is addressed through each wound d�bridement and treatment with appropriate antimicrobials. Other factors that negatively impression graft take are factors known to be answerable for impaired wound healing. The commonest of those are cigarette smoking, diabetes mellitus, and malnourished states. It is essential to elicit this data earlier than continuing with the operative plan. A quantitative culture may be carried out to assess this variable before pores and skin grafting. Before starting in the working room, the surgeon ought to have mentioned the proposed donor website with the affected person and in addition should have determined whether a full- or split-thickness graft is most acceptable. Positioning the volar and dorsal features of the distal higher extremity could be accessed simply with the affected person in a supine position with the arm placed on an arm desk.
Purchase 100mg lady era mastercardThe surgeon then returns the supracondylar ridge and begins elevating the anterior muscle with a Cobb elevator menopause osteoporosis order lady era 100mg. After excision of the anterior capsule, visualization of the ulnohumeral joint right down to the radiocapitellar joint. E Subperiosteally, the anterior structures of the distal humeral region proximal to the capsule are elevated to permit placement of a wide Bennett retractor. As the elevator moves from medial to lateral, the handle of the elevator is lifted fastidiously, preserving the blade of the elevator alongside the surface of the bone. When heterotopic ossification along the lateral distal humerus is profuse, the radial nerve is in danger if it is entrapped in the scar on the floor of the bone. The median nerve, brachial vein, and artery are superficial to the brachialis muscle. A small cuff of tissue of the flexor�pronator origin may be left on the supracondylar ridge because the muscle is elevated. A proximal, transverse incision within the lacertus fibrosus can also be needed to adequately mobilize this layer of muscle. Once the Bennett retractor is in place and the medial portion of the flexor�pronator has been incised, the aircraft between muscle and capsule must be rigorously elevated. As this plane is developed, the brachialis muscle is encountered from the underside. This muscle must be stored anterior and elevated from the capsule and anterior surface of the distal humerus. The dissection of the capsule from the brachialis muscle proceeds both laterally and distally. The first few occasions that this method is used, the coronoid seems fairly deep and much distal. A deep, slim retractor is often useful to enable the operator to see all the way down to the level of the coronoid. To see this area, a small, slender retractor may be inserted to retract the medial collateral ligament, pulling it medially and posteriorly. This affords visualization of the medial capsule and protection of the anterior medial collateral ligament. Once this edge of the capsule is incised, it can be lifted and excised as far distally as is protected. From this vantage, and after capsule excision, the radial head and capitellum can be visualized and freed of scar, as needed. In cases of main osteoarthritis of the elbow, removing the big spur from the coronoid is essential. Using the Cobb elevator, the brachialis muscle may be elevated anteriorly for two cm from the coronoid process. With the elevator held in place, defending the brachialis but anterior to the coronoid, the large osteophyte could be eliminated with an osteotome. Using the Cobb elevator, the triceps is elevated from the posterior distal floor of the humerus. The publicity ought to lengthen far sufficient proximal to permit use of a Bennett retractor. The posterior capsule may be separated from the triceps because the elevator sweeps from proximal to distal. In contracture launch, the posterior capsule and posterior band of the medial collateral ligament must be excised. The medial joint line up to the anterior band of the medial collateral ligament should also be exposed and the capsule excised. In contracture launch and in primary osteoarthritis, the tip of the olecranon usually should be excised to obtain full extension. The posteromedial joint line is definitely visualized, but the posterolateral facet must even be fastidiously palpated to ensure clearance. The sling can be customary by elevating two overlapping rectangular flaps of fascia or by using a medially primarily based flap connected to the underlying subcutaneous tissue. If a large enough cuff of tissue was left on the medial epicondyle, no holes want be drilled in bone. A small, narrow retractor is inserted to retract the medial collateral ligament, pulling it medially and posteriorly. The arm is elevated as much as attainable, and mechanical steady passive motion exercise is begun the day of surgery and adjusted to present as a lot motion as ache or the machine