|
Mayank V. Patel, MD - Department of Surgery
- Our Lady of Mercy Medical Center
- Westchester Square Medical Center
- Bronx, New York
Arava dosages: 20 mg, 10 mg
Arava packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills

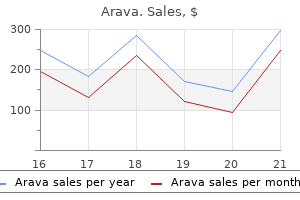
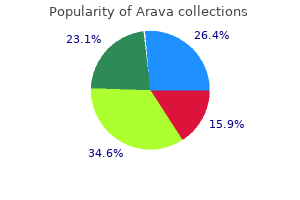
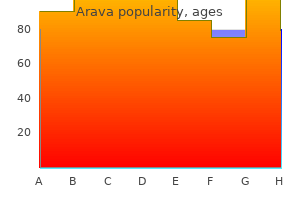
Order arava canadaLoaded pelvic colon could press upon the left testicular vein and stop its proper drainage medications while pregnant buy arava toronto. Ischioanal abscess: It is frequent as ischioanal fossae are situated on the two sides of the anal canal, deep to the pores and skin of perineum. The perianal area is located between ischial tuberosity and subcutaneous part of sphincter ani externus. Pudendal nerve block: this is an anaesthetic process used during vaginal deliveries or forceps supply. The pudendal nerve is the nerve of perineum and after anaesthesia, the vaginal delivery becomes nearly painless. Anteriorly by lesser omentum containing hepatic artery, portal vein and bile duct three. For each of the statements or questions beneath, a quantity of solutions given is/are appropriate. Superior and inferior layers of coronary ligaments, inferior vena cava and right triangular ligament 5. Introduction Nervous system is the chief controlling and coordinating system of the physique. It adjusts the body to the surroundings and regulates all bodily activities both voluntary and involuntary. The sensory a part of the nervous system collects information from the surroundings and helps in gaining information and experience, whereas the motor half is liable for responses of the body. Since brain floats in cerebrospinal fluid, it only weighs 50 grams which is comfortable. Autonomic nervous system for management of heart, clean muscle of the organs, glands and blood vessels. Classification of Neurons According to the Number of their Processes Each neuron is made up of the following. The impulses can move in them with great rapidity, in some instances about one hundred twenty five meters per 1 Multipolar neurons. According to Length of Axon 1 Golgi Type I: these neurons have long axons and numerous quick dendrites. Recently some neurons in olfactory region and hippocampus have been seen to divide. These somatic motor neurons are of two sorts: 1 Upper motor neurons are located in motor space of mind. Nerves Neurons are classified into sensory neurons, motor neurons and autonomic neurons, i. Sympathetic neurons (autonomic) 1 Preganglionic neurons are located in the lateral horn of thoracic one to lumbar two segments of the spinal cord. One cell may establish such contacts by way of its dendrites with as many as a thousand axonal terminals. The impulse is transmitted across a synapse via biochemical neurotransmitters (acetylcholine). A spontaneous gliosis is a sign of a degenerative change in the nervous tissue. Grey matter is the part of nervous tissue containing the cell body (soma), neuroglial cells and abundance of blood vessels. In advanced forms of the reflex arc, the internuncial neurons (interneurons) are interposed between the sensory and motor neurons. An involuntary motor response to a sensory stimulus is called the reflex motion. The spinal cord receives sensory information from the pores and skin, joints, and muscles of the trunk and limbs and contains the motor neurons liable for both voluntary and reflex movements. It also receives sensory data from the interior organs and control many visceral capabilities. In addition, the spinal cord contains ascending pathway by way of which sensory info reaches the mind and descending pathways that relay motor command from the mind Table 1. The pons: It lies rostral to the medulla and contains a lot of neurons that relay information from the cerebral hemispheres to the cerebellum. The midbrain: this is the smallest brainstem element which lies rostral to the pons. Several regions of this construction play an important role within the direct management of eye motion, whereas others are concerned in motor control of skeletal muscle tissue. The cerebellum receives somatosensory enter from the spinal wire, motor info from the cerebral cortex and stability data from the vestibular organs of the inner ear. The cerebellum integrates this information and coordinates the planning, timing and patterning of skeletal muscle contractions during movement. The cerebellum performs a major role within the management of tone, equilibrium and posture, including head and eye movements. It regulates levels of awareness and some emotional elements of sensory experiences. The hypothalamus lies ventral to the thalamus and regulates autonomic activity and the hormonal secretion by the pituitary gland. It consists of the cerebral cortex/grey matter and the fibres which kind white matter with deeply located nuclei: the basal ganglia, the hippocampal formation and the amygdala. The cerebral hemispheres are divided by the hemispheric fissure and are thought to be involved with perception, cognition, emotion, reminiscence and excessive motor features. Each hemisphere has a flat medial floor which lie adjoining to each other separated by a longitudinal fissure. In the decrease part of the fissure is present a thick band of fibres-the corpus callosum. The hemisphere reveals infoldings within the form of sulci and gyri, giving more space for the neurons. The outermost is the dura mater, center layer is delicate cobweb-like arachnoid mater and the inner one is the pia mater. The subdural area could be very slim whereas the subarachnoid house is massive containing crucial cerebrospinal fluid. Lastly mind and spinal twine with their meninges are securely kept within the bony cranium and vertebral canal, respectively. Such types of endings are present in connective tissue, dermis of pores and skin, fasciae, tendons, ligaments, joints, capsules, peritoneum, perichondrium and sheaths of blood vessels. Merkel (Disc Shaped) Endings Tumours of the nervous tissue arise largely from the neuroglia, as developed neurons have lost the power of multiplication besides in a few areas. The nerve fibres of these constructions broaden right into a disc applied carefully to the base of a specialised non-nervous cell (the Merkel cell) which is inserted into the basal cells of epithelium of the dermis. Dermis � Tactile corpuscles of Meissner: these are discovered in the dermal papillae of pores and skin of hand, ft, front of forearm, lips and mucous membrane of tip of tongue. They are cylindrical in form with lengthy axis perpendicular to deep floor of dermis and are about eighty m long and 30 m broad.
