|
Tyr Ohling Wilbanks, MD, FACS - Assistant Clinical Professor of Surgery
- Columbia University College of Physicians
- and Surgeons
- Associate Chief of Surgery
- Lincoln Medical and Mental Health Center
- Bronx, New York
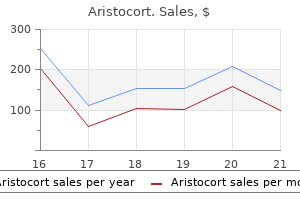
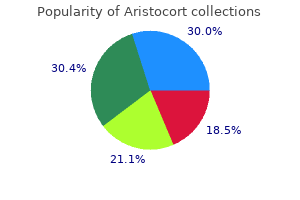
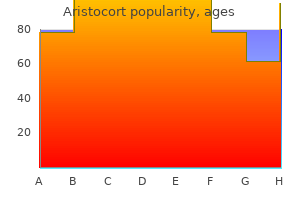
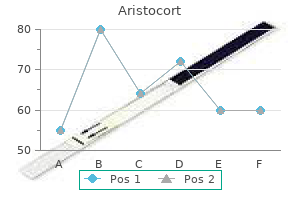
Aristocort dosages: 40 mg, 15 mg, 10 mg, 4 mg
Aristocort packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills

Purchase cheap aristocort onlineEpidural analgesia has been proven to hasten recovery from postischemic paralytic ileus in a rat model (53) and to stop endotoxin-induced gut mucosal damage in rabbits (54) allergy treatment vitamins purchase aristocort mastercard. During the perioperative interval, coagulation-related problems could also be an essential cause of morbidity. Spinal and epidural anesthesia using local anesthetic regimens will attenuate perioperative hypercoagulability and will provide physiologic advantages. Following surgical incision, there is a rise in coagulation elements and platelet activity and a decrease in fibrinolytic exercise (49). Intraoperative neuraxial anesthesia has been proven to attenuate perioperative increases in coagulation proteins (62) and platelet activity (63), to protect fibrinolytic exercise (7), and to increase arterial and venous blood circulate. Local anesthetics administered for epidural anesthesia and analgesia may be absorbed systemically and thereby exert systemic antithrombotic results, together with reduction in platelet aggregation, inhibition of thrombus formation, and discount in blood viscosity (64). Patients who were randomized to receive epidural anesthesia-analgesia had one-ninth the incidence of vascular graft occlusion (63). Patients who have been randomized to obtain epidural anesthesia and analgesia had one-fifth the incidence of reoperation (67). Compared to systemic parenteral opioids, epidural analgesia offers statistically lower pain scores for up to four days after a wide range of surgical procedures. Chronic ache following surgery has only lately been thought-about as a big postoperative complication (see Chapter 43). The incidence of chronic ache after surgical procedure varies by process but may be fairly high, with reported incidences of 30% to 81% after limb amputation, 22% to 67% after thoracotomy, 17% to 57% after breast surgery, 6% to 56% after cholecystectomy, and 4% to 37% after hernia repair (70). Persistent pain has additionally just lately been reported after cesarean section in approximately 12% of sufferers at 10 months after surgical procedure (71). As mentioned earlier on this chapter and mentioned at length in Chapters 31 by way of 33, peripheral and central sensitization may occur following surgery, finally resulting in persistent ache with hyperalgesia and allodynia. Patients undergoing thoracic surgical procedure underneath general anesthesia had been randomized to receive either steady epidural block before surgical incision or at completion of surgical procedure. Postoperative pain was less within the group that acquired steady epidural block previous to surgical incision. This group also had lower postoperative ache scores and the next percentage of pain-free patients at 3 and 6 months after surgical procedure (73). Postoperative central nervous system problems are generally marked by deficits in cognition and memory. These problems encompass a variety of postoperative states together with delirium or dementia (impairment in cognitive function), amnesia (impairment in memory), and sedation (impairment of consciousness). The etiologies of these issues are complex and could additionally be distinct for specific problems. However, mental function usually reaches a nadir in the early postoperative period, with a recovery to preoperative levels by 1 week following surgery in most sufferers (74,75). Delirium is a particularly problematic subset of postoperative cognitive dysfunction as it may contribute to at least a further 17. Delirium might happen in 9% to 11% of aged sufferers undergoing elective noncardiac surgical procedure (78,79) and as many as 36. Higher levels of postoperative pain severity are associated with a better incidence of postoperative cognitive dysfunction (especially delirium) (82,83). However, the effect of postoperative analgesia on psychological operate has not been rigorously investigated as trials in this area usually lack management of the postoperative analgesic routine. Chapter 7: Neural Blockade: Impact on Outcome 151 Patient-oriented Outcomes Patient-oriented ("nontraditional") outcomes, corresponding to affected person satisfaction, high quality of life, and high quality of restoration, are essential, valid outcomes that have been extensively utilized in other areas of drugs and are becoming more necessary within the field of anesthesiology and perioperative care. Although many various patient-oriented outcomes exist, several elements of regional anesthesia and analgesia. Although provision of analgesia is a generally acknowledged aim for postoperative pain control, the presence of analgesic agent�related unwanted effects, sometimes from opioids or native anesthetics, differ amongst analgesic methods and could additionally be an important affect on patientoriented outcomes. Patient satisfaction has turn out to be an important end result measurement and indicator of quality of medical care. Although assessing affected person satisfaction might seem intuitively straightforward, the idea of patient satisfaction incorporates many dimensions and domains and is quite complicated, embracing various theories, definitions, and concepts concerning affected person satisfaction still not clearly codified by consensus. Appropriate strategies to assess affected person satisfaction must make the most of validated survey instruments which have been psychometrically constructed (85). For example, patients who acquired epidural anesthesia for elective cesarean part had larger maternal satisfaction (using a validated instrument) compared with those who have been randomized to obtain spinal anesthesia, due in part to the elevated side effects. Complications A variety of complications could happen with neuraxial anesthesia and analgesia. These are discussed in detail in the context of perioperative care in Chapters 12 and 20, and in relation to ache administration in Chapter 50. In mild of those critical antagonistic results, clinicians must rigorously weigh the risks and benefits of contemplated neuraxial methods on an individual foundation. The incidence of neuraxial opioid-induced respiratory melancholy is dose-dependent and is reported to occur in approximately zero. Risk elements for the development of respiratory depression after administration of neuraxial opioids include growing dose, growing age, concomitant use of systemic opioids or sedatives, and possibly prolonged or intensive surgery, presence of comorbidities, and thoracic surgery (91). A prospective sequence of 4,185 patients with thoracic epidural catheters reported a 0. Epidural hematoma is probably one of the most feared complications of neuraxial methods. Although epidural vessel puncture might happen in up to 12% of epidural catheter placements (96), the event of symptomatic epidural hematomas is uncommon, with an estimated incidence of approximately 1:one hundred fifty,000 after epidural anesthesia/analgesia (97). Epidural abscess formation is luckily comparatively uncommon, with a reported incidence of zero. Although an epidural catheter provides a route of entry into the epidural house, epidural abscesses usually tend to outcome from hematogenous somewhat than direct spread (100) and are uncommon with routine postoperative use (101). Peripheral Nerve Analgesia and Outcomes Peripheral nerve blocks and catheter placement for steady local anesthetic infusion have turn out to be increasingly popular in acute postoperative pain administration. Peripheral methods provide extra targeted and limited sensory and motor block than central neuraxial analgesia and supply reduced risk of catastrophic issues such as spinal hematomas and abscesses. The amount of residency training devoted to regional anesthesia and peripheral nerve blocks has steadily elevated in the United States as a reflection of this increased interest and the potential advantages. A survey of American anesthesiology residency program directors in 2002 indicated that nearly 60% of programs now supply a specific peripheral nerve block rotation (102). A evaluation of medical case logs submitted from residents to the Residency Review Committee for Anesthesiology demonstrated a growth in use of regional anesthesia methods from 21% of cases in 1980 to 30% of cases in 2000 (103). Single-shot Peripheral Nerve Blocks Although wonderful evidence exists for elevated curiosity and coaching in peripheral nerve blocks, there stays little proof that these techniques have an effect on medical outcomes. Conceptually, single-shot peripheral nerve blocks would offer limited means to scale back the mechanisms of main perioperative problems described up to now. Duration of analgesia after a single injection of long-acting local anesthetic is at most about 12 hours (104), whereas maximal postoperative pain after major surgical procedure has a median length of 3 days (40). Mean and maximum ache scores for continuous perineural versus systemic opioid analgesia after a variety of surgical procedures.