itself permits. After 2 days the plexus block is discontinued, and, at day 3, the continuous passive motion machine is stopped. Adjustable splints are prescribed, depending on the movement earlier than and after the procedure. A detailed dialogue concerning warmth, ice, and antiinflammatory medicine, along with a visual schedule for bracing, is offered. Because the principal objective is to acquire motion but to keep away from ache, swelling, and inflammation, routine use of an anti-inflammatory treatment is prescribed. Therapy with splints is sustained for about 3 months, throughout which era the patient is seen at 2- to 4-week intervals, if possible. After 4 weeks, an arc of about 80 degrees of motion is obtained, and the amount of time that each splint is worn is gradually decreased. The authors emphasize the need to release the exostosis and the collateral ligament when contracted, especially noting the necessity to launch the posterior portion of the medial collateral ligament and decompress the ulnar nerve when ulnar nerve symptoms exist preoperatively. A functional arc of flexion�extension (30 to 130 degrees) was obtained in 7 of the 14 elbows. According to those authors, the medial approach has a number of advantages over both the anterior and lateral approaches: Pathologic modifications in the posterior oblique bundle of the medial collateral ligament may be noticed and excised under direct imaginative and prescient. Anterior and posterior publicity is possible through one medial incision, through which a whole delicate tissue release and excision of part of the olecranon and coronoid course of may be undertaken if essential. Additional lateral publicity is indicated provided that the medial method has proved to be inadequate. In the medial strategy, the ulnar nerve is routinely released and protected under direct vision, which decreases the danger of harm. Etude retrospective de 23 arthrolyses du coude pour raideur post-traumatique: facteurs pr�dictifs du r�sultat. Posttraumatic contracture of the elbow: operative release utilizing a lateral collateral ligament sparing strategy. The lateral strategy for operative release of post-traumatic contracture of the elbow. The "column process": a limited surgical approach for the remedy of stiff elbows. Extrinsic contracture: the column procedure, lateral and medial capsular releases. Progressive surgical launch of a posttraumatic stiff elbow: method and consequence after 2�18 years in 46 patients. Correction of posttraumatic flexion contracture of the elbow by anterior capsulotomy. The medial approach for operative release of post-traumatic contracture of the elbow.
100 mg lady era mastercardOften menstrual discount lady era online mastercard, these deep approaches may be performed by way of a direct medial or lateral pores and skin incision or a extra versatile posterior incision. Triceps fascia and aponeurosis are exposed alongside the tendinous insertion into the ulna. Medial and lateral flaps are elevated, allowing full entry to the triceps tendon. The insertion of the triceps being elevated off the olecranon from medial to lateral. Triceps muscle is then break up in midline, and the distal humerus is exposed subperiosteally. Periosteum and triceps are elevated for a distance of about 5 cm proximal to the olecranon fossa, exposing the posterior facet of the joint. If more extensive exposure is desired, the subperiosteal dissection is extended to the level of the joint, exposing the condyles each medially and laterally. After the process, if an elbow contracture has been corrected, the joint ought to be maximally flexed. The tendon slides distally from its preliminary position, and the proximal muscle and tendon are reapproximated within the lengthened relationship. The distal a part of the triceps is then securely sutured to the fascia of the triceps growth, and the rest of the wound is closed in layers. Triceps-Reflecting Approaches the triceps mechanism could additionally be preserved in continuity with the anconeus and easily mirrored to one facet or the other. Three surgical approaches have been described that preserve the triceps muscle and tendon in continuity with the distal musculature of the forearm fascia and expose the complete joint. The ulnar nerve is identified proximally at the margin of the medial head of the triceps and, depending on the process, is both protected or fastidiously dissected to its first motor branch and transposed anteriorly. The fascia of the forearm between the anconeus and the flexor carpi ulnaris is incised distally for about 6 cm. This ought to be performed at 20 to 30 degrees of flexion to relieve pressure on the insertion, thereby facilitating dissection. If stability is necessary, these ligaments ought to be preserved or anatomically repaired on the conclusion of the surgical procedure. The medial border of the triceps is identified