|
Professor J Stewart Cameron - Emeritus Professor of Renal Medicine
- Elm Bank
- Melmerby
- Penrith
- Cumbria
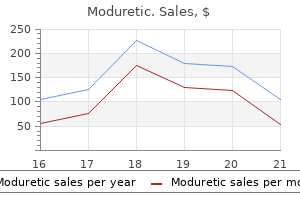
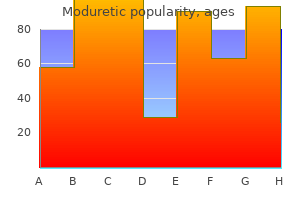
Moduretic dosages: 50 mg, 50 mg
Moduretic packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Discount 50mg moduretic otcPatients with renal pathology are also extra more likely to blood pressure medication brand names buy moduretic cheap have flank tenderness on the costovertebral angle than anterior stomach tenderness. A pelvic examination should be carried out in all ladies with lower belly ache to exclude adnexal tenderness from ovarian pathology. Chronic right ovarian pathology such as an enlarging cyst or neoplasm ought to be considered in ladies. Pyoderma gangrenosum appears as ulcerated pores and skin lesions and will happen unbiased of illness exercise. Left Lower Quadrant Pain the differential analysis entails: � � � � � � diverticulitis; left-sided colitis; appendicitis with malrotation; left renal pathology; left ovarian pathology; ectopic pregnancy. The vary of medical presentation varies from acute, extreme symptoms with sepsis and peritonitis, to continual, low-grade symptoms with extra benign findings on examination. All patients with possible diverticulitis must be questioned about prior colonoscopy and any symptoms of a colovesicular fistula such as persistent pneumaturia or faecaluria. Those with fever, tachycardia or hypotension along with localized peritonitis could have a diverticular abscess from a small, contained perforation. Those with shock and diffuse peritonitis are likely to have free colonic perforation with faecal peritonitis. Recent travel or contact with contaminated meals should increase a suspicion of Salmonella or Shigella an infection or amoebiasis. Ischaemic colitis should be considered in older patients with identified coronary or peripheral vascular disease. Pelvic examination will exclude left adnexal tenderness or masses which may be seen in cases of left ovarian torsion, tuboovarian abscess, left-sided ectopic being pregnant or left ovarian malignancy. These are often positioned along a line becoming a member of the umbilicus to the left anterior superior iliac backbone on the lateral border of the rectus sheath. Complications of colostomies include oedematous stomas, haemorrhage and ulceration from the divided finish, ischaemic stenoses, detachment of the cutaneous suture line, prolapse and paracolic hernias. Because of the acidic nature of the efflux, a spout is often common to stop pores and skin excoriation (a Brooke ileostomy). The technical complications of an ileostomy are much like those of a colostomy, however as properly as high output may lead to dehydration and electrolyte disturbance. Pelvic Pain the differential analysis of pelvic pain contains: � � � � � � � � diverticulitis; cystitis; ruptured bladder; ruptured haemorrhagic ovarian cyst; pelvic inflammatory illness; endometriosis; ovarian neoplasm; uterine neoplasm. Pelvic or suprapubic ache may be the preliminary presentation of a bunch of circumstances affecting the lower belly viscera. Although uncommon, a ruptured bladder might current with suprapubic ache in a patient with a history of latest alcohol intoxication with blunt trauma. With intraperitoneal rupture, irritation of the parietal peritoneum by urine produces diffuse rebound tenderness. Given the relative sterility of urine, the abdomen may be gentle without inflexible guarding upon early presentation. Women with pelvic pain may be suffering from considered one of many possible gynaecological situations. A historical past of unprotected intercourse or a number of sex partners together with adnexal tenderness or a purulent cervical discharge raises considerations of pelvic inflammatory illness. Young women with persistent cyclical pelvic ache, painful menstrual cycles, pain during sexual activity, ache with bowel movements or irregular bleeding may be suffering from endometriosis. This is common to divert the small bowel contents right into a bag and away from the adjoining pores and skin. Vaginal bleeding, an rising stomach girth, weight reduction and fatigue increase a suspicion of malignancy. Abdominal examination may reveal ascites and hepatomegaly if cumbersome liver metastases are present. Acute ischaemia from an arterial embolus in sufferers with atrial or ventricular thrombi or valvular lesions presents with sudden, extreme colicky mid-abdominal ache. Acute mesenteric venous thrombosis is seen in patients with an underlying hypercoagulable state or continual pancreatitis. Classically, sufferers with acute ischaemia initially have pain out of proportion to the actual tenderness discovered on examination. By distinction, patients with atherosclerotic lesions in at least two of the three main mesenteric arteries are more doubtless to experience persistent signs of postprandial ache leading to meals aversion, diarrhoea and weight reduction. Bowel Obstruction Transvaginal ultrasound is an excellent way to visualize the uterus and adnexae. Patients with diffuse belly ache in affiliation with stomach distension, nausea, vomiting and constipation might have an underlying small or large bowel obstruction. Faeculent-smelling emesis suggests a chronic stasis of enteric fluid inside dilated loops of bowel. Fluid loss through emesis and intraluminal secretions can lead to profound dehydration manifested by tachycardia, hypotension, lethargy and skin tenting. Patients with bowel obstruction often have a clearly distended abdomen with hyperactive or hypoactive bowel sounds, however it might be troublesome to assess for distension in overweight sufferers. Small bowel obstruction is most frequently due to adhesions from prior abdominal surgery or incarcerated hernias. Patients with out clear risk elements are presumed to have major small bowel obstruction from congenital bands, inside hernias or main small bowel tumours. There is marked tenderness over the loop while the remainder of the stomach is normally delicate and not notably distended. Adenomatous polyps in patients with Peutz�Jeghers syndrome may trigger intussusception or bleeding. Patients on anticoagulation might develop spontaneous intramural haematomas that can also cause intussusception. Infectious intra-abdominal processes such as diverticulitis or appendiceal abscesses might result in hypomotility of the adjacent small bowel leading to a segmental paralytic ileus. Although the circumstances discussed above should stay within the differential diagnosis for patients with this sort of generalized belly ache, the next circumstances should be given particular consideration: � � � � � � � � � � � � � � � � perforated viscus; haemoperitoneum; pancreatitis; mesenteric ischaemia; small bowel obstruction; intramural haematoma; large bowel obstruction; pseudo-obstruction; spontaneous bacterial peritonitis; peritoneal dialysis catheter-associated peritonitis; right heart failure; carcinomatosis; gastroenteritis; constipation; urinary retention; medical circumstances. Severe and sudden-onset generalized belly ache is the preliminary complaint in many surgical abdominal circumstances. Fever, tachycardia or hypotension, and a agency stomach with diffuse board-like guarding and absent bowel sounds raises considerations of peritonitis from bowel perforation. Perforated duodenal ulcer, diverticulitis and colon cancer are the more than likely prospects in aged patients. Less incessantly, appendicitis may result in the unfold of purulent content within the abdomen, leading to diffuse guarding. Patients with haemoperitoneum from blunt or penetrating trauma or ruptured vascular tumours corresponding to hepatocellular carcinoma or hepatic adenoma, may also exhibit board-like belly wall rigidity.