Buy generic aristocort canadaEffect of intracranial strain on cerebrospinal fluid formation in isolated mind ventricles allergy symptoms children buy aristocort. The affect of lumbosacral cerebrospinal fluid volume on extent and length of hyperbaric bupivacaine spinal anesthesia: A comparison between seated and lateral decubitus injection positions. Development of the cerebrospinal fluid pathway within the normal and abnormal human embryos. The penetration of particulate matter form the cerebrospinal fluid into the spinal ganglia, peripheral nerves, and perivascular areas of the central nervous system. The nice construction of mobile layers and connective tissue space at spinal nerve root attachments in the rat. The destiny of intraneural injection as demonstrated by method of radio-active phosphorus. Arachnoid diverticula and cystlike dilatations of the nerve-root sheaths in lumbar myelography. Occult, bilateral anterior sacral and intrasacral meningeal and perineural cysts: Case report and review of the literature. Vertebral stage of termination of the spinal cord with report of a case of sacral wire. Biomechanical features of the subarachnoid house and cervical wire in healthy individuals examined with kinematic magnetic resonance imaging. Medullary cone movement in topics with a standard spinal cord and in patients with a tethered twine. Determination of the segmental sensory and motor innervation of the lumbosacral spinal nerves. The nerve provide of the vertebral column and its related structures within the monkey. The nature and distribution of the innervation of human supraspinal and interspinal ligaments. Spinal projections of cat major fibers innervating lumbar side joints and multifidus muscle. Lumbar disc lesion with special reference to the histological significance of nerve endings of the lumbar discs. Immunohistochemical demonstration of nociceptors within the ligamentous buildings of the lumbar spine. Substance P: Localization, concentration and release in cerebral arteries, choroid plexus and dura mater. Immunohistochemical localization of substance P in the lumbosacral spinal pia mater and ventral roots of the cat. Localization of substance P and neurofilament immunoreactive fibers in the lumbar aspect joint capsule and supraspinous ligament of the rabbit. Morphological foundation for again pain: the demonstration of nerve fibers and neuropeptides in the lumbar aspect joint capsule however not in ligamentum flavum. Discharge properties of mechanosensitive afferents supplying the retroperitoneal area. Characterization of spinal somatosensory neurons having receptive fields in lumbar tissues of cats. A quantitative study of the central projection patterns of unmyelinated ventral root afferents in the cat. The spinal nerve root "innervation", and a new concept of the clinicopathological interrelations in again pain and sciatica. Observations on the trigger and mechanism of symptom-production in sciatica and low-back ache. The tissue origin of low back ache and sciatica: A report of ache response to tissue stimulation during operations on the lumbar backbone utilizing native anesthesia. Identification of distinct topographical distribution of lumbar sympathetic and sensory neurons projecting to end organs with totally different features in the cat. Sympathetic activation of cat spinal neurons responsive to noxious stimulation of deep tissues within the low again. Electrical stimulation of the higher thoracic portion of the sympathetic chain in man. Pain responses on stimulation of the lumbar sympathetic chain underneath local anesthesia. On the nerve provide of the connective tissue of some peripheral nervous system elements. Three-dimensional evaluation of the vascular system in the rat spinal twine with scanning electron microscopy of vascular corrosion casts. Arterial vascularization of the spinal wire: Recent studies of the anastomotic substitution pathways. Preoperative spinal artery localization and its relationship to postoperative neurologic issues. Diffusion from the cerebrospinal fluid as a dietary pathway for spinal nerve roots. The vertebral and azygos venous systems, and a few variations in systemic venous return. The position of the vertebral venous system within the metastasis of cancer to the spinal column. A method of angiography of the azygos vein and the anterior inside venous plexus of the backbone. Comparison of intraosseous vertebral venography and Pantopaque myelography within the diagnosis of surgical conditions of the lumbar backbone and nerve roots. The significance of venous return impairment in ischemic radiculopathy and myelopathy. Distribution in spinal fluid, blood, and lymph of epidurally injected morphine and inulin in dogs. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. In the late nineteenth century, soon after the discovery of the local anesthetic properties of cocaine, spinal anesthesia was introduced into clinical practice. In the primary experiments and clinical use, the local anesthetic used was cocaine (Table 10-1) (1). Therefore, the use of spinal anesthesia was limited to a couple of fanatics until safer native anesthetics-procaine (2) and later tetracaine (3)-caused a widespread interest in its use. The growth of recent basic anesthesia utilizing muscle relaxants and an endotracheal tube, together with the worry of neurologic problems, decreased the interest in spinal anesthesia in 1940s and Fifties (6). As operations grew to become more radical, their length and extensiveness have been usually incompatible with spinal anesthesia.