and released and the superficial forearm fascia is sharply incised to allow reflection of the fascia and periosteum from the proximal ulna. The extensor mechanism has been mirrored laterally and the collateral ligaments have been launched. To forestall this, the flap could be raised as an osteoperiosteal flap (see osteocutaneous flap approach). The flap is mobilized laterally, elevating the anconeus origin from the distal humerus till it might be folded over the lateral humeral condyle. Osteoanconeus Flap Approach this supplies glorious extension and dependable healing of the osseous attachment to the olecranon. This approach exposes solely the ulnar nerve, whereas the Mayo method translocates the nerve. Proximally, the triceps is identified and freed from the brachioradialis and extensor carpi radialis longus along the intramuscular septum to the extent of the joint capsule. The interval between the extensor carpi ulnaris and the anconeus is recognized distally. Sharp dissection frees the bony attachment of the triceps expansion to the anconeus from the lateral epicondyle. If further publicity is necessary, the anterior and posterior capsule can be launched. Routine closure of layers is carried out, but the radial collateral ligament must be reattached to the bone through holes positioned in the lateral epicondyle. The triceps attachment is launched from the ulna by osteotomizing the attachment with a thin wafer of bone. The collateral ligaments are either maintained or launched, relying on the pathology being addressed and the need for stability. Interrupted sutures are used to restore the remaining distal portion of the extensor mechanism. The olecranon has been osteotomized and the triceps swept from medial to lateral in continuity with the anconeus and forearm fascia. Closure with sutures positioned by way of bone and the distal extensor mechanism is completed with interrupted sutures. C Mayo Modified Extensile Kocher Approach the extensile Kocher approach and the Mayo modification of the extensile Kocher approach provide sequentially greater exposure from the initial Kocher strategy. The extensor mechanism (triceps in continuity with the anconeus) may be mirrored from lateral to medial. The ulnar nerve must be decompressed or transposed if an extensile lateral strategy is used. The triceps is reattached in a trend similar to that described for the Mayo strategy. The medial and lateral aspects of the triceps are identified and developed distally to the triceps attachment on the ulna. For distal humerus fractures fixation: the frequent flexors and customary extensors are partially released from the distal humerus to expose the supracondylar column for plate fixation. For total elbow arthroplasty or tumor resection: the frequent flexors and extensors are absolutely released from the medial and lateral epicondyle. The collateral ligaments and capsule are launched and the distal humerus is excised. The distal humerus is exposed by bringing it by way of the defect along the lateral margin of the triceps. Olecranon Osteotomy Worldwide, the transosseous strategy is probably the publicity most often used, especially for distal humeral fractures. The indirect osteotomy has almost been abandoned, and the transverse osteotomy has largely been changed by the chevron. Occasionally the medial or lateral collateral ligaments are launched for higher publicity. At the completion of the process, the tip of the olecranon is secured via tension-band or plate fixation. With any of the lateral exposures to the joint or to the proximal radius, the surgeon have to be continually aware of the potential of harm to the posterior interosseous or recurrent branch of the radial nerve. Chevron Transolecranon Osteotomy Intra-articular osteotomy, first described by MacAusland, was originally recommended for ankylosed joints. It has been adapted by some for radial head excision and synovectomy and used or modified by others for T and Y condylar fractures. The chevron osteotomy enhances rotational stability compared to a transverse osteotomy.
References - Coutinho JM, Ferro JM, Canhao P, et al. Cerebral venous and sinus thrombosis in women. Stroke. 2009;40:2356-2361.
- Parambil JG, Myers JL, Ryu JH. Histopathologic features and outcome of patients with acute exacerbation of idiopathic pulmonary fibrosis undergoing surgical lung biopsy. Chest 2005;128:3310-15.
- Platt R, Polk BF, Murdock B, et al: Mortality associated with nosocomial urinary-tract infection, N Engl J Med 307:637-642, 1982.
- Bascands JL, Schanstra JP: Obstructive nephropathy: insights from genetically engineered animals, Kidney Int 68(3):925n937, 2005.
- Ajani JA, Rodriguez W, Bodoky G, et al. Multicenter phase III comparison of cisplatin/S-1 with cisplatin/infusional fluorouracil in advanced gastric or gastroesophageal adenocarcinoma study: the FLAGS trial. J Clin Oncol 2010;28(9):1547-1553.
|

