|
Julie A. Braga, MD - Department of Obstetrics and Gynecology
- Dartmouth Hitchcock Medical Center
- Lebanon, New Hampshire
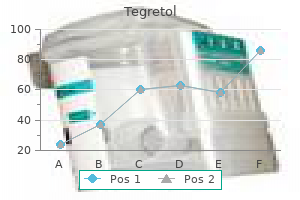
Tegretol dosages: 400 mg, 200 mg, 100 mg
Tegretol packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills
Generic tegretol 400mg without a prescriptionThe main hazards with injection of native anesthetics are hypersensitivity reactions and unintentional intravenous or intraarterial injection (see Chapter 29) muscle relaxant reviews generic tegretol 400mg otc. After steroid injection, roughly 2% of patients might experience an acute synovitis otherwise generally recognized as postinjection flare. Characterized by an increase in ache and joint swelling, symptoms usually start a few hours after steroid injection and might final so long as 3 days. These reactions can be stressful to the affected person who has anticipated relief, rather than exacerbation, from an injection. Histologically, steroid crystals have been seen within polymorphonuclear leukocytes, making it a real synovitis. Postinjection flare seems to be extra prone to develop with the extra soluble (shorter-acting) steroid solutions and may be associated to the carrier by which the steroid is manufactured. Although the trigger is obscure, this phenomenon might outcome from the trauma of needle insertion, penetration of infected tissue, or pressure on adjoining nerves from native swelling or bleeding. Another comparatively minor complication is localized subcutaneous or cutaneous atrophy on the site of the injection. These adjustments in the pores and skin happen when injections are made near the surface and a few of the injected steroid leaks back along the needle monitor. The skin despair usually recedes and the pores and skin returns to regular when the crystals of the steroid have been completely absorbed. These modifications are usually evident 6 weeks to three months after the initial injection and customarily resolve within 6 months, though they are often everlasting. The Z-tract approach is a technique of making an oblique route from the skin puncture to the final word website of the steroid injection. When the needle is midway via the fats tissue, redirect it to the target web site and inject both the anesthetic and the corticosteroid. Injection web site atrophy is more likely to happen with preparations which might be less soluble and thus longer acting. The precise etiology is unclear but could also be secondary to lowering the number and activity of melanocytes. Hydrocortisone would be the preferable agent for superficial injections to reduce depigmentation. One of the most severe issues after local steroid injection is tendon rupture. In common, the risk may be very low (<1%) and appears to be associated to the dose used. We nonetheless advise that one be diligent and cautious about injecting into the encompassing area of the tendon sheath and not into the tendon substance. Moreover, by using one measurement of needle and syringe, the operator is more likely to respect the rise in resistance when injecting immediately into the tendon. We additionally suggest limiting the frequency of injections to not extra than as soon as every three months in the same site. Specifically, intrasynovial injections of steroids have been shown to suppress the hypothalamic-pituitary-adrenal axis for two to 7 days. All corticosteroid suspensions, excluding cortisone and prednisone, can produce a significant and fast antiinflammatory impact (in the synovial spaces). Factors that affect the dosage and anticipated response include the scale of the affected space, the presence or absence of synovial fluid or edema, the severity and extent of any synovitis, and the steroid preparation selected (Table fifty two. For medium- or intermediate-sized bursae and ganglia on the wrists, knees, and heels, use 10 to 20 mg. Intrabursal remedy of the elbow (olecranon) or the knee (prepatellar) bursae, which comprise a considerable amount of fluid, may require 30- to 40-mg doses. However, if only a partial response occurs or if recurrence develops, a single injection can be repeated so long as one waits at least 12 weeks between injections. Corticosteroid preparations are categorized by their solubility and relative potency. The addition of tertiary butyl acetate to the answer causes decreased solubility and therefore an extended period of motion. For example, triamcinolone hexacetonide, the least soluble preparation has the longest period of action. In 1995 a survey of 172 rheumatologists found that opinions differ relating to almost each side of soppy tissue and intraarticular injection, together with affected person preparation, alternative of corticosteroid, and postinjection recommendation. The material required for local injection procedures consists of antiseptic resolution, needles, syringes, a hemostat, tradition and laboratory tubes, bandages, and sterile gauze. The ordinary sizes of needles for injection sites and corticosteroid doses are listed in Table 52. Needle and syringe Antiseptic Sterile gauze Hemostat Local anesthetic Culture tube Bandage Bursae and Tendon Sheaths local pores and skin anesthesia is an possibility earlier than injection however not universally practiced. For bursae and tendon sheaths, local anesthetics could be injected alone or with corticosteroids combined together in the same syringe. Use the Z-tract approach to limit the chance for a fistulous tract within the delicate tissue. Because the steroid might theoretically precipitate or layer within the barrel of the syringe during the injection, agitate the syringe immediately before utilizing it to optimize its distribution. In addition to minimizing the ache related to the injection, mixing an anesthetic with the corticosteroid additionally produces a bigger quantity for delivery. Caution the patient that the local anesthetic impact might wear off within a few hours and that the beneficial results of the corticosteroid could additionally be delayed. The optimum method for joint and gentle tissue injections has not been firmly established. However, one essential facet of a profitable technique is accurate positioning of the needle. Injecting an infected synovial space, such as a bursa containing fluid, may be as easy as puncturing a balloon. If the injection requires the appliance of serious stress, the needle may be in the tendon and ought to be withdrawn or advanced a few millimeters. Electric shocks felt with an injection may sign that the needle is in a nerve and must be repositioned. Although an correct injection is fascinating, using a generous quantity of anesthetic (3 to 6 ml) to dilute and hence disperse the steroid can compensate for lower than perfect injections. Asking the patient to use one finger to localize the area of most pain and tenderness is the easiest way to ensure essentially the most correct positioning of the needle. There are three usually accepted strategies for identification of trigger factors: flat palpation, pincer palpation, and deep palpation. Pincer palpation entails firmly grasping and rolling the muscle fibers between the thumb and forefinger until the taut band is found. Place a fingertip over the muscle attachment of the realm suspected of housing the trigger level and apply stress in numerous directions. It may be helpful to mark the set off level with a skin marker for easy identification earlier than therapy.