Buy generic moduretic 50 mg on lineA flat incision is made posterior to the tibial tubercle arteria epigastrica cranialis superficialis commissura labiorum dorsalis 50mg moduretic with amex, tapered anteriorly at its distal extent such that solely about 1 mm of bone is left on the distal tip of the osteotomy and the proximal minimize is made about 2 mm above the patellar tendon insertion. This proximal cut should be made in such a method that the tibial tubercle could additionally be freely moved medially, ie, in order that the medial facet of the proximal cut is extra proximal than the lateral side of the proximal minimize, open medially. In patients with a severe dysplasia requiring greater than 1 cm of medialization, a deeper reduce might be required. In sufferers requiring 1 cm of medialization, a proximal tibial tubercle thickness of 1 to 1. Care should be taken to taper this osteotomy anteriorly at the distal extent of the cut to permit for straightforward greenstick fracturing of the tip of the osteotomy to move the tubercle medially. Completion of the Transfer After the osteotomy has been completed with an oscillating saw, the proximal minimize normally is made with a 1/2-inch osteotome. Care should be taken to not enable the cortical screw tip to protrude any more than necessary beyond the posterior cortex. The surgeon releases the lateral retinaculum both arthroscopically or by open surgical procedure to achieve the needed stability of the extensor mechanism upon tibial tubercle transfer. Tracking of the patella within the central trochlea should be confirmed arthroscopically or brazenly after the tibial tubercle transfer. After isolating the patellar tendon, the anterior tibialis muscle is released and mirrored posteriorly. Because an indirect osteotomy shall be made from medial to lateral, a big retractor should be positioned to retract the anterior tibialis muscle laterally to view the saw making the osteotomy reduce because it exits on the posterolateral aspect of the tibia. For anteromedial tibial tubercle switch, the cut proceeds obliquely from medial to lateral, tapering toward the anterior crest distally. After transferring the tibial tubercle along the osteotomy (C), both anteriorization and medialization of the tibial tubercle are achieved (D). The osteotomy usually extends from the level of the tibial tubercle to a level of about 7 to 9 cm distally on the tibia and once more should exit on the degree of the anterior cortex of the tibia to avoid a large fragment distally. Making a deep reduce distally increases the risk of tibia fracture; this ought to be averted. This technique avoids damage to the anterior tibial artery and deep peroneal nerve, that are around the posterolateral nook of the tibia posteriorly. Once the proximal extent of the minimize has reached the level of the mid to posterior portion of the lateral tibia cortex, it ought to be stopped on the lateral side. An osteotome or noticed then is used to make a back reduce from the corner of the proximal lateral nook of the osteotomy up to a degree proximal to the patellar tendon laterally. This permits for launch of the lateral cortex when the osteotomy has been completed, and the osteotomized fragment shall be displaced anteromedially. The third minimize for anteromedial tibial tubercle transfer is instantly proximal to the patellar tendon insertion on the tibia, about 2 mm above the patellar tendon insertion. This cut often is made with a 1/4- or 1/2-inch osteotome under direct imaginative and prescient utilizing an Army-Navy retractor to hold the patellar tendon anteriorly. It is best made from medial to lateral and connects the proximal extent of the medial osteotomy reduce to the oblique back cut on the lateral aspect so that the osteotomy is now free to displace anteromedially. It is moved anteromedially by greenstick fracturing the anterior cortex distally, which must be not extra than 1 to 2 mm thick at its distal extent. The osteotomized fragment is moved about 1 cm but could also be moved barely more, as needed, to obtain extra anteriorization or medialization. Thus, this osteotomy is custom-made for every affected person, relying on the particular need. Completion of the Transfer the osteotomized fragment is mounted securely with two cortical lag screws. If probably the most proximal minimize has been made fastidiously, there shall be a ledge of bone on which the osteotomized fragment will relaxation, which is able to add stability to the osteotomy beyond what the screws offer. In sufferers with any retropatellar tendon contracture, this tendon also is launched to release the extensor mechanism. After tibial tubercle transfer, hemostasis should be meticulous, and then the subcutaneous tissue and pores and skin are closed. Smoking must be stopped before surgery and never resumed for no much less than 2 months due to its opposed effect on bone healing. All sufferers should obtain some form of postoperative anticoagulation, and will have prophylactic antibiotics on the time of surgical procedure. Hemostasis should be meticulous, and correct drainage of hematoma applied as needed. Patients are kept on crutches for 6 to eight weeks and resume weight bearing as tolerated after 6 weeks. During the preliminary 6 weeks, we suggest toe-touch or gentle weight bearing on the affected facet. We recommend anticoagulation with aspirin for a minimum of 4 to 6 weeks for many sufferers. Most of our patients go residence from same-day surgery and are seen in 1 to 3 days as wanted and then for suture removing and radiographs at 10 to 12 days. Steri-strips are applied and stored in place for four to 6 weeks to minimize wound spread. Our follow-up studies have persistently revealed a satisfactory outcome in 85% to 90% of patients. Patients with lateral and distal patellar lesions are more likely to experience aid than sufferers with proximal (dashboard) or medial (s/p dislocation) lesions. The use of scintigraphy to detect elevated osseous metabolic activity about the knee. Anteromedialization of the tibial tubercle for treatment of patellofemoral malpositioning and concomitant isolated patellofemoral arthrosis. Histologic evidence of retinacular nerve injury associated with patellofemoral malalignment. Correlation of patellar articular lesions and outcomes from anteromedial tibial tubercle switch. Anterior tibial tubercle transposition for patellofemoral arthrosis: a long-term research. Fracture of the proximal tibia with quick weightbearing after a Fulkerson osteotomy. Acute compartment syndrome usually is as a outcome of of trauma to , or reperfusion of, the extremity. Both acute and continual compartment syndromes are due to increased interstitial stress inside a compartment, leading to decreased perfusion and ischemia of soft tissues. Clinical manifestations of exercise-induced pain relieved by relaxation, swelling, numbness, and weak point of the extremity have lengthy been attributed to elevated intracompartmental pressures.