Discount aristocort amexIf a couple of chiral center is present allergy shots long term effects cheap aristocort online, they must be designated by their configuration at each place. As examples, levobupivacaine, which has one chiral middle, is (S)-1-butyl-2piperidylformo-2,6 -xylidide; natural (-)-cocaine, which has two chiral centers, the place of every being specified, is 3(S)benzoyloxy-2(R)-methoxycarbonyl tropane. Presently, drug regulatory authorities are attuned to new chemical entity racemic medicine; these must be demonstrated as being no less secure than their enantiopure counterparts (39). Analytical separation of native anesthetic (and many other) pairs of enantiomers for pharmacokinetic and other purposes relies on their totally different affinities for chiral macromolecular stationary phases, sometimes 1 -acid glycoprotein (also known as orosomucoid), or cyclodextrin, packed into a chromatographic column (40�42). On a producing scale, a racemate similar to bupivacaine, an organic base, could be separated into its component R- and S-enantiomers by mixture with an acceptable enantiomer of an natural acid, corresponding to tartaric acid, to form two diastereomer salts which have completely different solubilities and thus unique propensity for selective precipitation; this may be a widespread laboratory course of known as resolution, and business strategies have been patented for this process (43). Alternatively, chiral synthesis to protect the stereochemistry at the chiral center of the reagents used can be utilized to produce the required enantiomer selectively (44). For any drug, the industrial technique used finally is determined by cost-effectiveness of the method and the chemistry of the actual drug. Application of the various types of stereochemical notation is given in Table 3-2 using mepivacaine and bupivacaine as examples (522). Prilocaine, mepivacaine, bupivacaine, etidocaine, and articaine had been launched into scientific use as racemates before it was appreciated how necessary these agents would possibly turn out to be. Once in the body, enantioselectivity in pharmacokinetics makes a racemic agent into a nonracemic mixture, so that a measured plasma focus of bupivacaine, for instance, will usually comprise an unequal mixture of R- and S-bupivacaine. The efficiency of local anesthetic agents is decided early in drug improvement by blockade of isolated nerve electrophysiologic studies and/or neural blockade procedures in intact laboratory rodents. Their relative potency is commonly specified in terms of their equi-effective anesthetic concentrations, and some well-known relationships between brokers are given in Table 3-1. Equi-effectiveness is sometimes judged by scientific bioassay, for example, by topics having similar characteristics of neural blockade. By-and-large, the same chemical and physicochemical modifications that influence anesthetic efficiency among the numerous brokers also influence efficiency for toxicity, whether or not the brokers be ester- or amide-type, with some changes for variations launched by additionally contemplating chirality. Among these agents, the stronger substances are more lipophilic and less hydrophilic, and this could engender situations during which the physical presentation of the local anesthetic agent is limited by the soluble amount of dose. Greater efficiency can be normally associated with a longer length of neural blockade; for example, Chapter 3: Properties, Absorption, and Disposition of Local Anesthetic Agents 53 intrathecal doses of bupivacaine 4- and 8-mg have approximately the same time programs of neural blockade as ropivacaine 8- and 12-mg (47). Various nerve blocks are actually getting used to provide a means for assessing the relative potency of native anesthetic brokers for producing relevant results. It has been discovered, for example, that the imply (and 95% confidence intervals) of the relative analgesic potency ratios in intrathecal labor analgesia have been zero. Similarly, in separate studies, the relative ropivacaine-to-bupivacaine analgesic efficiency ratio for epidural labor analgesia was found to be 0. The different ratios for ropivacaine-tolevobupivacaine between intrathecal and epidural dosing presumably replicate the extra advanced milieu of epidural analgesia, as described later. The up-down sequential dose technique has also been used for assessing the effectiveness of remedies underneath particular conditions. The up-down sequential dose method is also used assessing mixture treatments with components corresponding to epinephrine or opioids (59,60). Of these, diffusion is most immediately depending on the physicochemical properties of the agent. C/ (1) Inasmuch as they determine D, K, and C, physicochemical properties will influence the speed of transport of local anesthetic agent on the membrane level, and doubtlessly, subsequently, the time course of anesthetic and pharmacologic results. By influencing the equilibrium distribution of medicine between fluids and tissues, physicochemical properties additionally modulate exercise and overall drug movement in the bloodstream. Equation 1 may be simplified to Equation 2, by which the time period comprising the constants D, A, K, and is mixed right into a permeability constant P; this equation signifies that the focus difference throughout a membrane, C, is the driving force for drug movement. C (2) Some physicochemical properties of the clinically used local anesthetics are proven in Tables 3-1 and 3-3. As Table 3-1 exhibits, structural changes within the fragrant portion of the esters and within the amine group of the amides markedly alter bodily properties such as oil or lipid/aqueous partition coefficients and affinity for proteins. For example, with mepivacaine, substitution of a four-carbon n-butyl group for the one-carbon methyl group on the amine function provides bupivacaine a 35-fold enhance in distribution coefficiente, increased protein binding, and increased efficiency. Lipophilicity is usually estimated by the distribution coefficient with a suitable natural solvent and an aqueous buffer, typically at pH 7. Composite determine exhibiting the relationships between some physicochemical properties (lipophilicity given by octanol log P, and ionizability given by pKa) of n-N-alkyl homolog members of the mepivacaine family and some pharmacokinetic properties in fashions of spinal anesthesia. Me, methyl (mepivacaine); Et, ethyl; Pr, propyl (ropivacaine); Bu, butyl (bupivacaine); Pe, pentyl; Hx, hexyl. The pH-pKa relationship is related as a result of it governs the ratio of concentrations of drug in the ionized (more water soluble) and nonionized (less water soluble) types. Differences in molecular weight amongst medicine from homologous collection are usually additionally related to parallel variations in lipophilicity and pKa making it difficult to isolate the consequences of particular person variables. Under these circumstances, variations in diffusibility and permeability occur as second-order effects. Molecular Weight Molecular weights of the commonly used native anesthetic agent bases differ from 220 to 288 Da (Table 3-1). These brokers have basically the identical skeleton with the increases in molecular weight being due to alkyl substitution; therefore, lipophilicity and pKa additionally change with molecular weight. Ex vivo studies of the dural permeability of medication have been carried out with cadaveric tissues, and these demonstrate a comparatively minor influence of molecular weight. Although a comparatively simple model, cadaveric membrane-diffusion cell preparations are themselves topic to experimental vagaries of tissue selection (species, site and thickness, and so forth. In vivo studies are even more difficult to interpret due to the competing influences of vascular activity, systemic absorption, and uptake into fastened spinal tissues, as properly as cardiovascular sequelae of concurrent basic anesthesia within the preparation of living topics. When tested with an ex vivo preparation of monkey or rabbit spinal meninges, the permeability coefficients of a Chapter three: Properties, Absorption, and Disposition of Local Anesthetic Agents fifty five heterogeneous collection of drugs together with lidocaine and bupivacaine had been found to be unbiased of molecular weight (and molecular axis and molecular volume); nonetheless, a bell-shaped relationship was found with lipophilicity (as measured by the octanol-to-pH 7. When examined ex vivo with a sequence of homologous mepivacaine-like native anesthetics. The permeability of human dura mater ex vivo to quite lots of opioids and native anesthetic agents was found to depend upon easy diffusion, unbiased of molecular weight, pushed by the concentration gradient, and was not enantioselective (69,seventy four,75). There is, however, some proof to counsel that molecular weight could be related to the diffusion of native anesthetics within the sodium (Na+) channel of the nerve membrane (76). Recent correspondence within the literature has additionally drawn attention to the relationship between molar and mass label portions of some native anesthetic brokers that could have implications for differences in dose requirements and the relative potency of comparable agents (77�79). It is worth reiterating here some parts of that discussion as a result of it additionally involves international differences that may occur in labeling necessities. An aqueous answer for injection will be made of the salt, but the focus of active ingredient may be specified either as that of the salt or the bottom; the water of crystallization is normally allowed for and adjustments are made. Levobupivacaine may, therefore, seem to be stronger than bupivacaine if this distinction in concentration had been to be ignored. The message is apparent: check the domestically issued product label/information as to how the focus of local anesthetic agent is specified! Ka = [H+][base] [conjugate acid] (4) the place the sq. brackets indicate focus or, extra correctly, exercise.