Purchase tegretol 200mg without a prescriptionFoley Catheter Removal of Esophageal Foreign Body 1 10- to16-Fr Foley catheter Deflated balloon 2 Balloon inflated Coin After administering topical anesthesia and/or mild sedation muscle relaxant usa buy tegretol 200 mg without a prescription, insert an uninflated Foley catheter (10 to sixteen Fr in children) in order that the tip is previous the international physique (as visualized on fluoroscopy or estimated by radiographs). Coin Fill the catheter balloon slowly with three to 5 mL of saline or distinction material (if fluoroscopy is used). Once the foreign body and the catheter tip reach the hypopharynx, grasp the object with forceps, or instruct the affected person to spit it out. Complication rates are decrease when the catheter is inserted orally and customarily lower at facilities that perform the procedure regularly. Failure to either remove the item or displace it into the stomach occurs in approximately 2% to 10% of rigorously chosen patients,75,79,80 but success charges are decrease in adults or patients with underlying esophageal disorders. Parents of youngsters who swallow coins could be instructed to look forward to cash in their stool. Indications and Contraindications Strict patient choice is paramount for successful and uncomplicated bougienage. The standards have changed little since initially proposed and define a gaggle in whom a round, clean object may be forcibly passed into the abdomen with little threat. It is essential to confirm the period of esophageal impaction to avoid performing the process when there may be underlying esophageal harm. Plain radiographs are indicated to confirm coin location and the absence of multiple esophageal bodies. In some patients a bite block may be wanted; several tongue blades can be taped collectively for this objective. The patient could gag momentarily; ask the patient to swallow and gently cross the dilator past the cricopharyngeus muscle. Once previous the cricopharyngeus, extend the top to enable the bougie to move distally to the stomach with little resistance. Terminate the procedure immediately if pain or resistance to advancement is encountered. Pulmonary aspiration and inadvertent passage into the airway are potential complications. Likewise, traumatic pharyngeal and esophageal harm, starting from delicate self-limited bleeding to frank esophageal perforation with concomitant an infection, are possible but uncommon. Esophageal bougienage is a way for dislodging impacted esophageal coins by blind mechanical advancement of the coin into the stomach, a procedure first described in 1965. Although early articles suggested that esophageal bougienage must be carried out exclusively by pediatric surgeons, the approach is definitely mastered and utilized by emergency clinicians. Achieve topical anesthesia with gargled 2% to 4% viscous lidocaine, atomized 2% lidocaine, or topical benzocaine spray. The affected person might gag momentarily; ask him to swallow, after which gently move the dilator previous the cricopharyngeus muscle. Coin in distal end of esophagus 3 Once past the cricopharyngeus, prolong the top to allow the bougie to cross distally to the stomach with little resistance. In most cases the ingestion is quickly realized by a caretaker, and in the majority of instances the coins pass uneventfully. Rarely, esophageal cash can cause airway distress by exterior compression of the trachea and simulate an asthmatic assault. Coins under the diaphragm are asymptomatic, and the presence of ache or symptoms requires additional evaluation. Here, the child swallowed a souvenir penny, which is seen within the area of the aortic crossover. It is advisable to additionally routinely obtain a lateral radiograph to decide whether a number of cash are stacked on top of one another. Overall, roughly 25% of cash will pass spontaneously, even when the coin is located proximally. Observation for 8 to 16 hours is an affordable strategy for asymptomatic youngsters if the ingestion has taken place inside 24 hours. Coins within the higher and center third of the esophagus are less likely to cross spontaneously, and a few favor to take away them as quickly because the diagnosis is made. Regardless of the approach, a radiograph ought to be taken simply earlier than removing to be sure that spontaneous passage has not occurred. If the patient is asymptomatic, the coin could additionally be eliminated immediately, or the patient could also be observed both as an inpatient or at residence. All are choices for single cash current within the esophagus for lower than 24 to 48 hours. Approximately two thirds of ingested coins are within the abdomen at the time of first investigation, and such sufferers may be launched home safely to allow almost certain spontaneous passage with a normal diet. Spontaneous passage of a coin from the stomach to the anus usually requires three to 7 days. If a follow-up radiograph demonstrates a persistent coin within the intestines for greater than 3 to 4 weeks, an obstructive lesion could also be present, and additional analysis is warranted. Theoretically zinc can lead to mucosal ulceration from its caustic nature91; nonetheless, the proof to date suggests no elevated threat from ingested pennies. Those with minor complaints may be evaluated safely over a interval of a few days, often as outpatients. In cooperative sufferers, cautious examination of the oropharynx must be accomplished by both direct or indirect laryngoscopy, or both. If the patient feels ache in the upper a part of the throat, special attention is directed to the tonsils as a end result of bones usually lodge on this area. This digital radiograph was by accident exposed 3 times; actually, only one coin was swallowed and x-rayed thrice throughout minimal movement. This can be accomplished with native oropharyngeal anesthesia by topical spray and direct visualization with a laryngoscope blade or business videoscope blade, after which removal of any bone with forceps. For these causes, a two-tiered, however individualized strategy to managing these sufferers is proposed. Carefully study the tonsils, posterior pharynx, and base of the tongue, which are widespread locations for bones to lodge. If the bone is removed and the symptoms disappear, no further intervention is required and follow-up is instituted as needed. Persistent signs are cause for further evaluation based on individual circumstances. If no bone is seen on physical examination, the bone might have passed after inflicting native irritation that persists, or the bone is present and not visualized due to location or consistency. Minor signs in the upper a half of the throat most likely represent persistent native irritation. Such objects embody tacks, pins, open paper clips, bobby pins, toothpicks, and razor blades. The solely appropriate removing technique is beneath direct visualization with endoscopy. Swallowed dentures or partial plates are a particular hazard in aged, demented, or mentally challenged patients.
Discount tegretol online american expressWithout removing it muscle relaxant norflex order generic tegretol on-line, redirect the needle in a special volar path, and repeat the process. Deposit a total of 5 mL of anesthetic in a fanlike pattern in every metatarsal house. Again, due to sensory overlap, two or extra spaces must be anesthetized for every toe to be blocked. For an online house block, select a site on the dorsum just proximal to the bottom of the toe. This serves to block the dorsal nerve and reduce pain at the needle insertion website. Advance the needle simply lateral to the bone toward the sole until the needle tents the volar pores and skin slightly. In this manner, two columns of anesthetic are positioned on both sides of the toe within the area through which the four digital nerves run. For blocks done within the toe itself, the process is similar, however smaller amounts of anesthetic. Alternative strategies using a single injection website, as described for the finger, may be carried out. Complications and Precautions Complications of lower extremity nerve blocks are similar to those associated with nerve blocks carried out within the upper extremity and embody intravascular injection, local anesthetic toxicity, nerve trauma, hematoma formation, and failure of the block. Ischemic problems could be avoided by taking note of changes within the skin in the course of the injection. If the pores and skin blanches, halt the process and reevaluate the position of the needle and the quantity and content material of the injected resolution. A toward the sole till the needle barely total of two to 4 mL of anesthetic is usually tents the volar skin. Redirect the needle (without fully removing it) across the dorsal floor of the toe. Inject anesthetic on the dorsal surface of the other facet of the toe, after which take away the needle. Insert the needle by way of the newly anesthetized area, and block the dorsal and volar nerves on this side of the toe. Nerve stimulators may be used to determine larger nerves and ensure proper placement of anesthetics. Additionally, some nerve blocks, such because the scalene block, may be avoided due to concern concerning adjoining anatomic structures. Use of ultrasound allows the clinician to establish the nerve in query, as well as to instantly guide the application of anesthetic. Furthermore, close by structures corresponding to arteries or veins may be recognized and prevented, thereby offering the operator larger confidence in performing more advanced blocks. Despite a restricted number of randomized controlled trials, preliminary evidence seems to assist the use of ultrasound, especially with regard to affected person safety. Peripheral nerves have a attribute appearance when considered by ultrasound and are normally simply identified, particularly in the transverse orientation. They are hyperechoic (white) in appearance and are generally round or oval, although some may also appear more triangular. In bigger nerves, the person fascicles could additionally be seen, especially when viewed with greater frequency. Nerve trunks (such as these used for scalene blocks) seem as rounded objects with a hypoechoic (darker gray) center. This may be accomplished by making use of shade flow Doppler and noting the absence of blood flow. Peripheral nerves are characterised by a brightly echogenic (white) texture and appear barely fibrillar. Use of this method will enable the sonographer to instantly follow the course of the needle because it travels toward the nerve. Once the nerve has been visualized, the "in-plane" technique is commonly essentially the most useful to information the needle to the selected area. Place the transducer within the transverse or slightly oblique aircraft relative to the nerve. Adjust the transducer in order that the nerve is additional away from the entry point of the needle. This will make sure that when the needle is inserted under ultrasound steering, it might be "adopted" because it advances towards the nerve in query. Once the picture has been obtained, introduce the needle from the tip of the transducer. Once the tip of the needle is seen adjoining to the nerve, inject anesthetic beneath direct ultrasound steering. The finest outcomes are usually obtained by injecting anesthetic in a sample that surrounds the nerve in a concentric manner. Nerve trunks appear similar to vascular buildings, with a hypoechoic (light gray) space surrounded by a hyperechoic (white) wall. The needle can be inserted from the midpoint of the transducer, although this system could cause more difficulty in following the tip of the needle. Detailed descriptions of the anatomy and strategy of the person nerve blocks can be discovered all through this chapter. However, it is important to discuss the nerve blocks sometimes carried out underneath ultrasound steerage as a outcome of the landmarks differ slightly. Interscalene Block the interscalene nerve blocks focuses on the trunks of the brachial plexus, particularly C5, C6, and C7. Blocking these trunks will present anesthesia to many of the shoulder and upper extremity and spare the medial elements of the arm and hand (these are innervated by the C8 and T1 nerve roots). This block is good for shoulder dislocations or advanced lacerations of the higher extremity. The trunks may be found grouped collectively in the neck and are sometimes simply identified with ultrasound. Because numerous crucial buildings are situated near these trunks, utilizing ultrasound to information the injection will offer the doctor increased confidence in the procedure, in addition to increased success in the block. Begin by putting the transducer, within the transverse orientation, lateral to the trachea on the degree of the thyroid cartilage. Move the transducer laterally till the interior jugular vein and carotid artery are visualized. Once these vessels are seen, proceed moving the transducer slightly laterally till the muscle bellies of the anterior and center scalenes are seen. The border between the muscle tissue may be delicate; nevertheless, shifting the transducer to a barely indirect plane could assist to better distinguish the anatomy. The trunks of the brachial plexus might be seen as rounded constructions mendacity between the muscle bellies. They sometimes have an echogenic (white) border with a hypoechoic (dark gray) to anechoic (black) heart. As famous beforehand, the nerve trunks can resemble blood vessels, so take care to consider the target buildings before inserting the needle. B, the anterior and center scalenes may be seen with the brachial plexus trunks lying between them (highlighted within the second image).