Diseases - Biemond syndrome
- Ovarian dwarfism as part of Turner syndrome
- Hypopituitarism postaxial polydactyly
- Trichomegaly cataract hereditary spherocytosis
- Onychophosis
- Long QT syndrome type 2
- Trypanosomiasis, East African
Buy moduretic 50 mg free shippingOn a real lateral radiograph zicam and blood pressure medication buy cheap moduretic line, trochlear dysplasia is evident when the floor of the trochlea crosses the anterior borders of both femoral condyles (ie, the "crossing" sign). Measurement of the trochlear prominence on the lateral view in accordance with Dejour et al. X and Y are strains tangential to the anterior and posterior cortices of the distal femoral metaphysis, respectively. Line Z crosses probably the most outstanding point of the line of the trochlear groove (point B) and the upper facet of the posterior border of the condyles. Line Z crosses the anterior side of the lateral condyle (point A) and line X (point C). Note that the floor of the trochlea lies anterior to the road tangential to the anterior cortex of the distal femur. Partial harm, with surrounding edema, to the midsubstance of the patellar retinaculum (open arrow) is also seen. A full tear (open arrow) is seen in the patellar insertion of the medial patellar retinaculum. A giant joint effusion with layering (black arrows) is present, in preserving with hemarthrosis. Plain radiographs ought to be reviewed for the presence of trochlear dysplasia (ie, crossing signal and trochlear prominence of three mm or more), avulsion fractures, and free our bodies. Offset of 20 mm or more should be treated with medialization of the tibial tubercle. The patella should displace more than 10 mm laterally from the centered place with the knee flexed 30 degrees, and there must be a delicate endpoint or no endpoint with the knee prolonged. Randomized prospective studies evaluating operative and nonoperative treatment of preliminary patellar dislocation found no profit from instant medial retinacular restore. As a result, nonoperative administration depends on brace protection throughout early progressive moblization and useful rehabilitation. After an acute dislocation, patients initially are positioned in knee immobilizers for consolation and weight bearing as tolerated. Patients are inspired to proceed sporting the patellastabilizing brace throughout participation in pivoting activities and sports. Surgical management often is indicated for any patient with at least two documented patellar dislocations and a bodily examination demonstrating extreme lateral patellar laxity. A superolateral portal is used to facilitate viewing of the patellar articular surface and passive patellar monitoring and mobility. Specifically, the patellofemoral compartment is assessed for the severity of articular cartilage harm and the presence of degenerative changes. After dissection through the subcutaneous tissue, the superficial medial patellar retinaculum (layer 1) is identified. The deep synovial layer (layer 3) can be dissected off the deep floor of the ligament to aid in inspection. The knee is then flexed to 30 levels with the patella manually lowered within the trochlear groove. With the knee extended, a laterally directed drive should reproduce a agency endpoint ("check rein" sign). Patellar mobility is assessed by making use of medial and lateral forces of about 5 kilos with the knee flexed to 30 levels. If lateral displacement is less than 5 mm or greater than 10 mm, then the medial repair is retensioned. Alternatively, the origin could also be approached through a separate posterior incision centered between the medial epicondyle and the adductor tubercle. The dissection is carried down by way of the subcutaneous tissue, and the injured medial retinacular tissue is recognized. Augmented restore of avulsion-tear kind medial patellofemoral ligament damage in acute patellar dislocation. Identify and isolate each the gracilis (proximal) and semitendinosus (distal) tendons from their deep aspect, ie, from inside the bursal layer. Apply pressure to the semitendinosus while freeing it from the crural fascia at the posteromedial corner with tissue scissors. Once all tendinous slips have been freed, harvest the semitendinosus tendon utilizing a closed (preferred) or open tendon stripper. Baseball stitches are positioned on each free ends for later graft passage throught the 2 patellar tunnels. The graft is ready on the back table by first sizing the graft to 240 mm, then folding it in half, leaving a doubled graft of 120 mm. Patellar Tunnel Placement A longitudinal incision the length of the patella is made on the junction of the medial and center thirds of the patella (in line with the medial border of the patellar tendon on the distal patellar pole). The medial eight to 10 mm of the patella is uncovered by subperiosteal dissection with a no. Again, a corresponding drill gap is placed on the anterior floor of the patella about 8 mm from the medial border, and the 2 holes are related with a curved curette. The knee is flexed barely to facilitate palpation of this landmark (flexion strikes the hamstrings posteriorly away from the medial epicondyle). If the affected person is obese and the landmarks are tough to palpate, a small pores and skin incision is made and palpation is finished via the wound to identifty the ridge. Using an extended, curved clamp, the chosen interval is developed (again, preferably between layers 2 and 3) from the patellar incision anteriorly to the medial femoral epicondyle posteriorly. With the tip of the clamp overlying the ridge between the medial epicondyle and adductor tubercle, layers 1 and a pair of are incised using a no. The tip of a Beath pin is positioned at a degree 9 mm proximal and 5 mm posterior to the medial epicondyle; the pin is then passed toward the lateral facet of the femur. If lengthening happens in flexion, a second Beath pin is positioned more distally towards the medial epicondyle. The first pin is left in place to facilitate repositioning whereas drilling the second Beath pin. If lengthing occurs in extension, a second Beath pin is placed extra proximally towards the adductor tubercle. Again, the first pin is left in place to facilitate repositioning while drilling the second Beath pin. Once the femoral pin website is accepted, a blind tunnel is reamed into the femur the size of the doubled graft. The femur is reamed to a depth of no much less than 20 mm, with a most popular depth of 25 mm. Fixation to the femur could additionally be achieved reliably with a 20-mm absorbable interference screw. The free graft arms are passed individually by way of their respective patellar tunnels using double 22-gauge chrome steel wire or a curved suture passer. The free graft arms are then doubled again and sutured on themselves just medial to the patella using two determine 8 mattress sutures of no. After correct placement of the femoral attachment web site is confirmed using the isometry suture, the semitendinosus graft has been fastened to the femur utilizing an interference screw. The isometry suture is used to shuttle the graft anteriorly out the medial patellar incision.

Purchase moduretic 50mg on lineThe anterior cruciate ligament is well visualized on the left pulse blood pressure relationship order moduretic toronto, with the posterior cruciate ligament on the proper more obscured by fat and synovial tissue. The posterior horn of the lateral meniscus, the posterior lateral femoral condyle, the posterior meniscal root, and the capsular attachment are visualized. Shoulder arthroscopy instrumentation and cannula techniques may be helpful with more advanced surgical procedures as nicely. The surgeon ought to talk to the affected person earlier than the surgery and carry out an examination underneath anesthesia to confirm the pathology necessitating surgical procedure. D�bridement of those structures will improve postoperative ache and extend rehabilitation. High pump pressures can lead to fluid extravasation into the soft tissues, resulting in the potential for compartment syndrome. The surgeon may need to consider gravity inflow or lower pump pressures in such conditions. Older sufferers usually have a tendency to maintain an harm to the collateral ligaments when varus or valgus stresses are utilized to gain compartment visualization. Some sufferers have ligamentously tight knees, making it difficult to reach the posterior aspect of the medial and lateral tibiofemoral compartments. The surgeon should use all portals available, together with the far medial and lateral as properly as the posteromedial and posterolateral portals, to properly handle the pathology. Regardless of suture sort or technique, the surgeon should acquire a decent closure. Intra-articular and portal injection of local anesthetic may help with postoperative ache administration. Deep vein thrombosis prophylaxis could additionally be accomplished with a compression dressing from the toes to the thigh, elevation, mobilization, and ankle pumps. Regardless of postoperative weight-bearing status, most sufferers will require crutches for mobility. Cryotherapy has been proven to improve ache scores after knee arthroscopy and is recommended. Complications of arthroscopy and arthroscopic surgery: results of a national survey. Incidence of deep vein thrombosis after arthroscopic knee surgery: a potential examine. The synovial lining undergoes hyperplasia, most prominent in rheumatoid arthritis. Synovitis secondary to inflammatory situations can lead to painful, swollen, and stiff knees. After medical administration has been exhausted, surgery is indicated if the patient experiences continued pain, swelling, and mechanical symptoms. In rheumatoid arthritis, the cervical backbone is commonly involved and should be evaluated earlier than surgical intervention. Also, the disease is commonly not restricted to the musculoskeletal system: sufferers can also have vasculitis, subcutaneous nodules, and pericarditis. During the bodily examination the