Arava 20 mg on lineThe stability of the joints depends on ligaments: palmar medicine holder generic arava 20 mg otc, dorsal and interosseous. Flexion (flexor carpi radialis and ulnaris aided by the long digital flexors) is bigger than extension (extensor carpi ulnaris and radialis longus and bre- vis assisted by the long digital extensors). Adduction (extensor and flexor carpi ulnaris) is bigger than abduction (flexor carpi radialis and extensor carpi radialis longus and brevis). Proximal to this the radial artery could be readily palpated because it lies on the radius. Medial to this are the tendons of flexor carpi radialis and palmaris longus, and beneath the latter the median nerve crosses the joint deep to the retinaculum. Lying centrally on a deeper airplane are the tendons of flexor digitorum superficialis and profundus and flexor pollicis longus. The form of the articular surfaces ensures that flexion is at all times accompanied by medial rotation, and extension by lateral rotation. One of essentially the most specific thumb actions is that of opposition, by which the tip of the thumb is introduced into contact with the tips of the fingers. It requires a mix of flexion, medial rotation and adduction of the thumb, and could be very a lot a human attribute: the carpometacarpal joints of the fingers are synovial plane joints. The second and third are less cell than the fourth and fifth, and all are much less mobile than that of the thumb; the metacarpal heads articulate with the cupped bases of the proximal phalanges. Superficial veins and cutaneous nerves lie within the superficial fascia, the terminal branches of the radial nerve crossing the tendon of abductor pollicis longus. Beneath it move the lengthy extensor tendons and their synovial sheaths, every being retained by fibrous septae inside fibro-osseous tunnels. Flexion/medial rotation � flexor pollicis longus and brevis and opponens pollicis Extension/lateral rotation � abductor pollicis longus and extensor pollicis longus and brevis Abduction � abductor pollicis longus and brevis Adduction � adductor pollicis Opposition � opponens pollicis. The metacarpophalangeal joints the metacarpophalangeal joints are synovial joints, the metacarpal heads articulating with the cupped bases of the proximal phalanges. Flexion, extension, abduction and adduction and circumduction are attainable, apart from the thumb, whose metacarpophalangeal joint is proscribed to flexion and extension: Flexion � long digital flexors and flexor pollicis longus, assisted by the interossei, lumbricals, flexor pollicis brevis and flexor digiti minimi Extension � within the fingers, extensor digitorum, extensor indicis and extensor digiti minimi; in the thumb, extensor pollicis longus and brevis Abduction � in the fingers, the dorsal interossei and abductor digiti minimi; within the thumb, abductor pollicis longus and brevis Adduction � palmar interossei and adductor pollicis. Its proximal apex is steady with the flexor retinaculum and receives the attachment of the tendon of palmaris longus; distally its base divides into four digital slips, which bifurcate across the long flexor tendons to be hooked up to the deep transverse ligaments of the palm. Its cause is unknown, however it results in shortening and thickening of the digital bands, which then pull the fingers into flexion, especially the ring and little fingers. Eventually the metacarpophalangeal and proximal interphalangeal joints turn out to be completely flexed. Thenar and hypothenar muscular tissues come up from its superficial floor, and the ulnar artery and nerve and its palmar branches cross it. Beneath it the carpal tunnel conveys the long flexor tendons, the radial and ulnar bursae and the median nerve and its digital branches. Whenever the dimensions of the tunnel is decreased, as it could be following the tissue swelling of rheumatoid arthritis or pregnancy, symptoms are produced by compression of the median nerve deep to the retinaculum (carpal tunnel syndrome). Compression of its cutaneous digital branches produces pain, tingling (paraesthesia) and anaesthesia over the lateral 3� digits. If the motor branches are affected then weakness, eventual paralysis and wasting of those small muscles of the hand provided by the median nerve results. There will be progressive loss of coordination and energy in the thumb, and a lack of muscle bulk in the thenar eminence may be famous. The tendons are confined within osseofascial tunnels that arch over the tendons and are hooked up to the sides of the phalanges. These potential fascial spaces might turn into infected, either by direct trauma from a puncture wound or by spread from a tendon sheath infection, and in these circumstances the infection can spread proximally deep to the flexor retinaculum to attain the lower forearm. The thick palmar fascia normally prevents the indicators of an infection showing in the palm. The painful swelling is mostly most evident on the dorsum the place the fascia is thinner. It is attached to the scaphoid and adjoining flexor retinaculum, and its tendon passes to the radial facet of the base of the proximal phalanx of the thumb. Opponens pollicis is hooked up proximally to the trapezium and adjacent flexor retinaculum and distally to the radial aspect of the 1st metacarpal. It flexes, adducts and medially rotates the thumb (otherwise known as opposing the thumb) to convey the pulp of the thumb tip into contact with the tips of the flexed fingers. The hypothenar muscles are small mirror photographs of the thenar muscular tissues and are equipped by the deep department of the ulnar nerve. They every come up from the medial aspect of the flexor retinaculum and pisiform or hamate bones. Abductor digiti minimi and flexor digiti minimi acquire distal attachment to the bottom of the proximal phalanx of the little finger; opponens digiti minimi is attached distally to the ulnar margin of the 5 metacarpal shaft. Proximally these are attached to the shafts of the metacarpals: the palmar to the palmar surfaces of the 1, 2, 4 and 5 bones; the bigger, more powerful dorsal muscular tissues are connected by two heads to adjacent metacarpals. Both groups, acting with the lumbricals, flex the proximal phalanx and, by their attachment to the extensor growth, help to prolong the middle and distal phalanges. Each is hooked up distally to the radial aspect of the extensor growth of its tendon. The two lateral lumbricals are provided by the median nerve, the two medial by the ulnar nerve. The power grip includes the long finger flexors and intrinsic flexors of the 4 fingers, locked down and reinforced by thumb flexion and adduction. A precision grip is far more a mix of mainly the interossei and lumbricals with help from the thenar and hypothenar opponens. The superficial palmar branch of the ulnar artery passes laterally deep to the palmar aponeurosis to be a part of the terminal department of the radial artery superficial to the long flexor tendons. It provides 4 palmar digital branches which, by bifurcating, supply adjacent sides of the fingers and also be part of with the deep palmar arch, another anastomosis, shaped largely by the radial artery and a smaller branch from the ulnar artery. It lies deep to the long flexor tendons and offers palmar metacarpal arteries and perforating arteries to the dorsum of the hand. Upper limb sensory testing (with eyes closed) of dermatomes and individual nerves Lumbricals (a) Touch (cotton wool); ache (sterile needle); temperature (side of finger versus chilly side of tuning fork); vibration (base of tuning fork on head of ulna); graphaesthesia (writing numbers on the forearm with a blunt instrument); stereognosis (recognizing a coin by touch); place sense (recognizing direction of motion � hold the perimeters of the index finger). Motor testing Power (grip); tone (passive flexion and extension of a relaxed elbow joint); coordination (finger to tip of nostril � eyes open after which closed); reflexes (biceps C5/6; supinator, triceps C6/7); observe wasting and abnormal movements; individual muscle tissue � active and passive actions, and towards resistance. They extend the interphalangeal joints by traction on the extensor tendons and flex the metacarpophalangeal joints by releasing tension within the digital aspect of the lengthy flexor tendons. Wrist-drop and sensory loss over the radial aspect of the palm and lateral fingers outcome. In the forearm, superficial injuries cause no extra than a small area of diminished sensation over the radial facet of the dorsum of the hand because the radial nerve incorporates no muscular branches. Deeper forearm accidents or fractures of the radial neck may damage the posterior interosseous nerve and end in incapability to prolong the thumb and the metacarpophalangeal joints of the fingers, because of the paralysis of the long extensors. Extension of the wrist is maintained as a end result of extensor carpi radialis is supplied by a department of the radial nerve that arises above the elbow. The consequent pull of the lengthy digital extensors produces hyperextension of the metacarpophalangeal joints.