Buy tegretol 400 mg mastercardDiscontinue the fluid problem as soon as hemodynamic signs of shock are reversed or indicators of cardiac incompetence are evident muscle relaxant pregnancy category order tegretol canada. Cardiac Tamponade In cardiac tamponade, pericardial pressure rises to equal right ventricular end-diastolic pressure. Additionally, physician-operated point-of-care ultrasound has proven to be exceptionally sensitive for visualizing tamponade physiology when pericardial pressures have begun to impair proper ventricular filling. The number of issues increases, especially thrombosis and line an infection, with longer durations of indwelling catheters and growing severity of illness. Key issues and accidents by approach are mentioned within the following sections. In common, failure and complication charges enhance as the number of percutaneous punctures will increase. Historically, operator talent and experience have reliably predicted complication or success charges. Inadvertent arterial puncture and hematoma formation are usually simply recognized and managed with easy compression. In cardiac arrest, low-flow, or shock states, arterial puncture may not be apparent, and arterial cannulation and intraarterial infusions have occurred. This can lead to the event of ischemia or thrombosis of the artery and limb. In critically unwell patients, nevertheless, this complication could escape detection for some time. Mumtaz and coworkers cited a 3% bleeding fee in coagulopathic patients who skilled solely minor bleeding that could be controlled with digital strain. Initially, the significance of this complication was minimized, however stories of fatalities brought on by tension pneumothorax, bilateral pneumothorax, and combined hemopneumothorax adopted. A small pneumothorax can quickly turn into a life-threatening tension pneumothorax with optimistic pressure ventilation. Treatment of a catheter-induced pneumothorax is controversial, however not all patients would require formal tube thoracostomy. Air embolism is a really uncommon, however probably life-threatening complication of central venous cannulation. A chest radiograph ought to be taken routinely to assess the place of a central venous catheter introduced by way of the subclavian or internal jugular route. The catheter continues to be in place (large arrow), and the absence of lung markings on the best and the pleural reflection (small arrows) are readily apparent. B, Left hydropneumothorax after left subclavian venipuncture (the catheter was removed earlier than this radiograph). Note the straight line of fluid (air-fluid degree, black arrows) and no meniscus, indicating that a pneumothorax should even be current. No clinician can place central venous catheters and fail to have a minimal of some problems which may be inherent to the process, no matter even flawless method. A 14-gauge needle can transmit 100 mL of air per second with a 5�cm H2O strain difference throughout the needle. The really helpful therapy is to place the affected person within the left lateral decubitus position to relieve air bubble occlusion of the right ventricular outflow tract. Catheter or wire embolization resulting from shearing of a through-the-needle catheter by the tip of the needle is a serious and customarily avoidable complication. Adverse occasions after embolization embrace arrhythmias, venous thrombosis, endocarditis, myocardial perforation, and pulmonary embolism. Initiatives by nationwide safety bodies such because the National quality Forum in the United States have targeted on decreasing the incidence of retained wires by classifying them as "never" events that require mandatory reporting in many states. Delayed perforation of the myocardium is a uncommon, however typically deadly complication of central venous catheterization by any route. Emergency echocardiography, pericardiocentesis, and operative intervention by a thoracic surgeon could all be required for salvage of the patient. Catheter knotting or kinking could occur if the catheter is pressured or repositioned or if an excessively lengthy catheter is used. Neurologic problems are extraordinarily rare and presumably caused by direct trauma from the needle throughout venipuncture. Brachial plexus palsy and phrenic nerve injury with paralysis of the hemidiaphragm have been reported. Femoral venous catheterization carries a higher risk for an infection than subclavian catheterization. Merrer and associates reported the general infectious complication rate from femoral and subclavian catheters to be 19. Organisms most commonly recovered from colonized femoral catheters are coagulase-negative staphylococci, Enterobacteriaceae, Enterococcus species, and Pseudomonas aeruginosa. The risk for catheter-related thrombosis is directly related to the location of access. The relatively superficial location of the vein when approached from above the clavicle (1. Infectious Complications Infectious problems include local cellulitis, thrombophlebitis, generalized septicemia, osteomyelitis, and septic arthritis. The commonest quick complications involve bleeding from damage to both the femoral artery or the femoral vein. Extra care ought to be taken in anticoagulated patients or after the administration of thrombolytic brokers. Injury to the bowel is often minimal and unlikely to require particular treatment. Nonetheless, the potential bacterial contamination of the femoral puncture website can pose a major problem. Aspiration of air throughout placement of a femoral line necessitates removal of the catheter and reinsertion at another website. Other problems include muscular abscesses, an infection of the hip joint, harm to the femoral nerve, and puncture of the bladder. Strict consideration to sterile technique and limiting use to a few days will negate a lot of the negatives of this approach. A, Significant hemorrhage can occur after puncture of the femoral artery, but this area is instantly compressed. The femoral route could be the strategy of choice in a patient with an inadvertently placed arterial catheter who requires a central line. B, Bleeding from an inadvertently positioned arterial catheter that was removed with out adequate pressure in an anticoagulated patient. Patients with severe shock, asystole, or pulseless electrical activity will lack palpable femoral pulses, thus making percutaneous femoral vein catheterization more difficult. Attempts at percutaneous venous cannulation could additionally be complicated and even unimaginable in such patients. Venous cutdown, a time-honored surgical method, has largely been replaced by various methods of obtaining venous entry, including intraosseous strains, the Seldinger technique, and ultrasound-guided central and peripheral venous cannulation. First described by Keeley in 1940 and Kirkham in 1945,2,3 venous cutdown offered an different choice to venipuncture in sufferers with shock. Though no longer taught as a mandatory procedure in the Advanced Trauma Life Support course, venous cutdown is considered optionally available and continues to be taught at the discretion of the teacher.