Discount 4 mg aristocort with mastercardBoth cart-based and transportable allergy symptoms swollen throat cheap 4 mg aristocort fast delivery, compact ultrasound machines at the moment are obtainable and fitted to nerve imaging. In theory, visual steering can impart confidence to anesthesiologists, enhance safety of sufferers, and enhance environment friendly time utilization within the working room. Outcomes information to demonstrate convincingly that the scientific advantages of ultrasound are pending. There is little doubt that this imaging technology will be a useful and enduring part of practice in regional anesthesia. In this text, where relevant, ultrasound-guided block strategies and out there literature shall be discussed. Preoperative Preparation, Psychology and Communication Psychology and communication play an important half within the success of any anesthetic method (10). Premedication Pharmacologic premedication facilitates patient consolation during regional anesthesia efficiency (11). Advantages of premedication embrace improved affected person satisfaction, acceptance, and cooperation. Disadvantages embody unpredictable response, unwanted effects, and interference with cooperation (12). In some instances, particularly with aged sufferers and in ambulatory surgical procedure, premedication is omitted. General Principles of Ultrasound-guided Nerve Block Techniques Certain basic rules apply to the profitable use of ultrasound to guide nerve block techniques: the standard of ultrasonographic nerve pictures relies on the quality of the ultrasound machine and transducers, correct transducer selection. Sterile conducting gel and a sterile plastic sheath to absolutely cowl the whole transducer should be used particularly for catheter strategies. Ultrasonography supplies anatomic information, while a motor response to nerve stimulation supplies practical details about the nerve in question. Observing local anesthetic spread is a valuable function of ultrasound along with real-time visible steerage to navigate the needle towards the goal nerve. This approach is most well-liked when you will need to observe the needle tip at all times. In this case, the ultrasound image captures a transverse view of the needle, which is proven as a hyperechoic "dot" on the screen. Accurate moment-to-moment tracking of the needle tip location can be difficult, and needle tip position is often inferred indirectly by tissue motion and native anesthetic spread. This strategy, nevertheless, is especially useful for continuous catheter placement along the lengthy axis of the nerve. A: Short-axis needle method with block needle perpendicular to the ultrasound beam. Some of its fibers unite with fibers from the first lumbar nerve and are terminally represented because the iliohypogastric and ilioinguinal nerves. The first are the paired grey and white rami communicantes, which cross anteriorly to and from the sympathetic ganglion and chain. The second department arises as the posterior cutaneous department and supplies the skin and muscles within the paravertebral region. The third department is the lateral cutaneous division, which arises just anterior to the midaxillary line. This branch is of most concern to the anesthesiologist as a end result of it immediately sends subcutaneous fibers coursing each posteriorly and anteriorly to supply pores and skin of a lot of the chest and abdominal wall. In the higher 5 nerves, this branch terminates after penetrating the exterior intercostal and pectoralis major muscles to innervate the breast and front of the thorax. The decrease six anterior cutaneous nerves terminate after piercing the sheath of the rectus abdominis muscle, to which they supply motor branches. Some ultimate branches continue an- teriorly and turn into superficial near the linea alba, to provide cutaneous innervation to the midline of the abdomen. Medial to the posterior angles of the ribs, the intercostal nerves lie between the pleura and the fascia of the interior intercostal muscle. At the angle of the rib (6 to eight cm from the spinous processes), the nerve comes to lie between the internal intercostal muscle and the intercostalis intimus muscle. Cadaver studies have shown that the nerve itself remains subcostal solely 17% of the time, has most regularly (73%) moved inferiorly into the midzone between ribs, and is often branching at this point (16). The costal groove turns into a sharp inferior fringe of the rib, about 5 to 8 cm anterolateral to the angle of the rib. Note additionally (a) the spinal nerves and dorsal root ganglia within the region of intervertebral foramen, with threat of perineurial spread into spinal fluid after intraneural injection on this region; (b) direct injection into an intervertebral foramen may reach spinal fluid via a dural cuff; (c) local anesthetic could gain entry to epidural area by diffusing into an intervertebral foramen; (d) near the midline, the intercostal nerve lies immediately on the posterior intercostal membrane and pleura; and (e) paravertebrally, answer may diffuse to rami communicantes and sympathetic chain. Section is proven in area of costal groove, which extends from close to the top of the rib to 5 to 8 cm anterior to the angle of the rib. At the extent of the angle of the rib, the intercostal nerve (one or more) lies inferior to vein and artery in the intercostal groove. The inclined position is particularly favored if bilateral blocks are to be carried out. A pillow is positioned under the abdomen to lower the lumbar lordosis and to intensify the intercostal spaces posteriorly. The arms should be allowed to hang down from the edge of the block desk to allow the scapula to rotate as far laterally as possible. The next step is to palpate laterally to the edge of the sacrospinalis group of muscles, where the ribs are most superficial. This distance is somewhat variable, depending on body size, muscle mass, and physique, but is normally 6 to 8 cm from the midline. Subsequent traces are drawn considerably parallel to the first one, but with a pattern to angle medially at the upper ranges because the sacrospinalis muscular tissues taper, so as to avoid the scapulae. The caudal finish of the road ought to cross near the end of the shortened twelfth rib, which is usually simple to palpate. For thoracic or other unilateral chest wall surgery, only the suitable facet and ribs are marked. The needle insertion level is infiltrated with native anesthetic using a 25-gauge needle. The ribs and intercostal areas are thicker on the angle of the rib, allowing a larger margin of safety before pleura is contacted. Note finger palpating rib nonetheless in place and hand holding syringe firmly braced against again. The lowest (most inferior) intercostal nerve is blocked first as a end result of the decrease ribs are straightforward to palpate. A 25-gauge 15-mm or a 23-gauge 25-mm needle is introduced in 20-degree cephalad orientation through the pores and skin between the tip of the retracting fingers and superior till it contacts rib. The average distance from posterior rib to pleura averages 8 mm (17), so advancing a small distance (2�3 mm) after walking off the rib is protected. Intercostal nerve blocks may also be positioned at the midaxillary line whereas the patient is mendacity supine. The ribs appear as dense, dark oval structures with a bright surface (periosteum).