Syndromes - Nausea or headache occur with the eye pain (this may be a symptom of glaucoma or stroke)
- Dimpling of the sacral area
- Electromyography (EMG)
- Decreased beard and body hair
- A cough with shortness of breath
- Convulsions
- You are a woman and your menstrual cycles are irregular
- Phenylalanine
- You have a stress fracture
Order arava cheapIdentify the broad ligament attaching uterus to the lateral pelvic wall and note varied structures present in its borders and surfaces useless id symptoms purchase arava 20mg visa. Definition � Determination of ovulation: In cases of sterility, the ovulation could be decided by repeated ultrasonography. Multiple small theca lutein cysts involve each the ovaries in circumstances with Stein-Leventhal syndrome. The syndrome is characterised by delicate hirsutism, deep voice, secondary amenorrhoea, and cystic enlargement of both the ovaries. Make a median dorsal reduce with a saw through the fourth and fifth lumbar vertebrae, the sacrum and coccyx to meet the knife. Separate the two halves of the pelvis and look at the cut surface of all the tissues. Identify the ovarian vessels within the infundibulopelvic ligament and trace these to the ovary and uterine tube. Identify the uterus and observe the peritoneum on its superior and inferior surfaces which is thus free to move. Trace the uterus downwards until the supravaginal part of cervix which is hooked up to the lateral pelvic wall by transverse cervical ligaments and to the sacrum by uterosacral ligaments. The posterior fornix is the They are tortuous ducts which convey oocyte from the ovary to the uterus. Spermatozoa launched into the vagina pass up into the uterus, and from there into the uterine tubes. Situation these are situated within the free upper margin of the broad ligament of uterus. At the lateral end, the uterine tube opens into the peritoneal cavity by way of its belly ostium. Subdivisions Section 1 the lateral end of the uterine tube is shaped like a funnel and is, therefore, known as the infundibulum. It bears a number of finger-like processes called fimbriae and is, therefore, called the fimbriated finish. One of the fimbriae is longer than the others and is connected to the tubal pole of the ovary. It is thin-walled, dilated and tortuous, and forms roughly the lateral two-thirds or 6 to 7 cm of the tube. Course and Relations 2 Abdomen and Pelvis 1 the isthmus and the adjoining a half of the ampulla are directed posterolaterally in a horizontal aircraft. It incorporates the termination of the uterine and ovarian vessels and the epoophoron. Blood Supply splanchnic nerves from S2�4 segments of spinal twine for the medial half. Lymphatic Drainage Most of the tubal lymphatics join the lymphatics from the ovary and drain with them into the lateral aortic and preaortic nodes. The lymphatics from the isthmus accompany the round ligament of the uterus and drain into the superficial inguinal nodes. Nerve Supply the uterine tubes are equipped by each the sympathetic and parasympathetic nerves running along the uterine and ovarian arteries. The mucous membrane is thrown into complicated folds which refill the lumen of the tube. Normally, air pushed into the uterus passes via the tubes and leaks into the peritoneal cavity. This leakage produces a hissing or effervescent sound which could be auscultated over the iliac fossae. The ciliary movements create an effective stream of lymph in the course of the uterus which assists in the nourishment of ovum in the lumen of the tube over the mucosal ridges. It is the organ which protects and provides diet to a fertilised ovum, enabling it to grow into a totally fashioned foetus. At the time of childbirth or parturition, contractions of muscle in the wall of the organ lead to expulsion of the foetus from the uterus. It is divisible into an higher expanded half referred to as the body and a decrease cylindrical half referred to as the cervix. The junction of those two components is marked by a round constriction referred to as the isthmus. The physique varieties the upper two-thirds of the organ, and the cervix forms the lower one-third. The superolateral angle of the physique project outwards on the junction of body and fundus and known as cornua of uterus. The uterine tube, ligament of ovary and round ligament are connected to it on all sides. Normally, the lengthy axis of the uterus types an angle of about 90� with the long axis of the vagina. The uterus can also be barely flexed at the level of internal os of cervix; that is referred to as anteflexion. The anterior or vesical floor of the body is flat and associated to the urinary bladder. It is covered with peritoneum and types the posterior or superior wall of the uterovesical pouch. The posterior or intestinal floor is convex and is related to coils of the terminal ileum and to the sigmoid colon. It offers attachment to the broad ligament of the uterus which connects it to the lateral pelvic wall. This finish of the border gives attachment to the round ligament of the uterus, anteroinferior to the tube; and to the ligament of the ovary posteroinferior to the tube. In sagittal part, the cavity of the body of the uterus is seen as a mere slit because the uterus is compressed anteroposteriorly. Cervix of Uterus Abdomen and Pelvis the cervix is the decrease, cylindrical a half of the uterus. The decrease a half of the cervix initiatives into the anterior wall of the vagina which divides it into supravaginal and vaginal elements. The fibrofatty tissue between the two layers of the broad ligament and below it, is called the parametrium. However, in multiparous ladies, the exterior os is bounded by anterior and posterior lips, both of that are in contact with the posterior wall of the vagina. It communicates above with the cavity of the physique of the uterus, by way of the internal os, and under with the vaginal cavity through the external os. The canal is flattened from earlier than backwards so that it comes to have anterior and posterior partitions. These partitions present mucosal folds which resemble the branches of a tree called the arbor vitae uteri.
Order arava 20mg overnight deliveryIt has: Two ends-upper and lower; Three borders-anterior treatment goals for ptsd order 20 mg arava with visa, posterior and lateral; Three surfaces-femoral, dorsal and pelvic. Borders Lower Limb 1 the anterior border forms the posterior margin of the obturator foramen. Below the spine the posterior border shows a concavity, called the lesser sciatic notch. From above downwards, it presents a convex surface adjoining the acetabulum, a large shallow groove, and the upper a half of the ischial tuberosity. The ischial tuberosity is divided by a transverse ridge into an upper and a lower area. The higher space is subdivided by an oblique ridge right into a superolateral space and an inferomedial area. Conjoined Ischiopubic Rami the inferior ramus of the pubis unites with the ramus of the ischium on the medial aspect of the obturator foramen. The conjoined rami have: Borders: Upper and lower 1 the upper border forms part of the margin of the obturator foramen. It is lined with hyaline cartilage, and articulates with the top of the femur to form the hip joint. The fibrocartilaginous acetabular labrum is hooked up to the margins of the acetabulum; it deepens the acetabular cavity. The secondary centres seem at puberty, two for the iliac crest, two for the Y-shaped cartilage of the acetabulum and one for the ischial tuberosity. Neck � Iliac crest is used for taking bone marrow biopsy in cases of anemia or leukemia. Femur has an higher rounded finish; a decrease bicondylar end and a long shaft which is convex forwards. Side Determination Anatomical Position 1 the top is directed medially upwards and slightly forwards. Section the higher end of the femur includes the head, the neck, the greater trochanter (Greek runner) the lesser trochanter, the intertrochanteric line, and the intertrochanteric crest. Greater Trochanter 1 this can be a large quadrangular prominence situated on the higher a part of the junction of neck with the shaft. The apex is the inturned posterior part of the posterior 1 Lower Limb 1 the higher end bears a rounded head whereas the decrease end is broadly expanded to type two giant condyles. The higher border, concave and horizontal, meets the shaft on the higher trochanter. The lower border, straight and oblique, meets the shaft near the lesser trochanter. The posterior floor is convex from above downwards and concave from side to aspect. The posterior floor is crossed by a horizontal groove for the tendon of the obturator externus to be inserted into the trochanteric fossa. It is strengthened by a thickening of bone referred to as the calcar femorale current along its concavity. It is a vital radiological parameter which offers the idea of course of medullary canal and its alignment with the greater trochanter. The vessels produce longitudinal grooves and foramina directed in the course of the head, primarily on the anterior and posterosuperior surfaces. The medial floor presents a tough impression above, and a deep trochanteric fossa under. Lesser Trochanter ridge which begins above, at the anterosuperior angle of the higher trochanter as a tubercle, and is steady beneath with the spiral line in front of the lesser trochanter. The spiral line winds round the shaft under the lesser trochanter to attain the posterior surface of the shaft. Intertrochanteric Crest Section It is a conical eminence directed medially and backwards from the junction of the posteroinferior part of the neck with the shaft. Intertrochanteric Line 1 It marks the junction of the anterior floor of the neck with the shaft of the femur. It is a distinguished roughened It marks the junction of the posterior surface of the neck with the shaft of the femur. It is a smooth-rounded ridge, which begins above at the posterosuperior angle of the larger trochanter and ends at the lesser trochanter. It is convex forwards and is directed obliquely downwards and medially, as a result of the upper ends of two femora are separated by the width of the pelvis, and their decrease ends are shut together. In the middle one-third, the shaft has three borders- medial, lateral and posterior and three surfaces- anterior, medial and lateral. The medial and lateral borders are rounded and ill-defined, however the posterior border is in the type of a broad roughened ridge, referred to as the linea aspera (Latin tough line). The medial and lateral surfaces are directed more backwards than in course of the sides. In the upper one-third of the shaft, the 2 lips of the linea aspera diverge to enclose a further posterior floor. The gluteal tuberosity is a broad roughened ridge on the lateral a half of the posterior surface. Thus, this part of the shaft has: Four borders-medial, lateral, medial supracondylar line and lateral supracondylar line. The medial border and medial supracondylar line meet inferiorly to obliterate the medial floor. Similarly the lateral border and lateral supracondylar line also meet inferiorly to obliterate the lateral floor. The tibial surfaces cowl the inferior and posterior surfaces of the two condyles, and merge anteriorly with the patellar floor. The a part of the surface over the lateral condyle is brief and straight anteroposteriorly. Lateral Condyle the lateral condyle is flat laterally, and is more consistent with the shaft. Intercondylar Fossa or Intercondylar Notch this notch separates the lower and posterior components of the two condyles. It is limited anteriorly by the patellar articular surface, and posteriorly by the intercondylar line which separates the notch from the popliteal floor. Attachments on the Femur the lower end of the femur is widely expanded to type two large condyles, one medial and one lateral. Anteriorly, the two condyles are united and are in line with the front of the shaft. Articular Surface the two condyles are partially lined by a large articular floor which is divisible into patellar and tibial parts. The clean posterior surface of the lesser trochanter is roofed by a bursa that lies deep to the higher horizontal fibres of the adductor magnus. The medial and popliteal surfaces are bare, apart from slightly extension of the origin of the medial head of the gastrocnemius to the medial part of popliteal surface.