Generic tegretol 400mg mastercardComplications Pain from needle insertion esophageal spasms xanax generic 400mg tegretol with amex, fluid injection, or bleeding Inaccurate readings because of poor technique, improper needle position, injected fluid or anesthetic, or exterior compression Injury to underlying tissue, nerves, or blood vessels Local or systemic an infection Review Box fifty four. A, this man was initially seen whereas in a coma from a heroin overdose and had been lying on his arm for a number of hours. B, Clear urine, a strongly optimistic dipstick for blood (arrow), and no purple blood cells by microscopy equate to myoglobinuria. C, When he awakened 20 hours later, the ache was severe, and compartment pressures indicated the need for fasciotomy. Heroin can cause rhabdomyolysis, and hypotension/reperfusion and positively prolonged strain on the muscular tissues might have exacerbated the situation. D, the basic wringer washer injury predisposes to compartment syndrome, but industrial rollers are actually normally the culprit. This chapter discusses the indications, problems, and interpretation of compartment pressure monitoring, in addition to the equipment and methods required to measure and monitor compartment pressure. Postischemic myoneural dysfunction and its associated contractures have been first described within the 1870s by the German surgeon richard von Volkmann, who acknowledged the consequences of increased pressure inflicting vascular compromise of the limb. The proximal end of the catheter is connected to a transducer and infusion system, which allows steady stress monitoring. Both the wick and slit catheters have been shown to provide comparable accuracy and reproducibility as long as patency of the catheter is ensured. This device uses a fluid-filled pressure measurement catheter, a pressure monitor, and a fluid infusion mechanism that maintains catheter patency and ensures accurate measurement. In contrast to earlier units during which comparatively massive volumes of fluid have been injected into the compartment to measure stress, the Stryker system uses a minimal amount of saline (< zero. They embody the "arteriovenous (aV) gradient" theory, which suggests that decreased aV pressure-perfusion gradients prevent sufficient blood supply37; the "critical closure" theory, by which blood circulate is arrested properly before the aV perfusion gradient declines to zero38,39; and the "venous occlusion" principle,40 which states that externally utilized pressure, thrombotic events, and reperfusion contribute to the increased compartment pressure and, in the end, tissue ischemia. Once blood move falls under a crucial degree, supply of oxygen to these buildings is impaired and aerobic mobile metabolism is no longer possible. Muscles then turn into ischemic, and a discount in venous and lymphatic drainage creates elevated stress inside this confined house. It is necessary to notice that ischemia and necrosis of the musculature can happen regardless of an arterial pressure excessive enough to produce pulses, due to this fact merely assessing distal pulses is inadequate. Hypotension can happen in a selection of settings, including hypovolemia, acute blood loss, cardiac disease states. Thus, the connection between intracompartmental pressure and the circulatory status of the extremity is a vital factor within the improvement of compartment syndrome. Studies of neuromuscular tissue ischemia have demonstrated that inflammatory necrosis can occur at intracompartmental pressures between forty and 60 mm Hg. In regular musculature, a P of less than 30 mm Hg results in loss of regular aerobic mobile metabolism. The Stryker system also has the flexibility to record a single measurement or present continuous compartment stress recordings when required. However, the fiberoptic transducer is relatively giant, should be hooked up to a sheath roughly 2. In current years, noninvasive, much less painful methods of measuring compartment stress have been studied in sufferers with each acute and continual exertional compartment syndromes. The remainder of this chapter describes essentially the most generally used gadgets and methods for measuring compartment pressures in the acute setting. The methodology chosen will depend upon the supply of the supplies and gear essential for a selected process and the experience of the operator. In the last decade, research means that muscle tissue could stay viable even after prolonged durations of ischemia and that a considerable proportion of the damage is generated throughout reperfusion. The authors found no distinction within the diploma to which phosphocreatine ranges fell between groups. In the group with compartment syndrome, these levels remained low even after fasciotomy. These outcomes counsel that elevated tissue stress performs a synergistic role with ischemia in mobile deterioration. However, due to their propensity for harm and the presence of several low-volume compartments, the decrease extremities are mostly affected. In the leg, the anterior compartment is involved most frequently,58 whereas the posterior compartment is most often related to a delayed analysis. The palms, toes, forearms, higher part of the arms, thighs, thorax, stomach, gluteal musculature, and back are different places where compartment syndrome is understood to occur. Treatment of fractures, by each open and closed discount, can improve compartment pressures. In addition, some proof suggests that compartment syndrome may occur within the setting of chronic exertion and muscle overuse. This underscores the necessity for serial examinations, significantly in these with equivocal or refined findings. Early signs of compartment syndrome embody a burning sensation over the involved compartment, nonspecific sensory deficits, or poorly localized deep muscular pain. Common features embody pain that seems out of proportion to the apparent injury and scientific examination and ache that intensifies when the musculature is passively stretched. Pallor, a pulse deficit with respect to the other limb, paresthesias, paresis, or paralysis are variably seen and lack diagnostic sensitivity. Neurologic complaints similar to weak spot and paresthesias could be confusing as a result of peripheral nerve injury may also outcome from the inciting trauma. When current, sensory deficits typically precede motor deficits and manifest distal to the concerned compartment. The interval between the harm and the onset of signs could be as quick as 2 hours and so long as 6 days. Frequently, the primary symptom described by sufferers is pain higher than expected given the medical scenario. Physical examination might reveal a tense compartment with a agency, "woody" feel, muscle tissue which may be weak, and hypoesthesia in the distribution of the concerned nerves. Sensory deficits, including lack of two-point discrimination and decreased vibratory sensation, may be present. The difficulty in diagnosing acute compartment syndrome was highlighted in a report by Vaillancourt and coworkers. The interval from the precipitating event to definitive surgery was as much as 35 hours, thus reflecting the problem in recognizing the presence of a compartment syndrome and instituting definitive remedy in scientific follow. Such statistics describe precise care, which can be lower than perfect in comparison with theoretical benchmarks. Notwithstanding the difficulties simply described, the analysis of compartment syndrome is primarily a clinical one that could be supplemented by direct measurement of compartment strain. In a examine evaluating the utility of clinical findings in making the prognosis of compartment syndrome, ulmer noted that the sensitivity and optimistic predictive worth of medical findings are low, whereas the specificity and adverse predictive value of those findings are excessive. The differential diagnosis of compartment syndrome is extensive and contains main vascular, nerve, and muscle injuries that produce comparable findings.
Syndromes - Fever
- CARES Foundation -- www.every1cares.org
- Fatigue
- Copperhead
- Tracheobronchitis
- Smoking
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen
- Ask your doctor which drugs you should still take on the day of your surgery.