surgeon ought to search for effusion, tenderness, warmth, mass, and synovial thickening. Lachman check: assesses competence of anterior cruciate ligament Posterior drawer test: assesses competence of posterior cruciate ligament Varus stress take a look at: assesses competence of lateral collateral ligament Valgus stress take a look at: assesses competence of medial collateral ligament Malalignment and ligamentous insufficiencies are famous and can probably preclude arthroscopic synovectomy, given their association with joint destruction. Normal synovium supplies vitamins for the articular cartilage and produces lubricants that bathe the joint surfaces to permit easy gliding. Histologic hallmarks of chronic synovitis embrace hyperplasia of the intimal lining, lymphocyte infiltration, and blood vessel proliferation. Patients with chronic synovitis can have localized or diffuse illness, depending on their underlying situation. It presents as an insidious onset of morning stiffness with multiple joint involvement. The synovitis that ensues is probably going an acute autoantibody-mediated inflammatory response. Hemophilia is an X-linked deficiency of clotting elements, resulting in bleeding of varying severity. The repeated hemarthroses can lead to a continual, progressive synovial hyperplasia. It can reduce the variety of recurrences and will gradual the progression of joint arthrosis. Appropriate medical clearance is important to maintain perioperative issues to a minimal. General anesthesia rather than native anesthesia is really helpful as a end result of the process can be lengthy. An epidural may be used when medically indicated and may help in postoperative pain relief. The surgeon ought to look for the attribute rheumatologic signs of periarticular erosions and osteopenia. Advanced degenerative disease is associated with a poorer prognosis after arthroscopy. Positioning the patient is placed supine and brought to the sting of the mattress to be positive that the leg could also be simply hung over the facet. The contralateral leg is positioned in a well-padded leg holder, flexing the hip and knee, with the hip in slight abduction. The mattress can be flexed to produce slight hip flexion, lowering the possibility of femoral nerve palsy that could be associated with excessive hip extension and leg traction. Oral anti-inflammatory drugs could also be used, in addition to intra-articular corticosteroid injections. The arthroscope is placed into the suprapatellar pouch with the knee in extension. Arthroscopic view reveals establishment of the superolateral working portal beneath direct visualization. Retropatellar Pouch, Inferolateral and Inferomedial Gutters Intercondylar Notch the arthroscope is moved to the superolateral portal and the shaver is positioned within the inferolateral portal. This establishes enough working area throughout the notch to allow visualization of the posterior compartments of the knee. The arthroscope is moved to the superolateral portal, and the shaver is positioned in the inferolateral portal. The arthroscope is moved to the inferomedial portal, and the shaver is placed in the inferolateral portal. The arthroscope is returned to the inferolateral portal, and the shaver is in the inferomedial portal. Posteromedial Compartment For entry to the posteromedial compartment, a blunttipped trocar is positioned in its arthroscopic sheath and inserted through the inferolateral portal. Alternatively, a switching stick may be placed through the inferolateral portal under direct visualization with the arthroscope placed in the inferomedial portal.
Generic moduretic 50 mg without prescriptionAbdominal examination might initially be very unimpressive prehypertension 135 generic 50 mg moduretic visa, with a soft but very tender mid-abdomen. Stools testing optimistic for occult blood or bloody diarrhoea could additionally be current in some sufferers. When full-thickness gangrene is creating or bowel perforation occurs, signs of peritoneal irritation become manifest. Mesenteric venous thrombosis happens in sufferers with underlying inherited hypercoagulable states or portal hypertension, in ladies utilizing oral contraception or because of intra-abdominal an infection. The resistance to venous outflow and creating bowel oedema might result in a diminished arterial circulate. The signs are sometimes less acute than in patients with acute arterial occlusion. Although slower to progress, mesenteric venous occlusion could result in large necrosis of the small bowel. An increased lactic acid stage, although not specific, and leukocytosis ought to improve the suspicion of mesenteric ischaemia. The presence of gasoline inside the intestinal wall (pneumatosis intestinalis) is sometimes seen in a quantity of benign conditions. Ischaemic Colitis Ischaemic colitis develops secondary to a period of an insufficient move through the colonic arteries. It is mostly non-occlusive and occurs in sufferers with associated medical comorbidities or accompanies the acute sickness. The splenic flexure and caecum have a decreased collateral network and hence a poor tolerance to hypoperfusion. Non-occlusive colonic ischaemia occurs in periods of global hypoperfusion: myocardial infarction, cardiopulmonary bypass, haemodialysis and shock. Ischaemia of the left colon is a known complication of aortic surgery and is expounded to an interruption of the collateral flow. Abdominal Aortic Emergencies 603 poor capacity of the vasculature to meet the metabolic calls for of the colon. Ischaemic colitis might happen in healthy younger individuals as a outcome of vasospasm because of excessive train or illicit drug use (cocaine, amphetamines). A small amount of bloody diarrhoea develops with in the first day of onset of the ache. Abdominal tenderness is located over the affected phase, often lateral to the umbilicus. Most sufferers get well within a quantity of days with conservative administration, normalization of the collateral move and backbone of the precipitating occasion. Healing in more severe instances may end in obstructing strictures of the affected areas. In some cases (more commonly in the best colon), acute ischaemia progresses to full-thickness necrosis and subsequent perforation. The term implies the presence of a particular disease with various microscopic and macroscopic changes. Peritonitis most commonly results from pathology of the adjoining organs (secondary), as described in the previous sections, and is only hardly ever a primary illness. Peritonitis is assessed as infectious (bacterial, fungal, hydatid disease) or non-infectious. Depending on their chemical properties, the leak of sterile fluids (bile, gastric contents, blood, urine, pancreatic fluid, the contents of an ovarian dermoid cyst) into the peritoneal cavity results in inflammation and ache. Talc peritonitis from chemical irritation and fibrosis is now not seen as talc is now not utilized to surgical gloves. Secondary bacterial peritonitis is by far the commonest kind and usually results from spontaneous, traumatic or iatrogenic perforations of the gastrointestinal tract (the most common aetiologies are discussed individually in this chapter). The severity of the an infection is determined by the nature of the illness and on patient-related components. Depending on the extent of the contamination and the ensuing infection, the peritonitis could also be focal or diffuse. Contamination and an infection stimulate an inflammatory response that in early stages leads to fibrin deposition. The ensuing adhesions of the greater omentum and adjacent organs, and adhesions from prior operations, could contain the world of spillage and seal the perforation. The severity of the disease and its clinical manifestations also rely upon the period of the infection, the character of the contaminants and the focus and virulence of the organisms involved. Faecal peritonitis ends in a serious systemic inflammatory response because of high counts of gram-negative rods and anaerobes. Even initially sterile or nearly sterile peritonitis (bile, pancreatic, gastric) becomes secondarily contaminated as the time progresses. Spilled solid particles are harder for the peritoneal immune system to clear. When the aortic diameter reaches 6 cm, the risk of rupture is roughly 20 per cent per year. Primary peritonitis (usually streptococcal) may also be seen in youngsters with nephrotic syndrome. In ladies, the fallopian tubes could serve as an entry point for an infection of the peritoneal cavity. The alkaline vaginal milieu in prepubertal ladies might predispose to pneumococcal spread, and the resulting acute peritonitis might mimic appendicitis. Ascending gonococcal or chlamydial infections in adults lead to perihepatitis (Fitz-Hugh�Curtis syndrome), which presents with right upper quadrant pain. Interestingly, in some patients the first cervicitis and salpingitis may not be clinically distinguished. Ascending transfallopian non-specific bacterial an infection (pelvic inflammatory disease) may also occur in women using intrauterine units. The pain is constant and exacerbated by motion of the abdominal wall, corresponding to in strolling and coughing. In diffuse peritonitis, sufferers scale back the amplitude of their respiratory actions to restrict the irritation. A paralytic ileus invariably follows intra-abdominal infection and is proportional to its severity. Signs of peritoneal irritation are current over the areas affected by the peritonitis. The manifestations of the systemic inflammatory response and organ failure progress together with the disease: fever, tachycardia, hypotension, oliguria and adjustments in mental standing. This is an autosomal recessive disorder occurring primarily in the descendants of ethnic teams who originated from the Mediterranean region. The illness manifests by recurrent assaults of fever and inflammation of the serosal surfaces. The first assault happens in childhood in most sufferers, and by the tip of the teenage years in almost all sufferers.