Purchase arava lineLower a half of the inferior ramus of the pubis Into the groove on the posterior surface of the medial condyle of the tibia treatment whooping cough order arava with american express. Weak extensor of the hip Chief flexor of the knee and medial rotator of the leg in semiflexed knee. Weak extensor of the hip Chief flexor of the knee and lateral rotator of leg in semiflexed knee. Weak extensor of the hip Adductor half causes adduction of thigh; Ischial part helps in extension of hip and flexion of knee 2. Course and Relations 1 In the pelvis: the nerve lies in entrance of the piriformis, beneath cowl of its fascia. It runs downwards with a slight lateral convexity, passing between the ischial tuberosity and the higher trochanter. It runs vertically downwards as much as the superior angle of the popliteal fossa, on the junction of the higher two-thirds and lower one-third of the thigh, where it terminates by dividing into the tibial and the frequent peroneal nerves. It begins in the pelvis and terminates on the superior angle of the popliteal fossa by dividing into the tibial and common peroneal nerves. The sciatic nerve is accompanied by a small companion artery-arteria nervi ischiadici. Branches Lower Limb 1 Articular branches to the hip joint come up within the gluteal region. When a person sits on the edge of a hard table/chair, the nerve gets compressed between the sting of table and femur. Pain often begins in the gluteal area, and radiates alongside the back of the thigh, and the lateral aspect of the leg, to the dorsum of the foot. This is often because of compression of a number of nerve roots forming the sciatic nerve. The lateral circumflex femoral department of the profunda femoris divides into ascending, transverse and descending branches. The main supply to the back of the thigh is through the perforating branches of the profunda femoris. Perforating Branches of the Profunda Femoris Artery Section the profunda femoris artery provides off four perforating arteries. These longitudinal anastomotic chains are formed by the branches of inner iliac, the femoral and popliteal arteries. This is formed by the companion artery of the sciatic nerve and the perforating arteries. These longitudinal anastomoses provide an alternate route of blood provide to the lower limb, bypassing the exterior iliac and femoral arteries. The pain on the again of thigh signifies compression of the roots of sciatic and radiating ache alongside cutaneous branches of tibial and common peroneal nerves. Tibial collateral ligament of knee is the morphological continuation of which muscle Section 1 Front of Leg with Dorsum of Foot; Lateral and Medial Sides of Leg -V Nabokov 8 Human life is however a series of footnotes to a vast obscure unfinished masterpiece. Dorsalis pedis artery, the distal continuation of the anterior tibial artery, is used for palpation in some medical circumstances. The dorsiflexors of foot equipped by deep peroneal nerve lie in the anterior compartment of leg. The two huge evertors of the foot with superficial peroneal nerve are placed in the lateral compartment of the leg. The tendons of all these muscle tissue are retained in position by two extensors and two peroneal retinacula. The tuberosity provides attachment to ligamentum patellae above, and is continuous with the shin below. It serves as a information to common peroneal nerve which winds across the posterolateral aspect of the neck of fibula. It is sinuously curved and extends from the tibial tuberosity to the anterior margin of the medial malleolus. Great saphenous vein crosses lower one-third of the surface, running obliquely upwards and backwards from the anterior border of medial malleolus. The posterior borders of two malleoli are in the same coronal aircraft, however the anterior border of lateral malleolus is about 1. It pierces the deep fascia on the medial side of the knee between the sartorius and the gracilis, and runs downwards in front of the good saphenous vein. It provides the pores and skin of the medial aspect of the leg and the medial border of the foot up to the ball of the good toe. It arises on the lateral aspect of the neck of the fibula deep to the fibres of the peroneus longus. It descends between the peroneal muscle tissue, pierces the deep fascia on the junction of the higher two-thirds and lower one-third of the lateral facet of the leg, and divides into medial and lateral branches. The skin over the complete dorsum of the foot aside from the next areas. It passes upwards in entrance of the medial malleolus, crosses the decrease one-third of the medial surface of tibia obliquely, and runs alongside its medial border to attain the back of the knee. Both saphenous veins are linked to the deep veins through the perforating veins. Medial plantar nerve supplies medial 3� toes; lateral plantar nerve supplies lateral 1� toes. Provide a vertical incision up from the centre of incision (1) to the middle of incision drawn just under the extent of tibial tuberosity. Carry this vertical incision onto the dorsum of foot until the center of the second toe. The anterior and posterior intermuscular septa are connected to the anterior and posterior borders of the fibula. The posterior compartment is subdivided into superficial, intermediate and deep elements by superficial and deep transverse fascial septa. On the front of the ankle there are the superior and inferior extensor retinacula. The peroneal retinacula are thought of with the lateral compartment of the leg and the flexor retinaculum with the posterior compartment again of leg. Medially, it splits to enclose the tendon of tibialis anterior and its synovial sheath. Attachments 1 the stem is connected to the anterior non-articular part of the superior surface of the calcaneum, in entrance of the sulcus calcanei. Relations the stem of this retinaculum loops across the tendons of extensor digitorum longus and peroneus tertius including their synovial sheaths. The higher band encloses tendons of tibialis anterior and extensor hallucis longus with their synovial sheaths. Competency achievement: the student ought to be in a position to: the attachments of those muscles are given in Tables eight. Adjoining a half of interosseous membrane Insertion Inferomedial surface of the medial cuneiform and the adjoining part of the base of first metatarsal bone a. Posterior half of the center two-fourths of Dorsal surface of the base of the distal the medial floor of the shaft of the fibula, phalanx of the big toe medial to the extensor digitorum longus b.