- Swollen glands (lymph nodes)
200mg tegretolBardakjian and coworkers96 instructed that an oxygen saturation under 95% in the distal finish of the extremity as demonstrated by pulse oximetry (in the absence of systemic hypoxia) is also a reliable indicator of the necessity for emergency escharotomy spasms rib cage buy cheap tegretol 400 mg line. A, Patients with deep, nearly circumferential or circumferential chest wall burns could require escharotomy to facilitate air flow. B, Properly carried out escharotomy will result in immediate enchancment in extremity blood move. Patients with deep partial-thickness burns may still possess ache sensation, and escharotomy could also be carried out with local anesthesia or systemic analgesia. This ends in minimal bleeding, which can be controlled with native strain or electrocautery. These incisions, despite the very fact that life or limb saving, symbolize potential sources of infection for the burn affected person and ought to be handled as part of the burn wound. The wounds should be loosely filled with sterile gauze impregnated with an applicable topical antimicrobial corresponding to silver sulfadiazine cream. Fasciotomy, which includes a deeper incision, may be wanted for thermal or electrical burns. Limbs Under sterile circumstances, incise the lateral and medial features of the concerned extremity with a scalpel or electrocautery 1 cm proximal to the burned space and 1 cm distal to the involved area of constricting burn. Because joints are areas of tight pores and skin adherence and potential vascular impingement, incisions ought to cross these structures. Bold traces point out areas where warning is required as a end result of vascular constructions and nerves could also be broken by escharotomy incisions. In circumferential burns of the feet, if escharotomy is indicated, prolong the incision to the good toe medially and the little toe laterally. In circumferential burns of the hands during which escharotomy is indicated, prolong the incisions to the thenar and hypothenar elements of the hands. Softening of the compartment, improved distal tissue perfusion, return of sensation, Doppler move sign energy, and oximetry values indicate sufficient launch. Nearly all these sufferers are anticipated to be intubated and mechanically ventilated. Evidence of the need to release the eschar is elevated airway stress or an lack of ability to ventilate. Escharotomy of the chest wall should prolong from the clavicle to the costal margin in the anterior axillary line bilaterally, while avoiding breast tissue in females. This may be joined by transverse incisions to result in a chevron-shaped subcostal incision. Neck Neck escharotomy should be carried out laterally and posteriorly to avoid the carotid and jugular vessels. Complications Complications of escharotomy embrace bleeding, infection, and harm to underlying constructions. Complications of insufficient decompression include muscle necrosis, nerve harm (such as footdrop), and even amputation of the limb. Systemic complications of insufficient decompression include myoglobinuria and renal failure, hyperkalemia, and metabolic acidosis. Wearn C, Hardwicke J, Kitsios A, et al: Outcomes of burns within the aged: revised estimates from the Birmingham Burn Centre. American Burn Association: Hospital and prehospital useful resource for optimal care of patients with burn harm: tips for growth and operation of burn centers. Provider Manual 2011: American burn life assist course, American burn affiliation. American Burn Association/American College of Surgeons: Guidelines for the operation of burn facilities. Heck E, Head M, Nowak D, et al: Aloe vera (gel) cream as a topical remedy for outpatient burns. Subrahmanyam M: A potential randomized scientific trial and histological study of superficial burn wound therapeutic with honey and silver sulfadiazine. Subrahmanyam M: Honey dressing versus boiled potato peel in the therapy of burns: a prospective randomized study. Falkenstein N, Weiss-Lessard S: Hand rehabilitation: a fast reference guide and evaluate, St. Abe R, Shimizu T, Shibak A, et al: Toxic epidermal necrolysis and StevensJohnson syndrome are induced by soluble Fas ligand. Bentur Y, Tannenbaum S, Yaffe Y, et al: the position of calcium gluconate within the therapy of hydrofluoric acid eye burns. Prisoners and psychiatric patients ingest all kinds of objects, a few of which may be quite unusual: spoons, razor blades, pins, nails, or virtually another object. The time-frame underneath which this mandate should be carried out varies broadly and depends on many circumstances. Approximately one third of those objects could cross spontaneously within 24 hours, and some authorities have advocated an observational approach, though this tends to be more poorly accepted by dad and mom. Inquisitive youngsters regularly place objects in their mouth and unintentionally swallow them. As a end result, kids mostly ingest coins, however in addition they swallow buttons, marbles, beads, screws, and pins. Drooling is suggestive of high-grade obstruction, and full inability to handle oral secretions is a sign of total obstruction. Swallowed coins that lodge in the lower a half of the esophagus in kids may cause no overt symptoms till feeding is attempted. The time of the ingestion, size and form of the ingested object, and any present symptoms ought to be ascertained. In this case they are going to be drooling, spitting, and unable to deal with oral secretions. Examination of the oropharynx, neck, respiratory system, cardiac system, and abdomen is important within the analysis of potential problems. Children additionally commonly keep in mind an ingestion, but some may have a imprecise history or symptoms. This is especially true if transient coughing or gagging occurred, even though the precise ingestion was not witnessed. However, the constraints of plain radiography require that other diagnostic approaches even be thought-about. In nonverbal patients, including preschool children and these who are demented or debilitated, maintain a low threshold for screening radiography in instances with a suspicious history. This coin would probably be symptomatic in an infant and cause respiratory distress, drooling, wheezing, and possibly stridor. When used, a whole oropharyngeal radiographic sequence contains the nasopharynx to the lower cervical vertebra in both lateral and anteroposterior views. Patients must be positioned upright with the neck prolonged and the shoulders held low. Phonation of "eeeee" during radiography prevents movement artifact from swallowing, distends the hypopharynx, and enhances gentle tissue landmarks. Objects that turn out to be lodged within the center portion of the esophagus more than likely symbolize esophageal pathology, such as stricture associated to tumor or eosinophilic esophagitis. Coins on this area are more than likely to cross and be favorably manipulated by medicine (see Table 39.
Order 200 mg tegretol with amexA comparability of equianesthetic doses of lidocaine and bupivacaine for infiltration anesthesia (Table 29 muscle relaxant phase 2 block effective 100 mg tegretol. However, patients expertise a moderate amount of pain after restore of a laceration when the lidocaine wears off in approximately 1 hour. A prolonged length of anesthesia can be achieved by including epinephrine, sodium bicarbonate, or both to lidocaine. This latter property decreases the peak blood degree, reduces the potential for a toxic response, and permits a greater quantity of agent to be used for intensive lacerations. Bicarbonate added to the anesthetic just before injection decreases the pain of administration. The deciding components are many, however some logical decisions are as follows: � For a wound with excessive bleeding, use lidocaine with epinephrine and sodium bicarbonate. The larger most dose for options containing epinephrine appears in parentheses. Do not use for: Areas provided by end-arteries Patients "delicate" to catecholamines four. The objective of using bupivacaine is to delay the period of anesthesia; this effect can also be achieved considerably through the use of buffered lidocaine (plain or with epinephrine). Temperature Manipulation Warming an anesthetic to physique temperature (37�C to 42�C) reduces the ache of infiltration,77,78 however warming might not cut back injection pain as a lot as buffering with sodium bicarbonate does. Brogan and associates,80 utilizing lidocaine warmed to 37�C, discovered the warmed lidocaine and room-temperature buffered lidocaine to be equal during wound infiltration. Martin and coworkers81 found that warmed (37�C) lidocaine was no much less painful than buffered lidocaine. Leff and colleagues82 demonstrated that patients receiving native infiltrative anesthesia for restore of an inguinal hernia had less ache when the incision space was cooled earlier than infiltration. Patients were randomized to two groups and had a 1000-mL bag of saline positioned over the inguinal area for five minutes. One group used saline baggage at room temperature, the other group used saline bags cooled to 4�C. A vital lower in pain notion was found in the group in which the inguinal space was cooled before lidocaine infiltration. Injection the pain from injection of local anesthetics is primarily a results of pores and skin puncture (which can be minimized with smallgauge needles) and subcutaneous injection. Place the injection in subdermal tissue to reduce needle puncture pain and the tissue distention that occurs with intradermal placement. Place the needle "as much as the hub" and inject whereas withdrawing alongside the just-created subdermal tunnel to reduce tissue distention. After an preliminary injection, instead of totally withdrawing the needle from the tissue, redirect