Syndromes - What other symptoms or abnormalities are present?
- Pregnancy
- Pulmonary fibrosis (scarring of the lung)
- Birth control pills
- Hematin given through a vein (intravenously)
- Several days before surgery, you may be asked to stop taking drugs that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), clopidogrel (Plavix), warfarin (Coumadin), naprosyn (Aleve, Naproxen), and other drugs like these.
- Blood culture

Generic moduretic 50 mg fast deliveryThe complete contents of the scrotum arrhythmia practice strips buy online moduretic, including the testes, epididymides and twine structures, need to be examined individually and assessed for their presence and normality. If a mass is found in the scrotum, five key questions ought to be answered: � Is it potential to palpate above the mass. A haematocele is a collection of blood with the tunica vaginalis and usually results from blunt or sharp trauma to the exterior genitalia. The testes range in dimension between people and to a lesser diploma inside people. Testicular Maldescent � In a toddler, it is necessary to confirm the presence of two testes. Over 70 per cent of cryptorchid testes will spontaneously descend by 3 months, and at 1 year of age the incidence of cryptorchidism is approximately 1 per cent. The testis can even lie in an ectopic place exterior the road of normal descent. Torsion of the Spermatic Cord Torsion of the twine needs to be considered in all patients who current with acute scrotal signs. Patients usually present with acute and extreme testicular ache that radiates to the inguinal area. The absence of a cremasteric reflex is an effective signal of torsion of the twine however is often tough to assess due to extreme pain. The testicular salvage rate for surgical detorsion is ninety per cent if carried out within 6 hours of symptom onset, but only 50 per cent after 12 hours and 10 per cent after 24 hours. Adolescents sometimes present with a historical past of intermittent episodes of severe scrotal pain which have resolved spontaneously. These features are in keeping with wire torsion with spontaneous detorsion and are greatest managed by elective scrotal exploration and bilateral testicular fixation. Torsion of the Testicular and Epididymal Appendages Torsion of the appendix testis and appendix epididymis can current with variable symptoms ranging from mild scrotal discomfort to severe ache indistinguishable from torsion of the wire. In the initial section, the ache could also be localized to the higher pole of the testis or epididymis, where a young nodule could additionally be palpable. If scrotal exploration is performed for clinical uncertainty, the torted appendage can be excised. They transilluminate and, when small, are straightforward to differentiate from different scrotal pathologies. Most cysts are asymptomatic, however as they enlarge the affected person may complain of discomfort or a feeling of heaviness in the scrotum. Large epididymal cysts can mimic a hydrocele and are often only differentiated on ultrasound examination or during surgery. The Epididymis and Vas the epididymis is palpable behind the body of the testis and is steady with the vas, which passes inside the spermatic cord. Agenesis of the vas is associated with cystic fibrosis and absence of the epididymis and/or the seminal vesicles, as properly as with renal anomalies, including renal agenesis. The cysts are sometimes positioned within the A varicocele is a dilatation of the veins of the pampiniform plexus inside the spermatic wire. It happens in roughly 15 per cent of male adolescents and as a lot as 30 per cent of males investigated for infertility (it stays controversial whether or not varicoceles cause oligospermia). Approximately ninety per cent of varicoceles are leftsided, attributable to elevated venous strain in the inner spermatic vein (as the left drains into the left renal vein and the right drains into the vena cava), collateral venous anastomoses and absent or incompetent valves in the veins. Occasionally, they present with a uninteresting ache in the scrotum, exacerbated by prolonged standing or bodily exercise. Examination must be carried out with the patient each standing and supine and with and without a Valsalva manoeuvre. Renal injuries are usually because of blunt trauma sustained in street traffic accidents, sports accidents, falls and assaults. Penetrating injuries can occur with gun photographs and stab wounds, and through surgical and percutaneous procedures. Minor injuries to the kidney embrace contusions and small lacerations, while more vital and probably life-threatening accidents involve the renal vessels or a shattered kidney. Pre-existing renal abnormalities improve the chance of and complicate the outcome of kidney trauma. The initial precedence in the assessment and management of any trauma affected person consists of securing the airway, controlling exterior bleeding and resuscitation of shock. During the stabilization section, a radical physical examination ought to include in search of indicators of urogenital damage. The scientific findings could include a penetrating wound within the flank, higher stomach or lower chest, and if the patient has been shot, there may be an exit as nicely as an entry wound. It is necessary to not underestimate the degree of inner injury on the idea of a small penetrating injury wound. Signs associated with blunt renal injury could include haematuria associated with flank bruising, tenderness and swelling. Blood within the ureter and bladder could clot, producing clot colic, which characteristically occurs 2�5 days after damage. Rarely in major renal injury, the renal pedicle could additionally be avulsed, the pelviureteric junction disrupted or a segmental artery thrombosed, and the affected person might not exhibit haematuria. External harm can be penetrating or blunt, with gun shot wounds accounting for over ninety per cent of instances, and stab wounds and blunt trauma together accounting for lower than 10 per cent of accidents. Ureteric trauma extra commonly outcomes from iatrogenic injury, particularly abdominopelvic surgical procedure and ureteroscopy. The ureter may be divided, crushed, devascularized, ligated, excised or perforated. The majority of iatrogenic accidents are recognized postoperatively and current with flank ache, fever, sepsis, prolonged ileus or often renal failure. On bodily examination, there may be a tender flank mass secondary to a urinoma, signs of peritionitis or urine leakage from the wound or vagina. The superior surface of the bladder is covered by peritoneum, which in males passes down the posterior floor of bladder earlier than being mirrored onto the anterior facet of the rectum to form the rectovesical pouch. In females, the peritoneum reflects from the posterior bladder wall onto the physique of the uterus, forming the vesicouterine pouch. The risk of bladder harm is related to the diploma of bladder distension, a full bladder being extra susceptible to rupture than an empty one. Traumatic extraperitoneal bladder injuries are usually associated with pelvic fractures, leading to direct perforation by a bony fragment, a compression burst injury or laceration by shear forces. Pelvic damage may end up in simultaneous trauma to the bladder and posterior urethra. Bladder resection of the dome, the thinnest a part of the bladder wall, also can end in an intraperitoneal harm. This is often recognized intraoperatively and requires a laparotomy to close the bladder wall defect.