Purchase 20 mg arava with visaMorphological divisions: Morphologically medicine 665 buy cheap arava line, the iliac crest is divided into a long ventral phase and a short dorsal segment. Anterior Border essentially the most ill-defined, begins somewhat above and behind the anterior inferior spine, runs backwards and downwards to end near the apex of the higher sciatic notch. Iliac Fossa Iliac fossa is the large concave space on the inner floor of the ilium, situated in entrance of its medial border. Sacropelvic Surface Anterior border begins on the anterior superior iliac backbone and runs downwards to the acetabulum. The upper a part of the border presents a notch, while its decrease part exhibits an elevated space called the anterior inferior iliac spine. Posterior Border Posterior border extends from the posterior superior iliac spine to the higher finish of the posterior border of the ischium. A few centimetres below the posterior superior iliac backbone, it presents one other prominence is called the posterior inferior iliac backbone. Medial Border Sacropelvic floor is the uneven area on the inside surface of the ilium, situated behind its medial border. It is subdivided into three parts-the iliac tuberosity, the auricular floor and the pelvic floor. The iliac tuberosity is the higher, large, roughened space, lying just below the dorsal segment of the iliac crest. Along the upper border of the higher sciatic notch, this floor is marked by the preauricular sulcus. Attachments 1 the anterior superior iliac spine gives attachment to the lateral finish of the inguinal ligament. Attachment to the fascia transversalis and to the fascia iliaca in its anterior two-thirds, deep to the attachment of the transversus abdominis. Lower Limb Section Medial border extends on the internal or pelvic floor of the ilium from the iliac crest to the iliopubic eminence. Gluteal Surface Gluteal floor is the outer floor of the ilium, which is convex in entrance and concave behind, just like the iliac crest. The posterior gluteal line, the shortest, begins 5 cm in entrance of the posterior superior iliac backbone, and runs downwards to finish at upper part of larger sciatic notch. The anterior gluteal line, the longest, begins about four cm behind the anterior superior iliac backbone, runs backwards after which downwards to finish on the middle of the higher border of the greater sciatic notch. Attachment to the thoracolumbar fascia across the attachment of the quadratus lumborum. The upper half of the anterior inferior iliac spine gives origin to the straight head of the rectus femoris. Attachment to upper fibres of the sacrotuberous ligament above the larger sciatic notch. The capsular ligament of the hip joint is hooked up alongside the margin of acetabulum. The convex margin of the auricular surface offers attachment to ventral sacroiliac ligament. The preauricular sulcus offers attachment to the decrease fibres of the ventral sacroiliac ligament. The a half of the pelvic surface lateral to the preauricular sulcus provides origin to a few fibres of the piriformis. Body Body of pubis is flattened from earlier than backwards, and has: 1 A superior border referred to as the pubic crest. It types the anterior wall of the true pelvis, and is said to the urinary bladder. The medial or symphyseal surface articulates with the opposite pubis to kind the pubic symphysis. Superior Ramus Inferior ramus extends from the body of the pubis to the ramus of the ischium, medial to the obturator foramen. For convenience of Section Inferior Ramus 1 Superior ramus extends from the body of the pubis to the acetabulum, above the obturator foramen. It is a sharp crest extending from simply behind the pubic tubercle to the posterior a part of the iliopubic eminence. The border is a rounded ridge, extending from the pubic tubercle to the acetabular notch. The pectineal floor is a triangular area between the anterior and superior borders, extending from the pubic tubercle to the iliopubic eminence. The lacunar ligament on the medial finish, in front of the attachment of the conjoint tendon. Origin to the gracilis, from the margin of symphysis, and from the inferior ramus. Attachment to the puboprostatic/pubovesical ligaments medial to the attachment of the levator ani. The ischium varieties the posteroinferior a half of the hip bone, and the adjoining two-fifths of the acetabulum. Body it is a thick and big mass of bone that lies below and behind the acetabulum. The deeper fibres of the decrease half of the gluteus maximus are inserted into the gluteal tuberosity. The adductor longus is inserted along the medial lip of the linea aspera between the vastus medialis and the adductors brevis and magnus. The pectineus is inserted on a line extending from the lesser trochanter to the linea aspera. The medial and lateral intermuscular septa are attached to the lips of the linea aspera and to the supracondylar lines. The infrapatellar synovial fold is connected to the anterior border of the intercondylar fossa. The popliteal floor is covered with fats and types the floor of the popliteal fossa. When the knee is flexed the tendon of this muscle lies within the shallow posterior a half of the groove. The anterior cruciate ligament is hooked up to the posterior part of the medial floor of the lateral condyle, on a easy impression. This is derived from the second perforating artery, department of profunda femoris artery. Structure the angles and curvatures of the femur are strengthened on their concave sides by bony buttresses. The concavity of the neck-shaft angle is strengthened by a thickened buttress of compact bone, known as the calcar femorale. The upper epiphyses; lesser trochanter, larger trochanter and head, in that order, fuse with the shaft at about eighteen years. The neck represents the higher finish of the shaft as a result of it ossifies from the primary centre.
Peruvian Rhatany (Rhatany). Arava. - What is Rhatany?
- Dosing considerations for Rhatany.
- Intestinal inflammation (enteritis), chest pain (angina), leg ulcers, mild mouth and throat irritation, and other conditions.
- How does Rhatany work?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96396
Buy online aravaThe hypothalamic sulcus symptoms e coli discount 20mg arava free shipping, extending from the interventricular foramen to the cerebral aqueduct, divides every half of the diencephalon into dorsal and ventral parts. The superior surface is divided into a lateral ventricular half which forms the ground of the central a part of the lateral ventricle, and a medial extraventricular half which is covered by the tela choroidea of the third ventricle by the free margin of physique of fornix. Measurements: � Anteroposterior-4 cm � Vertical-4 cm � Transverse-4 cm It has anterior and posterior ends; superior, inferior, medial and lateral surfaces. It overhangs the lateral and medial geniculate White matter the exterior medullary lamina covers the lateral surface. The inside medullary lamina divides the thalamus into three parts-anterior, medial and lateral. It is divided into the lateral nucleus in the dorsolateral part, and the ventral nucleus within the ventromedial part. The ventral nucleus is subdivided into anterior, intermediate and posterior groups. The posterior group is further subdivided into the posterolateral and posteromedial teams. Exteroceptive and proprioceptive impulses ascend to it by way of the medial lemniscus, the spinothalamic tracts and the trigeminothalamic tracts. Visceral info is conveyed from the hypothalamus and doubtless via the reticular formation. In addition to these afferents, the thalamus receives profuse connections from all components of the cerebral cortex, the cerebellum and the corpus striatum. The thalamus is, due to this fact, thought to be a fantastic integrating centre the place info from all these sources is introduced collectively. This data is projected to virtually the entire of the cerebral cortex through profuse thalamocortical projections. Efferent Brain�Neuroanatomy projections also attain the corpus striatum, the hypothalamus and the reticular formation. Besides its integrating operate, the thalamus has some extent of capability to perceive exteroceptive sensations, especially pain. Metathalamus (Part of Thalamus) the metathalamus consists of the medial and lateral geniculate our bodies, which are located on both sides of the midbrain, under the thalamus. Medial Geniculate Body It is an oval elevation situated just below the pulvinar of the thalamus and lateral to the superior colliculus. The inferior brachium connects the medial geniculate body to the inferior colliculus. Afferents (1) Lateral lemniscus, (2) fibres from each inferior colliculi, and (3) ascending reticular pathway and notion of painful and nociceptive stimuli. Function Medial geniculate body is the last relay station on the pathway of auditory impulses to the cerebral cortex and for notion of painful and nociceptive stimuli. Lateral Geniculate Body It is a small oval elevation situated anterolateral to the medial geniculate physique, below the thalamus. Efferents: It offers rise to optic radiations going to the visible space of cortex by way of retrolentiform part of inner capsule. Function Lateral geniculate physique is the last relay station on the visual pathway to the occipital cortex. The trigone is a small, depressed triangular area, located above the superior colliculus and medial to the pulvinar of the thalamus. Afferents � Hypothalamus � Amygdaloid physique � Hippocampus Efferents: To interpeduncular nucleus Functions: Acts as nodal level for convergence of basic emotional drives. The pineal (Latin pine, cone) body is a small, conical organ, projecting backwards and downwards between the two superior colliculi. It is positioned under the splenium of the corpus callosum, however is separated from it by the tela choroidea of the third ventricle. It consists of a conical physique about eight mm long, and a stalk or peduncle which divides anteriorly into two laminae separated by the pineal recess of the third ventricle. Morphological significance In many reptiles, the epiphysis