it alongside one other path to lessen the number of skin punctures. Hamelin and coworkers demonstrated that blinded volunteers receiving digital nerve block with 2 mL of lidocaine and epinephrine (1: one hundred,000) experienced much less ache when the answer was injected over 60 seconds somewhat than over eight seconds. If the injection is made via the minimize edges of the wound, a 25- to 27-gauge needle suffices. A small-gauge needle slows the speed of injection and reduces the rate and pain of tissue distention. A 10-mL syringe is beneficial each for its ease of dealing with and for the relatively gradual rate of injection that it permits. Technique Once an agent has been chosen, proper administration technique minimizes pain, prevents unfold of bacteria, and avoids intravascular injection. Buffering, temperature manipulation, and cautious infiltration additionally cut back the pain of injection. Buffering Raising the pH of an anesthetic by adding sodium bicarbonate decreases ache dramatically, whereas decreasing the pH by including epinephrine increases ache. Buffering might be one of the best ways to reduce the pain of native anesthetic injections, and its routine use is extremely really helpful. Sodium bicarbonate probably works by increasing the ratio of nonionized to ionized molecules, which either renders the ache receptors much less sensitive or causes more rapid diffusion of solution into the nerve and a shorter time to the onset of anesthesia. As the pH of the answer is raised, the anesthetic becomes unstable and has a decreased shelf life. It was initially recommended that buffered lidocaine be prepared simply before use to avoid precipitation and degradation, however buffered lidocaine retains its effectiveness for 1 week and refrigeration could additional increase its shelf life. However, ache typically happens with distention of tissue by the anesthetic, and therefore injection should be sluggish and deliberate. B, If a wound is grossly contaminated, the anesthetic could additionally be launched via the intact skin. The needle is first launched at a degree in line with the wound and past the wound edge (1), and whereas the anesthetic is slowly injected, the needle is advanced to include one entire side of the wound (if possible) to some extent well previous the other end of the wound. The other aspect may be anesthetized by passing the needle via the realm already infiltrated by the primary injection (3) to make the pores and skin puncture painless. Some clinicians select to inject the anesthetic via intact skin in patients with a grossly contaminated wound. Inject 1% lidocaine by way of intact skin with the needle bevel dealing with upward as a end result of that is much less painful than injecting with the needle bevel going through downward. For infiltration anesthesia with a smallgauge needle, however, aspiration is normally unnecessary unless the injection is deeper than the subcutaneous space or the area to be injected accommodates many giant vessels. Its reputation has waned considerably due to the worry (unproven and theoretical) of introducing infection on the fracture site and its limited efficacy. This method is beneficial for decreasing fractures of the distal finish of the forearm and hand. To perform the block, slowly inject 5 to 15 mL of plain 1% lidocaine into the fracture cavity and around the adjoining periosteum. A hematoma block is particularly useful when a Bier block and basic anesthesia are contraindicated. Prepare the pores and skin over the fracture site with antiseptic resolution and insert the needle into the hematoma, as confirmed by aspirating blood. Slowly inject 5 to 15 mL of plain 1% lidocaine or 5 to 10 mL of plain 2% lidocaine into the fracture cavity and across the adjacent periosteum. Adequate anesthesia happens in roughly 5 to 10 minutes and will last for several hours. The approach can present reduction for a quantity of circumstances, primarily postthoracotomy ache, postcholecystectomy ache, and most importantly for emergency clinicians, posttraumatic chest ache. Several research have demonstrated improved respiratory mechanics when intrapleural anesthesia is used. Angle the needle 30 to 40 degrees with respect to the skin and purpose medially, with the bevel up and directed simply above the rib. After perforating the posterior intercostal membrane (felt as a definite resistance), take away the stylet and attach a well-wetted, air-filled glass syringe to the Tuohy needle. Advance the needle till it enters the pleural area, which is denoted by the plunger being drawn down the syringe because of the adverse strain created during inspiration. Remove the syringe and introduce an epidural catheter 5 to 6 cm into the pleural house. Remove the Tuohy needle, get hold of a chest radiograph to verify proper position, and secure the catheter.
Buy generic tegretol on-lineCullen L quinine spasms tegretol 400 mg, Taylor D, Taylor S, et al: Nebulized lidocaine decreases the discomfort of nasogastric tube insertion: a randomized, double-blind trial. Ducharme J, Matheson K: What is the most effective topical anesthetic for nasogastric insertion Bai Y, Miller T, Tan M, et al: Lidocaine patch for acute ache management: a meta-analysis of potential managed trials. Soueid A, Richard B: Ethyl chloride as a cryoanalgesic in pediatrics for venipuncture. El Fakahany H, Medhat W, Abdallah F, et al: Frational microneedling: a novel methodology for enhancement of topical anesthesia earlier than pores and skin aesthetic procedures. Buhsem O, Aksoy A, Kececi Y, et al: Increasing topical anesthetic efficacy with microneedle application. Auerbach M, Tunik M, Mojica M: A randomized, double-blind managed research of jet lidocaine compared to jet placebo for ache relief in youngsters present process needle insertion within the emergency division. Hajiseyedjavady H, Saeedi M, Eslami V: Less painful arterial blood fuel sampling using jet injection of 2% lidocaine: a randomized managed medical trial. Saghi B, Momeni M, Saeedi M, et al: Efficacy of the jet injector in local anaesthesia for small wound sutures: a randomised medical trial in contrast with the needle infiltration method. Hajimaghsoudi M, Vahidi E, Momeni M, et al: Comparison of local anesthetic effect of lidocaine by jet injection vs needle infiltration in lumbar puncture. Oni g, Brown S, Burrus C, et al: Effect of 4% topical lidocaine utilized to the face on the serum ranges of lidocaine and its metabolite, monoethylglycinexylidide. Bartfiled J, Sokaris S, Raccio-Robak N: Local anesthesia for laceration: ache of infiltration inside vs outdoors the wound. Candiotti K, Rodriguez Y, Koyyalamudi P, et al: the impact of needle bevel position on ache for subcutaneous lidocaine injection. Dragoo J, Korotkova T, Kim H, et al: Chondrotoxicity of low pH, epinephrine, and preservatives present in local anesthetics containing epinephrine. Shinohara K, Iwama H, Akama Y, et al: Interpleural block for patients with multiple rib fractures: comparability with epidural block. Engdahl O, Boe J, Sandstedt S: Plasma concentrations and hemodynamic changes after repeated interpleural injections of bupivacaine-epinephrine. Kawasaki C, Kawasaki T, Ogata M, et al: Lidocaine enhances apoptosis and suppresses mitochondrial features of human neutrophil in vitro. Fedder C, Beck-Schimmer B, Aguirre J, et al: In vitro publicity of human fibroblasts to local anaesthetics impairs cell development. Orlinsky M, Hudson C, Chan L, et al: Pain comparability of unbuffered versus buffered lidocaine in local wound infiltration. Born g: Neuropathy after bupivacaine (Marcaine) wrist and metacarpal nerve blocks. Lalonde D, Bell M, Sparkes g, et al: A multicenter prospective examine of three,110 consecutive circumstances of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical section. Denkler K: A comprehensive review of epinephrine in the finger: to do or not to do. Abraham encounter with dental ache, Emergency physiciansthese injuriespatientsboth timeaconsumfacial lacerations, and other accidents of the top on regular basis. Thankfully, regional anesthesia for these situations is straightforward to instill, reliable, and safe. Techniques similar to nerve blocks can be utilized for patient consolation during repair of lacerations of the face, ear, brow, and, significantly, the lips. A block avoids direct infiltration into the precise laceration, which preserves the anatomy in these delicate areas and thus permits higher beauty restore. Nerve blocks can be used to give patients with dental pain virtually quick reduction. The capability of an emergency physician to master these blocks results in quick and efficient patient care as nicely as improved affected person satisfaction (Table 30. This is the largest of the 12 cranial nerves, originating on the upper portion of the pons. The ophthalmic nerve, V1, programs via the cavernous sinus and exits via the supraorbital fissure. These nerves and their branches innervate the eye, orbit, brow, and parts of the nose. It then splits into many branches that provide the dura and muscular tissues of mastication (motor function), as well as the buccal branch and the auriculotemporal, lingual, and inferior alveolar branches. These branches provide sensation to the skin on the facet of the head, the auricle of the ear, the tongue, the mucosa and skin of the cheek, the mandibular enamel, and the lower lip. Medications embody common anesthetics similar to lidocaine or bupivacaine, with or without epinephrine. The practitioner ought to all the time be aware of the utmost doses of anesthetic agents being utilized, though most blocks would require much lower than the utmost dosing. During and after injection, particularly when working in areas close to the lip, slight exterior pressure and massage not solely