Discount moduretic 50 mg visaThe surgeon should work expeditiously; sufficient arthroscopic abilities blood pressure normal value buy discount moduretic 50 mg online, including suture passage and knot tying, are required. All anticipated devices should be open on the again desk firstly of the process. Suture limbs must be handed slowly and underneath visualization to permit for corrections. A looped suture-passing device is best used with two cannulas: one to move the loop and a second to retrieve the loop and thread the supposed "post-limb" suture. If one cannula has one of the best angle of approach for suture passage, a tissue-penetrating retriever is used to pierce the tissue and retrieve the suture via the same cannula to avoid tangling. An assistant ought to level and stabilize the cannula at the anchor to simplify tying. The surgeon should be taught and turn out to be proficient with one sliding and one nonsliding knot. A two-hole knot pusher (Arthrex) is beneficial for cinching the limbs down and untwisting the limbs throughout successive throws. Starting at 1 week, self-directed range-of-motion exercises are begun underneath specific guidelines (see below). Patients are seen often to assess progress and modify rehabilitation as needed. Immediate Passive external rotation with arm at facet (not abduction) inside specific parameters Elbow flexion and extension Capsulotomy sufferers are began on "sleeper" stretches on postoperative day 1. Weeks 1 to three Pendulum workout routines Passive vary of motion using pulley system in ahead flexion and abduction to 90 levels only Start shoulder shrugs and scapular retraction workout routines in sling. Passive vary of movement is advanced to full motion in forward flexion and abduction. Strengthening for rotator cuff, scapular stabilizers, and deltoid is began at 6 weeks. The disabled throwing shoulder: spectrum of pathology, part I: pathoanatomy and biomechanics. A cadaveric mannequin of the throwing shoulder: a potential etiology of superior labrum anterior-to-posterior lesions. Stiffness can be addressed successfully with modification of the Chapter 7 Arthroscopic Treatment of Biceps Tendonopathy J. Pathology of the lengthy head of the biceps tendon presents in a spectrum from delicate tendinopathy noticed on diagnostic imaging research to frank tearing or subluxation appreciated intraoperatively. Because the practical significance of the biceps tendon long head has been the subject of considerable debate, therapy has usually been tailor-made extra to affected person symptoms, activity ranges, and expectations rather than strict operative standards. The best indications and optimum operative method remain controversial, though latest advances in arthroscopic expertise have led to an evolution of surgical methods. Multiple anatomic variants of the long head biceps tendon origin have been described, the most typical of which includes an equal contribution from the anterior and posterior labrum. The bicipital groove has been a subject of great study in the literature for its relevance to arthroplasty and it has been implicated as a contributing factor to tendinopathy involving the lengthy head of the biceps. Some authors have advocated a role of the long head of the biceps in contributing to shoulder stability in overhead athletes. Arthroscopic view of lengthy head of biceps tendon and proximal facet of bicipital groove. Patients with high-grade tendinopathy, both in isolation or in affiliation with cuff tears, appear to be vulnerable to subsequent rupture. Lesions of the pulley complicated (which contributes to stability of the tendon inside the intertubercular groove) or tears of the higher subscapularis tendon could allow intra-articular subluxation and mechanical symptoms. Patients may complain of anterior shoulder pain exacerbated by resisted elbow flexion and supination. The historical past and character of shoulder pain is much less helpful in making the analysis than the suitable physical examination and diagnostic imaging findings in a related context. Biceps tendon issues can present either in isolation or in association with other pathology, usually tears of the rotator cuff. Physical examination findings are variable however sometimes embody focal tenderness to palpation over the course of the biceps long head within the bicipital groove. Active compression test: Primarily assists in differentiating between symptomatic superior labral pathology and acromioclavicular joint pathology. A optimistic end result may suggest biceps tendinopathy in the applicable scientific context. Despite these recommendations, few research have corroborated the sensitivity, reliability, or accuracy of these findings. For the analysis of subluxation or dislocation of the long head of the biceps, ultrasound has a reported sensitivity of 96% to one hundred pc and specificity of 100 percent. Ultrasound is most helpful to show pathology within the intertubercular groove and has been proven to be extremely operator-dependent. Alternative nonoperative management of suspected biceps pathology includes exercise modification, a course of nonsteroidal anti-inflammatory medication, and corticosteroid injections focused directly into the biceps sheath inside the intertubercular groove. Long head biceps ruptures historically have been treated with nonoperative management, based on the perception that this downside not often leads to any significant impairment. With respect to tendon involvement, nonscientific relative surgical indications embody symptomatic partial-thickness tearing or fraying higher than 25% to 50% of its diameter, or tendon subluxation or dislocation from its normal position within the bicipital groove. Because the biceps tendon is a identified "pain generator," its evaluation and inclusion in therapy of cuff problems is particularly essential. Preoperative consideration should be given to anticipate operative strategies if encountered. Operative options in treating biceps tendon disorders include d�bridement, tenolysis (release of the biceps tendon lengthy head), and tenodesis, by which the biceps is reattached to either bone or delicate tissue of the proximal humerus. The chosen surgical strategy should take into accounts affected person factors, intraoperative findings, and surgeon choice and comfort. Patient components embrace age, work, leisure and activity demands, expectations, and perspective on influence of cosmesis. Intraoperative findings affect decision making in a quantity of ways, including bone quality, soft tissue high quality, the presence of harm to the biceps sling or subscapularis, and the presence of instability. Surgeon elements embody arthroscopic proficiency and experience and concomitant surgical procedures which will influence the remedy approach (eg, swelling in the subacromial house during concomitant arthroscopic rotator cuff repair). Few studies have compared surgical alternatives within the similar inhabitants of patients. The ideal indications for d�bridement versus tenolysis versus tenodesis (soft tissue or bone) stay unclear presently. Arthroscopic d�bridement is an initial element of nearly every biceps tendon surgical process. The degree of tendon involvement requiring definite surgical administration with both tenolysis or tenodesis has not been scientifically established within the literature and varies relying on concomitant pathology.