cerebri is represented by a double construction. Brain�Neuroanatomy � Lesions of the thalamus cause impairment of all types of sensibilities; joint sense (posture and passive movements) being essentially the most affected. The vessels and nerves enter the gland by way of the connective tissue septa which partly separate the lobules. Calcareous concretions are constantly current within the pineal physique after the seventeenth 12 months of life and may form aggregations (brain sand). Functions the pineal physique has for lengthy been considered a vestigial organ of no significance. It produces hormones which will have an important regulatory affect on many other endocrine organs (including the adenohypophysis, the neurohypophysis, the thyroid, the parathyroids, the adrenal cortex and medulla, and the gonads). The finest identified hormone is melatonin which causes changes in pores and skin color in some species. The synthesis and discharge of melatonin is remarkably influenced by publicity of the animal to light and is more during darkish interval. Parts of the Hypothalamus the hypothalamus is subdivided into optic, tuberal and mammillary elements. The nuclei current in each half are as follows: Optic part 1 Preoptic and supraoptic nuclei. Tuberal half 4 Ventromedial nucleus 5 Dorsomedial nucleus 6 Tuberal nucleus-lateral to the ventromedial nucleus. Mammillary half eight Posterior nucleus-caudal to the ventromedial and dorsomedial nuclei and mammillary nucleus. The nuclei 3, four and 6 (medial) are separated from nuclei 5 and seven (lateral) by the column of the fornix, the mammillothalamic tract and the fasciculus retroflexus. It can also be related to several centres associated with olfactory pathways, together with the piriform cortex, cerebellum; and retina. Through its connections with the limbic system, it participates in the elementary drives associated with meals (hunger and thirst) and sex. Biological clocks Many tissues and organ-systems of the body show a cyclic variation of their functional activity during the 24 hours of a day (circadian rhythm). Sleep is produced by the hypnogenic zones, mainly of the thalamus and hypothalamus and partly by the brainstem. Lesions of the anterior hypothalamus seriously disturb the rhythm of sleep and wakefulness. Emotion, worry, rage, aversion, pleasure and reward these schools are managed by the hypothalamus, the limbic system and the prefrontal cortex. General autonomic effect the anterior elements of the hypothalamus mainly mediate parasympathetic activity; and the posterior parts, chiefly mediate sympathetic exercise, but the effects often overlap. Thus the hypothalamus controls cardiovascular, respiratory and alimentary functions. Temperature regulation the hypothalamus maintains a balance between warmth manufacturing and heat loss of the physique. Raised physique temperature is decreased via vasodilation, sweating, panting and lowered warmth production. Lowered physique temperature is elevated by shivering and in extended circumstances by hyperactivity of the thyroid.
Best arava 20 mgStatoacoustic nerve is afferent for listening to and steadiness whereas spinal root accent acts as its efferent component for turning the neck to the facet from the place sound is heard medicine 802 10mg arava mastercard. The mantle layer represents gray matter and the marginal layer represents the white matter. Soon the mantle layer differentiates right into a dorsal alar lamina (sensory) and a ventral basal lamina (motor), the two are partially separated internally by the sulcus limitans. The somatic columns are the final somatic efferent (motor or anterior horn) and the final somatic afferent (sensory or posterior horn). The visceral columns are the overall visceral efferent (motor) and the final visceral afferent (sensory). In the brainstem, significantly hindbrain, the alar and basal laminae come to lie in the same ventral airplane because of stretching of the roof plate (dorsal wall) of neural tube by pontine flexure. Further, the gray matter types separate longitudinal useful columns, where the motor columns (from basal lamina) are medial and the sensory columns (from alar lamina) are lateral in place. In addition to the four useful columns differentiated in the spinal twine, there seem two more columns (a motor and a sensory) for the branchial apparatus of the pinnacle region, specifically the special visceral (branchial) efferent and the particular visceral afferent; and one column more for the particular sense, particularly the special somatic afferent. Its fibres enter the oculomotor nerve and provide 4� extrinsic muscle tissue of the eyeball besides the lateral rectus and the superior oblique. It provides seven out of eight muscles of the tongue via the hypoglossal nerve. Special Visceral Efferent/Branchial Efferent Nuclei the small print of the nuclei of cranial nerves are summarized in Table 4. It forms an elongated column mendacity in both the open and closed elements of the medulla. General Visceral Efferent Nuclei these nuclei give origin to preganglionic neurons that relay in a peripheral autonomic ganglion. Its fibres pass through the oculomotor nerve to the ciliary ganglion to provide the sphincter pupillae and the ciliaris muscles. It gives off fibres that move through the facial nerve and its branch, the larger petrosal nerve to relay within the pterygopalatine ganglion and supply the lacrimal, nasal, palatal and pharyngeal glands. It sends fibres through the facial nerve and its chorda tympani branch to the submandibular ganglion for supply of the submandibular, sublingual salivary glands and glands in the oral cavity. It gives off fibres that cross by way of the vagus nerve to be distributed to thoracic and belly viscera (the ganglia involved are present in the partitions of the viscera supplied). Through the glossopharyngeal nerve from the tonsil, pharynx, posterior part of the tongue, carotid physique and carotid sinus. Through the vagus nerve from the pharynx, larynx, trachea, oesophagus and different thoracic and stomach viscera. Its upper half additionally receives sensations of style (special visceral afferent) as follows: a. From the posteriormost part of the tongue and from the epiglottis by way of the vagus (X) nerve in its inferior part. Exteroceptive sensations (touch, pain, temperature) from the skin of the face, through the trigeminal nerve; and from a part of the pores and skin of the auricle through the vagus (auricular branch) and thru the facial nerve. Proprioceptive sensations from muscle tissue of mastication attain the mesencephalic nucleus through the trigeminal nerve. The nucleus can additionally be believed to obtain proprioceptive fibres from the ocular, facial and lingual muscle tissue, enamel and temporomandibular joint. Special Features Muscles of facial expression of decrease quarter of the face are equipped only from contralateral motor cortex. The genioglossus muscle of the tongue receives fibres from contralateral motor cortex solely. Receptors and the First Neuron 1 the olfactory cells (16�20 million in man) are bipolar neurons. They lie in the olfactory part of the nasal mucosa, and serve both as receptors in addition to the first neurons within the olfactory pathway. They pass through the cribriform plate of ethmoid and make synaptic glomeruli with cells of olfactory bulb. Second Neuron the uncus and anterior part of the parahippocampal gyrus, tertiary olfactory cortex in posterior part of orbitofrontal cortex. The fibres attain the cerebral cortex without synapsing in any of the thalamic nuclei. These are situated within the main olfactory cortex which incorporates the anterior perforated substance, periamygdaloid and prepiriform areas. Third Neuron Third neuron positioned within the major olfactory cortex which includes the anterior perforated substance, and a quantity of other small lots of gray matter round it like periamygdaloid and prepiriform areas. Fourth Neuron Fibres arising in the primary olfactory cortex go to the secondary olfactory cortex (entorhinal area) located in � Anosmia: Loss of olfactory fibres with ageing. These suits are of imaginary unpleasant odours with involvement of tongue and lips. Right eye sees a little additional of right side whereas left eye sees a little additional of left side of the thing. Larger right temporal and smaller right nasal fields of vision fuse to kind right Brain�Neuroanatomy a part of binocular area. Retina is also divided into temporal and nasal parts and each is additional subdivided into upper and lower components. Fibres from the nasal components of the two retinae decussate to type the optic chiasma and journey to the contralateral aspect within the optic tract. Right optic tract carries the fibres of the right temporal hemiretina and the left nasal hemiretina and vice versa. Macular fibres lie within the central a part of optic tract, higher retinal fibres project downwards and decrease retinal fibres project upwards. Optic Nerve Optic nerve is made up of axons of ganglion cells of the retina which kind the second order neurons. A few of its fibres cross to the superior colliculus, the pretectal nucleus and the hypothalamus. Each optic tract contains temporal fibres of retina of the same facet and nasal fibres of the opposite side. Lateral Geniculate Body Lateral geniculate body receives the lateral root of the optic tract. The cells on this physique are organized in six layers which form the third order neurons. Layers 2, three, 5 receive ipsilateral fibres, and layers 1, 4, 6 receive contralateral fibres. Objects are recognized by integration of those perceptions with past expertise saved in the parastriate and peristriate areas 18 and 19. The space of the visible cortex that receives impulses from the macula is relatively much larger than the part associated to the remainder of the retina. It leads to swelling of optic disc because of blockage of tributaries of the retinal veins. To the pyramidal tracts of both sides which kind the supranuclear pathway of the nerve. To the fourth, sixth and eighth nerve nuclei by medial longitudinal bundle for coordination of the eye actions.