help the anesthetic diffuse to its goal but additionally assist stop ballooning of the lip or facial tissue. To apply a topical anesthetic, first dry the tissue with gauze and then apply a topical mucosal anesthetic, as an example, viscous lidocaine. Another technique is to soak a piece of gauze with the anesthetic after which place it over the dry mucosa. Spray anesthetics such as cetacaine are in style and efficient alternatives to lidocaine-soaked gauze. Supraperiosteal Injection Indication Supraperiosteal injection is generally used to obtain anesthesia of particular person maxillary enamel, however it might be used for any tooth. This block works well if the anesthesia is needed for only one or two teeth, and it could be very helpful to alleviate ache related to a simple toothache. As noted previously, care should be taken to keep away from inserting the needle by way of any infected tissue. Anatomy the nerves for every individual tooth enter at the apex of that tooth and are protected by the bone supporting the tooth. Once the anesthetic has had time to take impact, retract the lip till the tissues are taut (down and out for maxillary tooth and up and out for mandibular teeth). Intraarterial injection is unlikely on this block, however you must aspirate prior to slowly injecting 1 or 2 ml of anesthetic. Because the anesthetic must penetrate the bone, a couple of minutes are needed for anesthesia to happen. The danger of inoculating deeper tissues with bacteria is possible if the injection goes via contaminated tissue. Anesthesia can fail if the injection is too high, too low, or too distant from the nerve. For occasion, a tongue depressor is beneficial for use as a retractor, however another acceptable instrument or maybe a finger can be used for this function. One of them includes infected tissue: the needle should by no means be inserted through contaminated tissue because this approach might end in inoculation of deep tissue with micro organism. Although not an absolute contraindication, coagulopathy may current a higher threat for hematoma and bleeding complications, so, as for any process, the risks ought to be considered and may outweigh the advantages. B, Cutaneous branches of the trigeminal nerve and their exit points from the cranium. B and C, Adapted from Eriksson E, editor: Illustrated handbook in native anesthesia.
Cheap tegretol 400 mg with visaAnimal Bites Many features of the treatment of animal bites are controversial zma muscle relaxant discount 100 mg tegretol mastercard, and no common standards exist. Numerous organisms could be cultured from an infected bite wound brought on by a dog or cat, and cultures may guide antibiotic therapy in contaminated wounds. The predominant pathogens in animal bites are the oral flora of the biting animal and human skin flora. Approximately 85% of bites harbor potential pathogens, and the typical wound yields five forms of bacterial isolates; virtually 60% have mixed aerobic and anaerobic bacteria. Pasteurella species are isolated from 50% of canine chew wounds and 75% of cat chew wounds. When in contrast with dog bites, cat bites may turn into contaminated rather rapidly after the bite (within 24 hours), thus suggesting Pasteurella infection. Cat bite wounds are inclined to penetrate deeply, with a higher threat for osteomyelitis, tenosynovitis, and septic arthritis than with dog bites, that are associated with crush damage and wound trauma. Capnocytophaga canimorsus, a fastidious gram-negative rod, can cause bacteremia and deadly sepsis after animal bites, especially in asplenic patients or these with underlying hepatic illness. Anaerobes isolated from canine and cat chunk wounds embrace Bacteroides, fusobacteria, Porphyromonas, Prevotella, propionibacteria, and peptostreptococci. Puncture wounds from a canine can be problematic because Miscellaneous Aspects of Wound Care Traumatic wounds are created by a broad variety of mechanisms, and clinicians should generally adjust wound administration strategies to match particular circumstances. Aside from evaluating tetanus immunization status and considering the potential for a overseas physique, the clinician has few proven choices to prevent an infection in a puncture wound. Scrubbing the surface of the puncture, evaluating the opening for retained overseas matter, and trimming jagged pores and skin and tissue edges may be useful. The value or appropriateness of coring, probing, or irrigating the puncture track has not been established. The final course of a puncture wound is probably going set at the time of harm they usually often do properly. A�C, this nail gun puncture of the distal finger joint was able to be d�brided by D, passing a small hemostat by way of the puncture wound and pulling gauze via the wound. E, A small piece of metal, used to connect the nails collectively (arrows), was removed with this maneuver. F, Note that nails from a nail gun clip are held along with a bit of steel or glue which will hamper removal or be left in the wound. A splint and three days of cephalexin prophylaxis (because of the discovered foreign body) have been provided, and this wound healed well. Some clinicians have advocated major closure of huge dog bite lacerations that are centrally located on the body; nonetheless, markedly contused lacerations are good candidates for delayed major closure. Infected animal bites must be handled with antibiotics, but using prophylactic antibiotics for animal bites is controversial. Depending on location, canine bites could have an an infection price of 3% to 5%, whereas cat bites may turn into infected 50% of the time. Prophylactic amoxicillin-clavulanate (875/125 mg twice daily) given for three to 5 days could cut back infection rates after cat or dog bites, especially for a puncture wound, when the patient is seen more than eight hours after the bite, or when wound cleansing has been inadequate. D, After the entrance wound is d�brided of the powder burn, cross an instrument by way of the wound. E, For a similarly cleansed gunshot wound of the leg, depart the gauze packing within the observe for 48 hours. No antibiotics got, the pack was eliminated at wound examine in forty eight hours, and the patient did well. The greatest method to strategy bite wounds is solely to adhere to the basic principles of wound care. When a wound results from the chew or scratch of both a wild or a domestic animal, give rabies prophylaxis if indicated (Tables 34. When cultured, most contaminated human bites harbor three to 4 pathogens, together with each aerobes and anaerobes. Lacerations usually happen over the third and fourth metacarpophalangeal or proximal interphalangeal joints of the dominant hand. Relaxation of the fist could disseminate organisms into the deep compartments and the deep tendon spaces of the hand, predisposing the affected person to deep soft tissue an infection, septic arthritis, and osteomyelitis. Irrigate chunk wounds copiously with tap water or sterile saline, and remove grossly seen particles. Many clinicians will lengthen a small laceration to allow visualization of the underlying structures and higher cleansing. Wounds involving tendons or joint areas are more critical and require close follow-up. This patient was seen on a Monday morning with a small puncture wound on the dorsal surface of his hand (arrow), and he claimed that it was an damage sustained at work. Facial chew wounds are an exception; major closure may be thought of for these wounds. Consider splinting the hand able of operate with a short-arm volar splint for a few days to decrease joint movement. In making use of them, take into account the animal species involved, the circumstances of the chunk or other exposure, the vaccination standing of the animal, and the presence of rabies within the area. Local or state public health officers should be consulted if questions come up in regards to the need for rabies prophylaxis. Local and state public well being officials must be consulted on questions about the need for rabies prophylaxis. Bites of squirrels, hamsters, guinea pigs, gerbils, chipmunks, rats, mice, different rodents, rabbits, and hares virtually never call for antirabies prophylaxis. All bites and wounds must be immediately cleansed completely with soap and water. Vaccination may be discontinued if immunofluorescence tests of the animal are negative. Four formulations of three inactivated rabies vaccines are presently licensed for preexposure and postexposure prophylaxis within the united States. Most infections are polymicrobial, but use of antibiotics with exercise towards S. Amoxicillin-clavulanate (875/125 mg twice daily) for 3 to 5 days is a typical suggestion for monotherapy. Alternative empirical combination regimens include clindamycin (450 mg three times daily) plus trimethoprim-sulfamethoxazole (1 double-strength pill twice daily), or ciprofloxacin (500 to 750 mg twice daily), or moxifloxacin (400 mg once daily) for three to 5 days. Serious Wound Infections Most wound infections are easily acknowledged and could be treated in the outpatient setting with oral antibiotics, suture removing, evaluation for a retained overseas physique, and a follow-up examination inside a few days. Consider inpatient remedy for a patient with systemic complaints (fever, malaise, nausea), worsening an infection at follow-up, an unreliable affected person, or an immunocompromised patient. Some infections, similar to a subgaleal an infection in a scalp laceration, could be critical and will require immediate, aggressive remedy. Digital Nerves Numbness in the space of digital innervation, concomitant injury to a digital artery (flash, pulsating bleeding), or an electrical shock sensation when exploring a laceration should alert the clinician to a attainable digital nerve harm.