Discount 50 mg modureticThe saphenous vein and nerve are identified within the subcutaneous tissue and retracted anteriorly blood pressure quick reduction buy moduretic 50mg fast delivery. The opening between the origins of the flexor hallucis longus and the tibialis posterior is enlarged if constrictive. An 8- to 10-cm vertical incision is made over the midportion of the leg roughly 1 cm posterior to the posteromedial edge of the tibia. Dissection is carried down by way of the subcutaneous fats and superficial fascia until the deep fascia overlying the muscle is visualized. The sheath is eliminated and the balloon is inflated to create a cavity within the fascial cleft. A one-way cone-shaped cannula is inserted in the pores and skin on the site of balloon insertion. The optical cavity between the superficial and deep fascial layers may be maintained subsequently with 15 mm Hg of carbon dioxide insufflation to enable enough visualization of the fascia to be released and to permit adequate house to perform gentle tissue dissection with the endoscopic equipment. Next, the fascia is released with endoscopic scissors all the way down to the extent of the ankle underneath direct vision. If necessary, a distal instrument portal with a pneumatic lock can be positioned, however the fasciotomies often are carried out proximal to distal by way of the initial portal. The wound is closed in a two-layer trend with 2-0 Vicryl for the deep layer and a operating subcuticular sew for the pores and skin over a medium Hemovac drain. Identify the buildings in the subcutaneous tissue on the medial aspect of the leg. Avoid excessive traction on the saphenous nerve, which results in a traction paresthesia. Extend lateral and anterior fasciotomies to 4 to 6 cm above the ankle and posterior fasciotomies to eight to 10 cm above the ankle. Crutches can be utilized as wanted within the preliminary postoperative interval, however sufferers are inspired to bear weight as tolerated and carry out mild actions. Chronic exercise-induced compartment strain elevation measured with a miniaturized fluidpressure monitor. Chronic exertional compartment syndrome: the controversial "fifth" compartment of the leg. Fatal rhabdomyolysis with bilateral gluteal, thigh, and leg compartment syndrome after the Army Physical Fitness Test. Endoscopically assisted fasciotomy: description of method and in vitro assessment of lowerleg compartment decompression. The wick catheter method for measurement of intramuscular stress: a new research and clinical tool. Modified criteria for the objective prognosis of persistent compartment syndrome of the leg. Intramuscular pressure, muscle blood circulate, and skeletal muscle metabolism in continual anterior tibial compartment syndrome. The anterior and the lateral compartment syndrome of the leg due to intensive use of muscular tissues. Slimmon et al reported on long-term follow-up of sufferers handled with fasciotomy with partial fasciectomy and famous a good or wonderful consequence in 60% at a mean follow-up of fifty one months. Thirteen of sixty two had decreased activity levels as a outcome of recurrence of symptoms or improvement of a unique lower extremity compartment syndrome. Some authors have postulated that failure of the fasciotomy could also be due to an incomplete fasciotomy or not figuring out and releasing the fascia around the tibialis posterior. Compartment strain measurements: an experimental investigation utilizing the slit catheter. Surgical management of exertional compartment syndrome of the lower leg: long run observe up. Long-term end result of fasciotomy with partial fasciectomy for chronic exertional compartment syndrome of the decrease leg. Chronic exertional compartment syndrome of the leg: outcomes of treatment by fasciotomy. Microcapillary infusion approach for measurement of intramuscular strain during exercise. Near infrared spectroscopy within the diagnosis of persistent exertional compartment syndrome. Chapter fifty five Common Peroneal and Lateral Femoral Cutaneous Nerve Injuries Ivica Ducic and Jeffrey M. Unlike other surgical disciplines, a big proportion of peripheral nerve surgical procedure makes an attempt to correct neuropathy within the postoperative patient and, therefore, is reoperative in nature. The nerve can turn out to be entrapped in postoperative scar tissue, stretched with knee or ankle dislocations, or inadvertently immediately damaged, resulting in neuropathy. General Nerve Anatomy the peripheral nerve has a big intrinsic blood provide that allows the surgeon to carry the nerve from its anatomic mattress, open the epineurium, and function between the fascicles. In addition, an intensive variety of longitudinal vessels in the epineurium, perineurium, and endoneurium provide the nerve. Scar formation from any surgery or trauma can engulf a peripheral nerve and compress it; symptomatic relief can then be achieved through surgical decompression of the peripheral nerve. Peripheral nerve damage becomes symptomatic both when a critical operate is misplaced or when paresthesia and ache substitute normal sensory signaling. Similarly, compression on a peripheral nerve causes ischemia and neuroma formation. Note the proximity of the nerve to the fibula because it wraps anteriorly on the lower leg. Extreme warning should be exercised in repeat neurolysis of a peripheral nerve, due to repeated nerve devascularization. Those processes amenable to surgical intervention embrace nerve harm because of physical compression associated to varied metabolic situations and surgeries round or adjacent to a nerve. History and physical examination, notably a radical neurologic examination, often counsel the diagnosis by demonstrating a dermatomal distribution of pain or paresthesia. Further imaging and electrodiagnostic testing could also be necessary, mainly to evaluate different causes for the signs. Diagnostic workup must evaluate and exclude other etiologies for postoperative ache, notably infection, loosened hardware, mechanical misalignment, spinal involvement, and neoplasm. The timing of the sensory or motor signs needs to be considered when taking the history and performing the bodily examination, because that can help in understanding the cause of neuropathy. Therefore, the examining physician should be aware of the different potential causes of ache in this anatomic area and should have the flexibility to distinguish deep and superficial paresthesias and pains within the knee space. The most commonly affected sensory nerves concerned in deep knee ache are the lateral retinacular nerve, the medial retinacular nerves, and the articular branch of the widespread peroneal nerve, whereas superficial knee pain is brought on primarily by involvement of the infrapatellar department of the saphenous nerve and the medial and anterior cutaneous nerves of the thigh. Electrodiagnostic research also can have a false-negative fee as excessive as 33%, whereas nerve blocks, because of anatomic variations, may give a false-negative outcome. At that time, additional evaluation by a peripheral nerve surgeon or electrodiagnostic workup is suitable to determine whether or not surgical intervention or continued observation is indicated.
Generic moduretic 50 mg otcThe posterolateral strategy is indicated for fractures of the lateral posterior plateau blood pressure before heart attack order 50mg moduretic mastercard. The incision is prolonged down through the iliotibial band proximally and the fascia of the anterior compartment distally. To expose the lateral tibial plateau, the lateral meniscus is raised with holding sutures after incision of the coronary ligament. The dimension of the fragment is crucial for the decision of whether gentle tissue is stripped off. For small fragments not permitting compression, stripping the displaced fragment for buttress plating is indicated. At the end of surgical procedure the fibular head is refixated by pressure band wiring or screw fixation. Elevation is achieved by fastidiously exerting punches on the pestle (eg, with a hammer) beneath fluoroscopy until the contour of the articular surface is re-established. In instances of severe bone loss, the defect must be full of bone graft or bone substitute. Peripheral longitudinal lesions of the anterior and intermediate part of the meniscus are fixated utilizing the "outside-in suture" technique. Peripheral longitudinal lesions of the posterior meniscus are fixated utilizing the "all-inside" approach to keep away from damage to the neurovascular constructions within the popliteal area. If the lateral metaphyseal shell is intact, a lag screw with a washer or a three-hole typical plate within the antiglide position is normally sufficient. Multifragmentary fractures or fractures with extreme bone loss normally require plate osteosynthesis. Preformed locking or nonlocking plates enable a precise alignment and retention of the fracture. A minimally invasive approach by sliding the plate with the aiming gadget underneath the muscle may be selected. Locking Plates In multifragmentary fractures or fractures with extreme bone loss, an evidence-based advantage of locking plates versus nonlocking plates has not been reported in the literature. However, locking plates in these kind of plateau fractures are advisable for the following reasons: Angular stable plates require much less bone graft compared to conventional plates in fractures with severe bone loss. In circumstances of extreme bone loss, bone graft or bone graft substitute may be wanted for stabilization. Three place screws are placed subchondrally to assist the impacted joint surface (rafting) and a locking plate or buttress plate is applied. Medium-term