Cheap aristocort genericOn the parable of the glial/Schwann junction (Obersteiner-Redlich zone): origin of vestibular nerve schwannomas jackfruit allergy treatment order aristocort australia. Intralabyrinthine schwannomas: analysis, administration, and a model new classification system. Hearing loss owing to intralabyrinthine schwannoma conscious of intratympanic steroid treatment. Factors affecting ultimate facial nerve end result following vestibular schwannoma surgery. Cochlear implantation in unilateral sudden deafness improves tinnitus and speech comprehension: meta-analysis and systematic evaluate. Cochlear Implantation in Patients with Intracochlear and Intralabyrinthine Schwannomas. Numerous retrospective case stories, case series, and literature reviews have elevated our information of these tumors. Armed with the knowledge of their scientific presentation and overlap with other neurotologic pathology, as nicely as the imaging specifics required to visualize these tumors, clinicians will definitely lower delays in analysis. Though a conservative "wait-andscan approach" can be utilized for many patients, operative administration is typically indicated and ends in uncommon morbidity. Primary internal ear schwannomas: a case series and systematic review of the literature. Dephosphorylation results in a closed confirmation and activation of the molecule. This is managed by a family of ras-related kinases including protein kinase A and p21 activated kinases. The unphosphorylated active form may have numerous roles, all of which act to inhibit cell growth19: 1. An upstream regulator of the Hippo pathway, a regulator of cell progress by contact inhibition. Patients with mosaicism usually have less severe disease and the severity of illness is said to the proportion of cells affected. The earlier the mutation takes place, the extra affected cells are present and the more severe the disease. Truncating mutations, together with non-sense and frameshift mutations, are related to a youthful age of disease presentation and extra extreme phenotype24,26,27,28 and poorer survival29 than that seen with missense mutations, in-frame mutations, or large deletions. Splice-site mutations, in distinction, may end up in a range of illness severity relying on the site of the mutation. For instance, mutations within the first five exons are associated with extra severe illness than those occurring in exons 11 to 15. It has been hypothesized that the mutant protein dimerizes with the traditional product leading to much less regular product to suppress tumor growth. Truncating mutations have a better prevalence of meningioma in comparison with missense or splice-site mutations. For instance, splice-site mutations in exons eleven to 15 are associated with less extreme disease than splice-site mutations in exons 1 to 530 and threat of meningioma growth is larger if a mutation is in exons 1 to 3 in comparability with exons 14 to 15. Second, it supplies some measure of doubtless severity of illness depending on the type of mutation recognized. Fourth, if a mutation is identified, it facilitates screening of currently unaffected relations for the mutation. For youngsters of affected people, screening might start at birth with an examination of the eyes to identify cataracts. The practicalities of scanning at youthful ages are difficult and improvement of symptomatic tumors earlier than 10 years of age could be very uncommon. Above the age of 20 years, the scanning interval can be elevated to three to 5 years as tumors are inclined to grow less aggressively with rising age. If an individual has a confirmed mutation, then cranial imaging should be undertaken yearly and spinal imaging undertaken every 3 years. If no tumor has been identified by the age of forty years, then scanning may be discontinued. This ought to ideally be undertaken from tumor, however testing in blood can be likely to be useful. For de novo sufferers, the danger of transmission is considerably much less due to mosaicism. Follow-up cranial imaging should happen at 5, 10, and 20 years after initial evaluation for all at-risk sufferers. Individuals fulfilling two standards of the Manchester standards < 50 years of age but including childhood mononeuropathy as a criterion. Other patients with decrease risk (but still at risk) include these with unilateral vestibular schwannomas aged between 20 and 30 years and people fulfilling two Manchester criteria over 50 years of age. Patients with two or extra nonvestibular schwannomas should be assessed for this situation by tumor and blood analysis. Various forms of mutations of the gene have been identified with truncating mutations being the most common. Severity of illness is associated with the sort of mutation, with truncating mutations being associated with extra extreme illness than deletions. Identification of the mutation in blood is feasible in 93% of circumstances in nonmosaic individuals however is significantly decrease in mosaic sufferers. Prevalence, mutation rate, health, and affirmation of maternal transmission impact on severity. Bilateral acoustic neurofibromas: a clinical examine and field survey of a family of five generations with bilateral deafness in thirty eight members. A mutation in the neurofibromatosis sort 2 tumor-suppressor gene, giving rise to broadly different medical phenotypes in two unrelated individuals. Somatic mosaicism in neurofibromatosis 2: prevalence and threat of illness transmission to offspring. A novel moesin-, ezrin-, radixinlike gene is a candidate for the neurofibromatosis 2 tumor suppressor. Alteration in a new gene encoding a putative membrane-organizing protein causes neuro-fibromatosis sort 2. The molecular biology of vestibular schwannomas: dissecting the pathogenic course of on the molecular degree. Ruffling membrane, stress fiber, cell spreading and proliferation abnormalities in human Schwannoma cells. Germ-line mutations in the neurofibromatosis 2 gene: correlations with disease severity and retinal abnormalities. Segmental neurofibromatosis kind 2: discriminating two hit from four hit in a patient presenting a quantity of schwannomas confined to one limb. CpG island methylation in sporadic and neurofibromatis type 2-associated schwannomas. Determination of the mutant allele frequency in patients with neurofibromatosis type 2 and somatic mosaicism via deep sequencing.
Common Oak (Oak Bark). Aristocort. - What is Oak Bark?
- How does Oak Bark work?
- Colds; fever; cough; diarrhea; bronchitis; loss of appetite; improving digestion; inflammation of the skin, mouth, throat, genital, and anal region; and other conditions.