Order tegretol mastercardViral vesicles typically involve the digits however can also contain other areas of the hand spasms under ribs discount 100mg tegretol overnight delivery. Drainage of herpetic whitlow is contraindicated as it could induce a secondary bacterial an infection and delay therapeutic. Oral antiviral agents effective in opposition to herpes infections (acyclovir, famciclovir, or valacyclovir) can shorten the course of the disease if given early. Infection recurs in 30% to 50% of instances, but the preliminary an infection is usually the most severe. Acyclovir, 200 mg taken orally three to four instances a day, can decrease recurrence charges. An occlusive dressing decreases the possibility of viral transmission, but health care suppliers with herpetic whitlow should restrict and even perhaps chorus from affected person contact, especially till all lesions have crusted over and viral shedding has stopped. An important anatomic characteristic of this space is that many fibrous septa lengthen from the volar skin of the fat pad to the periosteum of the phalanx; these septa subdivide and compartmentalize the pulp area. When an infection occurs in the pulp, these buildings make it a closed-space an infection. The septa limit swelling, delay pointing of the abscess, and inhibit drainage after incomplete surgical decompression. The distal phalanx was almost completely resorbed due to pressure, irritation, and continual osteomyelitis. The an infection can progress to osteomyelitis of the distal phalanx, septic arthritis, and flexor tenosynovitis. Although the septa could facilitate an an infection in the pulp, additionally they provide a barrier that protects the joint house and tendon sheath by limiting proximal unfold of the infection. A affected person in whom a felon is developing will describe a gradual onset of pain and tenderness of the fingertip. In a couple of days, the ache turns into constant and throbbing and steadily becomes severe. In the preliminary phases, physical examination could additionally be fairly unimpressive as a end result of the fibrous septa limit swelling within the closed pulp area. Occasionally, one may elicit level tenderness, however frequently, the whole pulp house is extremely tender. The affected person characteristically arrives with the hand elevated over the pinnacle as a outcome of the ache is so intense within the dependent place. During the early stages of cellulitis, a felon may be managed by therapy consisting of elevation, oral antibiotics (see Box 37. A minor felon can usually be drained on an outpatient foundation after the application of a digital nerve block. Surgical drainage should be carried out rigorously to avoid damage to nerves, vessels, and flexor tendons. Most felons can be managed with a restricted process, but many surgical choices have been advocated, none of which has been proved to be superior for all circumstances. The most well-liked preliminary therapy is a straightforward longitudinal incision over the realm of best fluctuance,194,195 3 to 5 mm distal to the distal interphalangeal joint. Frank pus may be encountered throughout incision, but usually only a few drops are expressed. A potential drawback to an incision in the course of the fat pad is the manufacturing of a scar in a very sensitive and commonly traumatized area. The incision should not prolong to the distal interphalangeal crease due to the danger of injuring the flexor tendon. The subcutaneous tissue is bluntly dissected with a hemostat to present adequate drainage. A gauze pack may be positioned in the wound for 24 to 48 hours to ensure continued drainage. Recurrent or extra extreme infections may require a more aggressive approach by a hand specialist. Follow-up suggestions for patients with a analysis of felon should embrace referral to a hand surgeon. No matter which incision is made, it should not be carried proximal to the closed pulp space due to the danger of entrance into the tendon sheath or the joint capsule. A comfortable dressing, splinting, elevation, and adequate opioid analgesics are prerequisites for a profitable end result. On the first postoperative visit, perform a digital block and remove the packing if current. Irrigate the incision copiously with saline and remove any extra necrotic tissue. At the first revisit, check the sensitivities of the bacterial cultures and decide to proceed or change antibiotics. Some clinicians advocate radiographic evaluation for retained foreign our bodies on the initial go to, in addition to a baseline evaluation of the bone for subsequent evaluation of osteomyelitis. Other clinicians reserve radiographs for wounds not displaying vital enchancment in 5 to 7 days. Evidence of osteomyelitis, nonetheless, will not be discovered radiographically for a quantity of weeks after the appearance of the lesion. After adequate drainage, osteomyelitis may reply surprisingly nicely to outpatient antibiotic therapy, with nearly complete regeneration of bone being achieved if the I&D process has been enough. A fat pad incision is mostly avoided but can be acceptable for localized infections. The transverse fat pad incision ought to avoid the digital nerves (2), and the longitudinal fat pad incision should keep away from the flexor tendon (3). The eponychium is lifted, which resulted in immediate drainage of enormous quantities of pus. A hemostat is used to break up loculations in the fats pad after which to seize gauze for a pull-through pack. The gauze pack is pulled via the incision and left in place for 24 to forty eight hours to ensure continued drainage. For a felon the authors favor the through-and-through drainage procedure proven in B. Culture can aid within the choice of long-term antibiotics, but most initially cover for community-acquired methicillin-resistant Staphylococcus aureus. In this example, blood accrued solely underneath the nail, not in any paronychial areas. B, Subungual hematoma of the nice toe after dropping a heavy object on the foot (a widespread injury). Subungual Hematoma Subungual hematomas are sometimes attributable to hitting a fingertip with a hammer, slamming a finger in a door. Patients present with horrible throbbing pain that increases with the strain under the nail. There is an associated blue-black discoloration underneath the affected nail, indicative of the hematoma.
References - Sarris WH, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes. Rev. 2003;4:101-114.
- Markman M, Liu PY, Moon J, et al. Impact on survival of 12 versus 3 monthly cycles of paclitaxel (175 mg/m2) administered to patients with advanced ovarian cancer who attained a complete response to primary platinumpaclitaxel: follow-up of a Southwest Oncology Group and Gynecologic Oncology Group phase 3 trial. Gynecol Oncol 2009;114(2):195-198.
- Gabbe BJ, Sutherland AM, Wolfe R, et al. Can the modified Functional Independence Measure be reliably obtained from the patient medical record by different raters? J Trauma 2007;63: 1374-9.
- Quinn JV, Osmond MH, Yrack JA, et al: N-2-Butylcyanoacrylate: risk of bacterial contamination with an appraisal of its antimicrobial effects. J Emerg Med 13:581-585, 1995.
|