Arava 20mg low priceIt runs upwards on or instantly to the left of the aorta medications contraindicated in pregnancy buy arava 10mg with mastercard, as much as the upper border of the second lumbar vertebra, where it turns forwards to turn out to be continuous with the jejunum at the duodenojejunal flexure. The terminal part is suspended by the uppermost part of the mesentery, and is cell. Arterial Supply it is a fibromuscular band which suspends and supports the duodenojejunal flexure. The opening of the bile duct into the second part of the duodenum represents the junction of the foregut and the midgut. The supraduodenal artery of Wilkie, which is often a department of the frequent hepatic artery. From right here the lymph passes partly to the hepatic nodes, and through them to the coeliac nodes; and partly to the superior mesenteric nodes and finally through intestinal lymph trunk into the cisterna chyli. Some vessels from the primary part of the duodenum drain into the pyloric nodes, and through them to the hepatic nodes. The ulcer pain located at the proper half of epigastrium is relieved by meals and reappears on an empty stomach. They are seen alongside its concave border, typically at points where arteries enter the duodenal wall. The jejunum constitutes the upper two-fifths of the mobile part of the small intestine, while the ileum constitutes the decrease three-fifths. The construction and features of the jejunum and ileum correspond to the general description of the small gut. Blood Supply the jejunum and ileum are provided by branches from the superior mesenteric artery, and are drained by corresponding veins. Lymphatic Drainage Lymph from lacteals drains into plexuses in the wall of the gut. Passing by way of quite a few lymph nodes present within the mesentery, and along the superior mesenteric artery, it in the end drains into nodes current in front of the aorta on the origin of the superior mesenteric artery. Nerve Supply Sympathetic nerves are from T9 to T11 spinal segments and parasympathetic nerve is from vagus. Mesentery Jejunum Occupies higher and left parts of the intestinal area Thicker and extra vascular Wider and often empty a. Windows present Fat much less plentiful Arterial arcades, 1 or 2 Vasa recta longer and fewer Ileum Occupies decrease and proper elements of the intestinal area Thinner and less vascular Narrower and infrequently loaded a. No windows Fat more abundant Arterial arcades, three or 6 Vasa recta shorter and more numerous 2 5. Circular mucosal folds Larger and more closely set Large, thick (leaf-like) and extra plentiful Absent Fewer Smaller and sparse Shorter, thinner (finger-like) and fewer abundant Present More numerous Section Microscopic 6. Cut through the small intestine between each pair of ligatures and take away it by dividing the mesentery close to the intestine. Remove only the mucous membrane and submucosa to see the underlying circular muscle coat. The basic structure of enormous gut is taken into account first adopted by its elements one after the other. The construction of the large intestine is adapted for storage of matter reaching it from the small intestines, and for absorption of fluid and solutes from it. Adequate lubrication for passage of its contents is provided by numerous goblet cells scattered in the crypts in addition to on the surface of the mucous membrane. The presence of quite a few solitary lymphatic follicles supplies protection in opposition to micro organism current within the lumen of the intestine. Proximally, the taeniae converge at the base of the appendix, and distally they spread out on the terminal a part of the sigmoid colon, to turn into steady with the longitudinal muscle coat of the rectum. In the caecum, the ascending colon, the descending colon and sigmoid colon the positions of taeniae are anterior or taenia libera; posteromedial or taenia mesocolica and posterolateral or taenia omentalis, however in the transverse colon the corresponding positions of taenia are inferior, posterior and superior. One taenia, taenia libera, is placed anteriorly within the caecum, ascending, descending and sigmoid colon, but is placed inferiorly within the transverse colon. Third taenia, taenia omentalis, is situated posterolaterally in caecum, ascending, descending and sigmoid colon, however is located on the anterosuperior floor of transverse colon where layers three and four of greater omentum meet the transverse colon. These are most numerous on the edges of the sigmoid colon and on the posterior surface of the transverse colon. The variations between the small intestine and large gut are summarised in Table 20. Terminal branches from the marginal artery are distributed to the intestine as lengthy and quick vessels, vasa longa and vasa brevia. Fixity Small intestine Absent Absent Absent Less distensibility and fewer diameter Greater half is freely mobile Present Permanent Present in ileum a. Tuberculosis Diarrhoea Large intestine Present Present Present More distensibility and extra diameter Greater half is fastened Absent Obliterated when longitudinal muscle coat relaxes Absent a. Effects of infection and irritation serous and muscular coats and attain the amesocolic taeniae. Short branches come up either from the marginal artery or from the long branches, and the majority of them without delay sink into the bowel wall on the mesocolic border. The quick and lengthy branches together thus present the mesocolic area of the wall with ample blood provide. Subserous coat of lengthy branches is intimately associated to appendices epiploicae, to which they contribute branches. During removing of these appendages, care should be taken not to pull on them so as to avoid traction on the subjacent vessel. Mucosa might herniate in these situations inflicting diverticulosis, with related dangers of diverticulitis, fibrosis and stricture. Paracolic nodes, on the medial aspect of the ascending and descending colon and close to the mesocolic border of the transverse and sigmoid colon. In carcinoma of the colon, the related paracolic and intermediate lymph nodes should be removed. Their removing is possible only after the ligature of the primary department of the superior or inferior mesenteric artery alongside which the concerned lymph nodes lie. It is necessary, subsequently, to take away a large phase of the bowel than is actually required by the extent of the illness, to have the ability to keep away from gangrene on account of interference with the blood supply. It is at all times wise to remove the entire portion of the bowel equipped by the ligated vessel. The midgut territory receives its sympathetic supply from the coeliac and superior mesenteric ganglia (T11 to L1), and its parasympathetic provide from the vagus. Both kinds of nerves are distributed to the gut through the superior mesenteric plexus. The hindgut territory receives its sympathetic provide from the lumbar sympathetic chain (L1, 2), and its parasympathetic provide from the pelvic splanchnic nerve (nervi erigentes), each via the superior hypogastric and inferior mesenteric plexuses. The ultimate distribution of nerves in the intestine is similar to that within the wall of the small intestine. The parasympathetic nerves are motor to the big gut and inhibitory to the internal anal sphincter. Pain impulses from the intestine as much as the descending colon journey through the sympathetic nerves, and from the sigmoid colon and rectum through the pelvic splanchnic nerves. It is situated in the best iliac fossa, above the lateral half of inguinal ligament.