- Dosing considerations for Oak Bark.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96504
Discount aristocort 4 mg visaCervical epidural analgesia by way of a thoracic method using nerve stimulation steering in an adult patient undergoing elbow surgical procedure allergy symptoms go away generic 4mg aristocort with mastercard. Thoracic epidural catheter placement in infants by way of the caudal approach underneath electrocardiographic steerage: Simplification of the original approach. Ultrasound steerage speeds execution and improves the standard of supraclavicular block. Practice Guidelines for sedation and analgesia by non-anesthesiologists: An up to date report by the American Society of Anesthesiologists task pressure on sedation and analgesia by non-anesthesiologists. Sedative infusions throughout native and regional anesthesia: A comparison of midazolam and propofol. A comparison of propofol with a propofol-ketamine mixture for sedation during spinal anesthesia. Comparison of responses to transmitter candidates at an Nmethylaspartate receptor mediated synapse, in slices of rat cerebral cortex. Concomitant administration of morphine and an N-methyl-D-aspartate receptor antagonist profoundly reduces inflammatory evoked spinal c-Fos expression. The benefits of intraoperative small-dose ketamine on postoperative ache after anterior cruciate ligament repair. Preemptive analgesia by intravenous low-dose ketamine and epidural morphine in gastrectomy: A randomized double-blind study. Intraoperative ketamine together with epidural analgesia: Postoperative analgesia after renal surgical procedure. A comparability of dexmedetomidine versus typical therapy for sedation and hemodynamic management during carotid endarterectomy carried out beneath regional anesthesia. Comparison of intravenous sedativeanalgesic techniques for outpatient immersion lithotripsy. Remifentanil or propofol for sedation during carotid endarterectomy under cervical plexus block. Remifentanil versus remifentanil/ midazolam for ambulatory surgery during monitored anaesthesia care. Remifentanil, propofol or both for aware sedation throughout eye surgical procedure under regional anaesthesia. Speed of recovery and side-effect profile of sevoflurane sedation in contrast with midazolam. Beyond this, anatomic understanding is required to keep away from problems due to needle damage or incorrectly placed injection, to understand the physiologic events resulting from neural blockade, and to develop new techniques for anesthesia and ache treatment. This is partially as a result of the special interests of anesthesiologists in such issues because the group of tissue planes and the permeability of assorted limitations that regulate distribution of fluids, pursuits shared by few other physicians and scientists. An additional challenge is the problem of observing the contents of the spinal canal, that are enclosed by sturdy bones and ligaments. Removal of these constructions disrupts the natural arrangement of the gentle tissues inside the canal. This article anatomically tours the neuraxis, typically from outer to internal buildings, and contains new observations wherever attainable. Errors are comparable within the sitting and mendacity positions, are larger with overweight subjects, and are larger using the vertebra prominens as a reference level compared to the Tuffier line (10,11). The numerical designations of the vertebra could differ between individuals because of anomalous patterns of vertebral segmentation, that are predominantly discovered within the lumbosacral backbone (12). This parallels the phylogenetic stability of mammalian cervical and thoracic segmentation and the marked variability in the number of lumbar vertebrae, even amongst primates (13). The final lumbar or first sacral vertebrae is often indeterminate in configuration, with fusion of L5 to S1 in 6. Although the vertebrae differ in design at the numerous levels of the vertebral column, common components could be defined. The lumbar vertebral bodies are distinctly narrowed into an hourglass form, with a diameter 15% less at the middle than on the endplates (14). Stout pedicles come up on the posterolateral features of the body and fuse with the platelike laminae to encircle the vertebral foramen. Together, the vertebral foramina of the adjacent vertebrae in sequence type the vertebral (or spinal) canal. The width of the canal measured between the pedicles is narrowest within the thoracic area (about 17 mm), but widens in each the cervical (25 mm) and lumbar areas (about 22 mm at L1 to about 27 mm at L5) (15�20). In contrast, the anterior/posterior diameter of the vertebral canal is pretty fixed (about 16 mm) throughout the vertebral column (21). The transverse process relies at the junction of the pedicle and lamina and passes laterally. The spinous process tasks posteriorly from the midline junction of the laminae, is usually bifid within the cervical column, and may not lie in the midline at different ranges. The sample described here varies considerably in different regions of the vertebral column. Vertebral our bodies are relatively large on the lumbar ranges, however less so in the thoracic column and particularly in the cervical area. Whereas the transverse processes are hooked up to the pedicles and laminae within the lumbar and thoracic zones, they take their origin from the vertebral body within the cervical vertebrae. This metameric arrangement into individual vertebrae additionally dictates that communication of the peripheral nervous system with the spinal twine must be likewise segmented, regardless of the shortage of any organization into subunits throughout the spinal twine. The seventh thoracic backbone is often reverse the inferior angle of the scapula, and the line connecting the iliac crests (Tuffier line) crosses the vertebral column most frequently on the L4�L5 disc. For instance, the primary thoracic vertebral backbone could also be more prominent than the seventh cervical. Also, the Tuffier line may cross the vertebral column as high because the L3�L4 disc or as little as the L5�S1 disc (2�5). For this reason, and due to a variable amount of subcutaneous fats, the accuracy of predicting the vertebral degree of needle insertion is about 50% at finest when unaided by radiologic imaging. Vertebral column, in lateral view (left) and posterior view (right), illustrating curvatures, lumbar interlaminar areas, and the sacral hiatus. In childhood, the sacral vertebrae are related by cartilage, however progressively fuse right into a single structure after puberty. Instead, the concave anterior surface of the sacrum features four pairs of large anterior sacral foramina that present passage from the midline sacral canal for the anterior rami of the higher 4 sacral nerves. In contrast with their posterior counterparts, which give an exit for the posterior primary rami at every level, the anterior foramina are unsealed and supply a ready passage for escape of native anesthetic resolution injected into the sacral canal. Lateral to this crest and medial to the 4 posterior sacral foramina is the intermediate sacral crest with a row of four tubercles, representing the higher 4 sacral articular processes. The remnants of the S5 inferior articular processes are free and distinguished, and flank the sacral hiatus, constituting the sacral cornua. Specifically, the quantity of the adult sacral canal may vary from 12 mL to sixty five mL (22).