Purchase genuine arava lineDifferences between higher motor neuron and lower motor neuron paralyses Brain�Neuroanatomy 1 symptoms just before giving birth buy cheap arava line. Some nerves type the afferent loop and others kind the efferent loop of the reflex arc. Olfactory takes the sense of smell and stimulates dorsal nucleus of vagus for enhanced secretion, if the smell is good. The nuclear complex contains the next components: � Dorsolateral-to supply inferior rectus muscle � Intermediate-to inferior indirect � Ventromedial-to medial rectus � Caudal central-to part of levator palpabrae superioris � Median raphe-to superior rectus � Edinger-Westphal-to ciliaris and sphincter pupillae muscle tissue. It descends to the lateral wall of the sinus where it lies above the trochlear nerve. In the anterior a part of the sinus, the nerve divides into upper and lower divisions. In the fissure, the nasociliary nerve lies in between the two divisions while the abducent nerve lies inferolateral to them. The bigger, decrease, division divides into three branches for the medial rectus, the inferior rectus and the inferior oblique. Ptosis or drooping of upper eyelid because of paralysis of voluntary a half of levator palpebrae superioris muscle. Dilatation of pupil due to paralysis of parasympathetic fibres to sphincter pupillae muscle. Eyeball will get turned downwards and laterally because of unopposed motion of lateral rectus and superior indirect muscle tissue. Functional Components 1 General somatic efferent fibres, for lateral movement of the eyeball. The connections of the nucleus are much like those of the oculomotor nucleus, aside from the pretectal nuclei. It passes between the posterior cerebral and superior cerebellar arteries to appear ventrally between the temporal lobe and higher border of pons. Nucleus 3 the nerve runs upwards, forwards and laterally via the cisterna pontis and normally dorsal to the anterior inferior cerebellar artery to reach the cavernous sinus. As the nerve crosses the superior border of the petrous temporal bone, it passes beneath the petrosphenoidal ligament, and bends sharply forwards. Connections of the nucleus are much like these of the third nerve, apart from the pretectal nuclei. Its susceptibility to such injury is due to its long course within the cisterna pontis, to its sharp bend over the superior border of petrous temporal bone and the downward shift of the mind stem in the course of the foramen magnum leading to medial squint and diplopia. Branches of this nerve provide sensory fibres to the 4 parasympathetic ganglia associated with cranial outflow of parasympathetic nervous system. Ophthalmic, the first division, carries sensory fibres from the structures derived from frontonasal course of. Maxillary, the second division, conveys afferent fibres from buildings derived from maxillary process. Mandibular, the third blended division, carries sensory fibres derives from mandibular process. Principle sensory nucleus of V nerve: Fibres carrying touch and strain relay in this nucleus. It receives proprioceptive impulses from muscle tissue of mastication, temporomandibular joint and teeth. The fibres of the motor nucleus provide eight muscles derived from first branchial arch. It includes three branches, two of which Sensations of pain, temperature, touch and pressure from skin of face, mucous membrane of nose, most of the tongue, paranasal air sinuses journey along axons. Ophthalmic nerve fibres finish within the inferior half, maxillary nerve fibres end in the center half and mandibular nerve fibres terminate in the upper part of spinal nucleus. Proprioceptive fibres from muscles of mastication, extraocular muscular tissues and facial muscular tissues bypass V ganglion to attain unipolar cells of mesencephalic nucleus. Axons of neurons of spinal nucleus, superior sensory nucleus and central processes of cells of mesencephalic nucleus cross to the alternative facet and ascend as trigeminal lemniscus. The lemniscus ends within the ventral posteromedial nucleus of thalamus, where these fibres relay. Its branches are: Frontal Lateral a half of higher eyelid; conveys secretomotor fibres from zygomatic nerve to lacrimal gland. Maxillary Nerve Division (Sensory) 1 Supratrochlear: Upper eyelid, conjunctiva and lower part of brow. Nasociliary Meningeal branch In Pterygopalatine Fossa 1 Long ciliary: Sensory to eyeball. Zygomaticofacial 3 Posterior superior alveolar In Infraorbital Canal 1 Middle superior alveolar 2 Anterior superior alveolar On Face Infraorbital a. Sensory examination: � An ascending lesion spares the openings of nostril and mouth (muzzle area) until final. If pterygoid muscles are weak, the jaw would deviate to weak side as the conventional muscles will push the jaw to the weak side. Efferent pathway of sneeze reflex is nucleus ambiguus, respiratory centre in medulla oblongata, phrenic nerve nucleus, motor cells of spinal wire for intercostal muscles. The principal illness affecting sensory root of V nerve is characterised by attacks of severe ache in the space of distribution of maxillary or mandibular divisions. Penetrating wounds of parotid gland may injury each auriculotemporal and nice auricular nerves. Proprioceptive impulses from muscle tissue of the face travel by way of branches of the trigeminal nerve to reach the mesencephalic nucleus of the nerve. The a half of the nucleus that supplies muscular tissues of the higher a half of the face receives corticonuclear fibres from the motor cortex of both the right and left sides. The two roots run laterally and forwards, with the eighth nerve to reach the inner acoustic meatus. The first part is directed laterally above the vestibule; the second part runs backwards in relation to the medial wall of the center ear, above the promontory. The second bend is gradual, and lies between the promontory and the aditus to the mastoid antrum. In its extracranial course, the facial nerve crosses the lateral aspect of the bottom of the styloid course of. It enters the posteromedial floor of the parotid gland, and runs forwards through the gland crossing the retromandibular vein and the exterior carotid artery. Behind the neck of the mandible, it divides into its five terminal branches which emerge along the anterior border of the parotid gland. The nerve to the stapedius arises opposite the pyramid of the center ear, and provides the stapedius muscle. The muscle dampens extreme vibrations of the stapes caused by high-pitched sounds. The chorda tympani arises within the vertical a half of the facial canal about 6 mm above the stylomastoid foramen.
References - Horwich TB, Fonarow GC, Hamilton MA, et al. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol 2002;39:1780.
- Koontz MZ, Visser BM, Kunz PL. Neoadjuvant imatinib for borderline resectable GIST. J Natl Compr Canc Netw 2012;10(12):1477-1482.
- Bott SR, Young MP, Kellett MJ, et al: Contributors to the UCL Hospitalsi Trust Radical Prostatectomy database. Anterior prostate cancer: is it more difficult to diagnose?, BJU Int 89(9):886n889, 2002.
- Meyers JD, Flournoy N, Thomas ED. Nonbacterial pneumonia after allogeneic marrow transplantation: a review of ten yearsí experience. Rev Infect Dis. 1982;4:1119-1132.
|