Aristocort 4mg overnight deliveryChronic epidural catheterization in cancer sufferers can be a potential threat for epidural an infection allergy medicine safe breastfeeding order aristocort 4 mg on line. Du Pen and co-workers (78) studied 350 sufferers in whom permanent (tunneled) epidural catheters had been positioned. The authors examined three areas of the catheter monitor for evidence of an infection: exit site, superficial catheter monitor, and epidural house. The price of epidural and deep-track catheter-related infections was one in each 1,702 days of catheter use in the 19 patients who developed deeptrack or epidural infections. All 19 patients with deep infections had been treated with catheter elimination and antibiotics; none required surgical decompression or debridement. Catheters had been replaced in 15 of the 19 patients who requested them after remedy with no recurrent infections. The authors state recommendations similar to Strafford and colleagues (81); longterm epidural catheterization is protected when sufferers are rigorously monitored for signs of an infection and receive immediate remedy when the analysis is established. The main an infection is associated with viremia and could be accompanied by a wide range of symptoms, including fever, headache, and infrequently aseptic meningitis. In distinction, recurrent or secondary infections current as genital lesions without evidence of viremia. The sufferers studied confirmed no postpartum change in immune, infectious, or neurologic standing. However, in all three collection (with a combined total of 117 patients), the patients have been relatively healthy and in the early stage of their disease. The use of an antimicrobial cleaning soap reduces bacterial growth and reduces the danger of micro organism being released into the operative area should gloves turn into torn or punctured in the course of the process. An alcohol-based antiseptic supplies the utmost degree of antimicrobial exercise and period. At this time, there are insufficient knowledge to make suggestions relating to routine use for single-injection or momentary neuraxial/ peripheral catheter placement. However, placement of an indwelling permanent gadget, corresponding to a spinal wire stimulator, warrants the identical asepsis as a surgical process, including robes, hats, and antibiotic pretreatment (100,103). Interestingly, related stories have been noted among sufferers present process ache procedures. Antiseptic Solutions Controversy still exists concerning essentially the most appropriate and secure antiseptic solution for sufferers present process neuraxial and peripheral strategies. Povidone iodine and chlorhexidine gluconate (with or with out the addition of isopropyl alcohol) have been most extensively studied (109,110). In almost all medical investigations, the bactericidal effect of chlorhexidine was extra fast and more practical (extending its impact hours following its application) than povidone iodine. Although common anesthesia was administered to fifty nine patients, the remaining a hundred and ten patients obtained spinal or epidural methods. The authors concluded that neuraxial block was protected in circumstances of secondary an infection. Additional investigations assist these suggestions, though the total number of patients studied is too restricted to make a definitive evaluation (93,94). In addition, since the danger of neurologic complications in patients present process neuraxial block in the presence of primary an infection remains unknown, a conservative approach is beneficial. It should be famous that chlorhexidine-alcohol labeling accommodates a warning in opposition to use as a skin preparation prior to lumbar puncture. Therefore, because of its superior effect, alcohol-based chlorhexidine options are thought of the antiseptic of alternative for pores and skin preparation before any regional anesthetic process (100). Anesthetic Management of the Infected or Febrile Patient In abstract, a number of scientific and laboratory studies have instructed an association between dural puncture during bacteremia and meningitis. Patients with proof of systemic an infection may safely endure spinal anesthesia, if antibiotic therapy is initiated prior to dural puncture and the affected person has demonstrated a response to remedy, such as a decrease in fever. Placement of an indwelling epidural (or intrathecal) catheter in this group of patients stays controversial; sufferers ought to be carefully selected and monitored for evidence of epidural an infection. Spinal anesthesia may be safely performed in sufferers in danger for low-grade transient bacteremia after dural puncture. Once once more, little info exists concerning the risk of epidural anesthesia in sufferers suspected of developing an intraoperative transient bacteremia (such as throughout a urologic procedure). Likewise, the vary of microorganisms inflicting invasive infection in the immunocompromised host is way broader than that affecting the general population and consists of atypical and opportunistic pathogens. Consultation with an infectious disease specialist is suggested to facilitate initiation of early and effective therapy (91). Meticulous aseptic method, together with hand-washing with chlorhexidine, carrying of mask and sterile gloves by the proceduralist, pores and skin asepsis with chlorhexidine, and antibiotic pretreatment for the placement of permanent units, is important to the prevention of infectious problems related to regional anesthesia (100). A delay in diagnosis and treatment of even a couple of hours considerably worsens neurologic outcome. Meningitis presents most frequently with fever, extreme headache, altered level of consciousness, and meningis- mus. The clinical course of epidural abscess progresses from spinal ache and root pain, to weak point (including bowel and bladder symptoms), and ultimately paralysis. The initial back ache and radicular signs might remain stable for hours to weeks. However, the onset of weak point typically progresses to full paralysis inside 24 hours. A mixture of antibiotics and surgical drainage remains the remedy of alternative. As with spinal hematoma, neurologic recovery relies on the period of the deficit and the severity of neurologic impairment earlier than remedy. The reason for postoperative deficits is difficult to evaluate, as a end result of neural damage may occur as a result of surgical trauma, tourniquet strain, prolonged labor, improper affected person positioning, or anesthetic approach. Progressive neurologic ailments such as multiple sclerosis could coincidentally worsen perioperatively, independent of the anesthetic methodology. The most conservative authorized approach is to keep away from regional anesthesia in these sufferers. However, high-risk sufferers, including those with vital cardiopulmonary illness, may benefit medically from regional anesthesia and analgesia. The choice to proceed with a regional anesthesia in these sufferers ought to be made on a case-by-case basis. The presence of preexisting deficits, signifying chronic neural compromise, theoretically places these patients at elevated danger for additional neurologic harm. The presumed mechanism is a "double crush" of the nerve at two locations, resulting in a nerve damage of scientific significance. The double-crush concept means that nerve harm attributable to traumatic needle placement/local anesthetic toxicity through the efficiency of a regional anesthetic may worsen neurologic consequence within the presence of an additional patient factor or surgical damage. Progressive neurologic diseases may coincidentally worsen perioperatively, impartial of the anesthetic method.
Purchase aristocort 4 mg on lineSide results (nausea allergy on eyelid purchase cheapest aristocort, vomiting, urinary retention) were much less frequent within the paravertebral group (30% versus 75%; p <0. Intercostal Blockade Intercostal blockade (single-injection or continuous) was more in style for thoracotomy before thoracic epidural anesthesia turned widespread. The injections may be carried out either beneath direct view by the surgeon from contained in the chest or percutaneously. Cryoanalgesia Cryoanalgesia is carried out by making use of a cryoprobe to the nerve beneath direct view by the surgeon and freezing the nerve to �60 C to �80 C for two minutes. This native chilly shock destroys the myelin sheath without damaging the axons, an impact that may last for 3 months. As with intercostal blocks, the technique is applied on the degree of the surgical incision and the levels above and below (41,42). Studies evaluating cryoanalgesia to systemic opiates confirmed conflicting leads to pain aid as properly as pulmonary function with a marginal benefit toward cryoanalgesia. The method fell into disgrace when a quantity of studies demonstrated painful neuromas in 20% to 30% of sufferers after cryoanalgesia for thoracic surgery, occurring at about 6 weeks publish surgical procedure and lasting for about 4 weeks (43,44). In one examine, a lower within the submit thoracotomy ache syndrome was found with cryoanalgesia versus opioids or epidural or interpleural anesthesia (45). Interpleural Analgesia Interpleural analgesia consists of depositing native anesthetics between the parietal and visceral pleura. Explanations for the restricted analgesic efficacy of interpleural analgesia include (a) lack of native anesthetic by way of the chest tube, (b) dilution of native anesthetic with blood and exudative fluid current within the pleural cavity, (c) binding of local anesthetic with proteins, and (d) altered diffusion across the parietal pleural following surgical manipulation and inflammation. Phrenic Nerve Infiltration Approximately one-third of patients present process thoracic surgical procedure with thoracic epidural anesthesia complain of ipsilateral shoulder ache due to diaphragmatic irritation (49). A latest study evaluated the effect of infiltration of 10 mL of 1% lidocaine into the paraphrenic fats pad at conclusion of surgery at the level of the diaphragm in sufferers present process thoracotomy. Patients receiving lidocaine had a significantly decreased incidence of ipsilateral shoulder ache and an total reduction in ache score compared with placebo infiltration. This could also be a simple and effective method for optimizing postoperative ache control when used in conjunction with epidural analgesia (50). In the first 24 hours after surgical procedure, the median morphine consumption is analogous for lung biopsy and pleurectomy but significantly decrease than for pleural biopsy and sympathectomy (52,53). Analgesic use at the third and seventh days, in addition to lung function check recovery pattern, are unaffected by regional anesthesia (54). This strategy may also contribute to earlier postoperative ambulation and to decrease intraoperative opioid necessities. In a subsequent examine, higher ache control was famous only through the sixth postoperative hour by Hill, without the prolonged impact beforehand reported (58). A main distinction between these research is that, in the first one, all blocks were decided to achieve success earlier than inducing basic anesthesia, whereas in the Hill research, numerous failed blocks have been included. Regional Anesthesia in Patients with Chest Trauma the excruciating pain caused by coughing, deep breaths, and movement remains a administration concern in sufferers with chest trauma and rib fractures. An ideal method to control pain in these patients must be safe, present complete and extended analgesia, and facilitate deep breathing and clearance of secretions throughout chest physiotherapy. The method used should ideally also enhance respiratory dynamics, have minimal central nervous and systemic unwanted effects, and permit early mobilization. Systemic opioids may provide good static pain management but cause respiratory melancholy and hypoxemia. It may end up in high plasma levels of local anesthetic as a result of high vascularization of the pleural area (66). The drawback is the need for repeated block because of the short action of the native anesthetics. In addition, a quantity of injections are required, and together with fast absorption from the intercostal space, toxic ranges of local anesthetics can easily be reached. Multiple intercostal blocks nerve blocks for rib fractures additionally predispose to a better incidence of pneumothorax. The reported incidence of pneumothorax after intercostal blocks in sufferers with a quantity of rib fractures is 1. Regional Anesthesia for Esophagectomy Esophagectomy is a significant surgical process carried out in patients with esophageal cancer and is associated with high morbidity (20%�50%) and mortality (0%�30%). Thoracic epidural anesthesia is recommended as part of the intraoperative anesthetic administration and is sustained to present analgesia for three to 5 postoperative days. In addition to a beneficial effect on respiration and intestine perfusion, epidural anesthesia facilitates immediate extubation in the working room, thereby reducing the risks associated with prolonged mechanical air flow. Neal and colleagues also emphasized the importance of providing optimum analgesia with thoracic epidural anesthesia as part of the fast-track strategy. Thoracic epidural anesthesia facilitates ambulation the identical day of the surgery, reduces the incidence of ileus and deep venous thrombosis, and permits early enteral feeding (67). Thoracic epidural anesthesia used in the course of the postoperative course has been shown to lower the risk for anastomotic leakage (68). Shallow respiratory improves to near regular levels and paradoxical chest wall movements are lowered. Patients on a thoracic epidural anesthesia regimen are alert, in a place to cough adequately and comply with chest physiotherapy, and develop fewer issues (see Chapter 11). Thoracic epidural anesthesia might be technically demanding, particularly in sufferers distressed with pain. The neural blockade can masks intra-abdominal injuries and could also be related to hypotension through the early part of remedy, probably resulting in cardiovascular collapse and cardiac arrest within the inadequately resuscitated patient. Luchette and coworkers evaluated analgesia for 72 hours in 19 blunt trauma patients with unilateral rib fractures (66). Buggy and coworkers studied the impact of steady paravertebral anesthesia with levobupivacaine on the oxygen tension in the latissimus dorsi flap after mastectomy (70). The imply PtO2 over the 20-hour period was significantly greater in patients receiving paravertebral block (75 versus forty four mm Hg; p <0. Preincisional paravertebral anesthesia has been shown to scale back chronic ache after breast surgery. At 1-month after surgery, patients who received paravertebral anesthesia in the perioperative period had a decrease intensity of motion-related ache. At 6 months, the prevalence of any sort of ache continued to be lower, and at 12-month follow-up motion as nicely as pain at rest have been significantly lower within the paravertebral group. Neuraxial blockade grew to become in style later as their security elevated and functions for postoperative analgesia were developed. More lately got here the conclusion that regional anesthesia may influence a few of the perioperative components intrinsically tied with postoperative consequence (see also Chapter 7). Major decreases in splanchnic blood flow occur throughout low cardiac output states, and if this persists, the gut mucosal barrier could also be disrupted, resulting in generation of inflammatory mediators which, along with ischemia�reperfusion damage, precipitate gastrointestinal organ dysfunction (72). The control of splanchnic blood flow is regulated by way of a nice balance involving sympathetic and parasympathetic methods. Other native and systemic components also modulate the tone of the mesenteric vasculature. The resulting decreased venous return and systemic hypotension could compromise gut mucosal integrity.
References - Soler R, Macedo A Jr, Bruschini H, et al: Does the less aggressive multimodal approach of treating bladder-prostate rhabdomyosarcoma preserve bladder function? J Urol 174(6):2343n2344, 2005.
- Vijayalakshmi IB, Chitra N, Prabhu Deva AN. Use of a Amplatzer Duct Occluder for closing an aortico-left ventricular tunnel in a case of noncompaction of left ventricle. Pediatr Cardiol. 2004;25:77-9.
- Sivilotti L,Woolf CJ.he contribution of GABAA and glycine receptors to central sensitization: disinhibition and touch-evoked allodynia in the spinal cord. J Neurophysiol 1994;72:169-179.
- Gage J, Rutman H, Lucido D, LeJemtel TH. Additive effects of dobutamine and amrinone on myocardial contractility and ventricular performance in patients with severe heart failure. Circulation. 1986;74:367.
- Cullen DJ, Coyle JP, Teplick R, et al. Cardiovascular, pulmonary, and renal effects of massively increased intra-abdominal pressure in critically ill patients. Crit Care Med. 1989;17:118-121.
- Essed E, Schroeder FH: New surgical treatment for Peyronieis disease, Urology 25:582n587, 1985.
|