results of percutaneous, arthroscopically-assisted osteosynthesis of fractures of the tibial plateau. Even a failed meniscal repair that requires subsequent meniscotomy can be briefly protecting to the underlying cartilage. To stop secondary articular melancholy, enough bone graft or bone graft substitute should be used to stabilize tibial plateau despair fractures. However, tibial plateau depression fractures with a poor radiographic reconstruction should be associated with an excellent functional outcome if meniscal integrity is preserved. Therefore, minimally invasive strategies with the least possible gentle tissue stripping and soft tissue irritation must be used. Bone grafting Iliac crest bone grafting is the remedy of choice to preserve the discount of depressed tibial plateau fragments. Bone substitutes corresponding to coralline hydroxyapatite and calcium-phosphate cements have additionally been successfully used. Soft tissue evaluation is a straightforward however pivotal step within the administration of tibial plateau fractures. An excellent discount and fixation could also be compromised by infection secondary to inadequate evaluation of the encompassing soft tissue standing. Fractures with severe soft tissue impairment profit from exterior stabilization and secondary open reduction and inside fixation. Toe-touch weight bearing is really helpful for 4 to eight weeks, with progression thereafter according to radiographic findings. Impression fractures of the lateral plateau managed with a minimally invasive angular plate are allowed weight bearing about 12 weeks after surgery. Early mobilization and range-of-motion exercises are key to the profitable therapy of proximal tibia fractures to keep away from later knee stiffness and muscle wasting. A favorable consequence has been reported for surgically handled low-energy tibial plateau fractures. Spiral computed tomography with two- and three-dimensional reconstruction within the management of tibial plateau fractures. Closed reduction/percutaneous fixation of tibial plateau fractures: arthroscopic versus fluoroscopic control of discount. Compartment monitoring in tibial fractures: the stress threshold for decompression. Tibial condylar fractures: impairment of knee joint stability as a sign for surgical treatment. Total knee arthroplasty after open discount and inside fixation of fractures of the tibial plateau: a minimum five-year follow-up examine. Other indications include the stabilization of closed fractures with high-grade soft tissue harm or compartment syndrome. For patients with multiple long bone fractures, exterior fixation has been used as a technique for short-term, if not definitive, stabilization. With the introduction of circular and hybrid techniques, indications have been expanded to embrace the definitive treatment of advanced periarticular injuries, which include high-energy tibial plateau and distal tibial pilon fractures. Contemporary exterior fixation techniques in current clinical use can be categorized in accordance with the sort of bone anchorage used. This is achieved both using giant threaded pins, that are screwed into the bone, or by drilling small-diameter transfixion wires through the bone. The pins or wires are then related to each other via the use of longitudinal bars or circular rings. The distinction is thus between monolateral exterior fixation (longitudinal connecting bars) and round external fixation (wires connecting to rings). Acute trauma functions primarily use monolateral frame configurations and are the major target of strategies described right here. These "simple monolateral" frames permit for a variety of flexibility with "build-up" or "build-down" capabilities. The second type of monolateral frame is a extra constrained type of fixator that comes preassembled with a multipin clamp at every finish of an extended rigid tubular body. For diaphyseal accidents, the most common sort of fixator utility is the monolateral kind of frame utilizing large pins.
Best buy for modureticMinor levels of fascial dehiscence could go unnoticed and current later as incisional hernias arteria aorta buy generic moduretic pills. Incisional Hernia this type of ventral hernia occurs when part or the entire musculoaponeurotic layer of a laparotomy incision fails to heal correctly. Most hernias are minimally symptomatic, some produce intermittent episodes of ache or obstruction, and others present with acute incarceration. Hernias with bigger fascial defects are generally at a lower threat of incarceration and strangulation. Evisceration Evisceration is a rare however a dreaded complication of contemporary belly incisions. It may be related to poor closure strategies or supplies, or to underlying illness processes similar to persevering with sepsis, malnutrition, immunosuppression or obesity. Note the oedematous and inflamed bowel secondary to a lack of protective coverage. Classification and General Characteristics 541 (a) (b) (c) (d) equipment over the bulge. In the early phases, a spigelian hernia stays contained beneath the external oblique aponeurosis (as an interparietal hernia) and should thus not be Obturator Hernia this unusual hernia occurs via the obturator canal, under the superior pubic rami along the obturator vessels and nerve. These hernias incessantly current as intestinal obstruction and may be troublesome to diagnose. Note the slender fascial defect (marked with arrows) around the urinary conduit (C) and an incarcerated obstructed small bowel loop. Occasionally, the affected person complains of pain referred to the knee along the genicular department of the obturator nerve. A larger hernia could additionally be palpated within the upper medial thigh whereas the hip is flexed, abducted and externally rotated or throughout vaginal examination. With groin hernias, recurrence might outcome not only from an inadequate method, but in addition from a failure to recognize a second coexisting kind of groin hernia through the initial operation. Inferior lumbar hernias arise on the posterolateral abdominal wall through a possible site of weakness within the triangle of Petit, formed by the iliac crest inferiorly, the latissimus dorsi muscle medially and the posterior edge of the external indirect muscle. The superior lumbar hernia originates by way of the triangle of Grynfeltt, which is bounded by the twelfth rib superiorly, the posterior border of the inner oblique muscle inferiorly and the erector spinae and quadratus lumborum muscles medially. Since the predominantly Interparietal Hernia Most hernias herniate by way of the musculoaponeurotic layers of the abdominal wall to current directly underneath the skin. This deep location might create difficulties with bodily prognosis, and imaging could also be needed. Abdominal hernias should be a half of the differential analysis in any affected person presenting with belly ache, bowel obstruction or mass. Groin hernias are best examined with the affected person in an upright position and should be characterized as inguinal or femoral. While minimally symptomatic inguinal hernias may be observed, femoral hernias are more likely to cause incarceration or strangulation and must be repaired. Assess incarcerated hernias (both acute and chronic) for the presence of strangulation. The differential diagnosis of groin pain is extensive and consists of hernias, genital pathology, musculoaponeurotic pain, abnormalities of the lymph nodes and femoral vessels, and referred ache. The pathophysiological mechanism answerable for the most severe complication of incarcerated hernias is: a Gastrointestinal bleeding b Ischaemia c Intestinal obstruction d Pain e Urinary problem Answer b Ischaemia. In any affected person presenting with acute hernia, incarceration, compromise of perfusion (strangulation) and viability of the hernia contents should be the principal concern. Various visceral organs, including the intestines, omentum and ovaries, could be incarcerated in a hernia. Strangulation of the bowel ends in ischaemia of its wall that may end in perforation and sepsis. Intestinal obstruction, on the other hand, could initially occur with or with out strangulation and compromise of blood move. Pain can accompany even a non-strangulated hernia and by itself is a symptom and never a pathophysiological mechanism. Incarceration of the omentum may cause important pain however is in any other case not associated with serious adverse sequelae. In any affected person presenting with an acutely incarcerated groin hernia (inguinal or femoral), an attempt at mild discount ought to be made. If the hernia is irreducible and contains bowel or ovary, pressing surgical intervention have to be instigated. Patients presenting with symptomatic hernias ought to be questioned in regards to the period and nature of their symptoms, wanting particularly for proof of intestinal obstruction. The dimension of the hernia contents is by itself not the criterion for urgency of intervention. Incisional hernias, especially these with a big hernial defect within the absence of obstructive symptoms and with a benign abdominal examination (no concern for strangulation), may be observed. Asymptomatic and minimally symptomatic inguinal hernias in adults, even if bilateral, may be noticed. Inguinal hernias in youngsters ought to all the time be repaired, however this can be done electively if the hernia is reducible. Acquired umbilical hernias develop in adults due to progressive stretching of the umbilical scar (typically in its weaker upper portion) because of chronically elevated intra-abdominal pressure. Symptomatic hernias ought to be thought of for restore to enhance the quality of life and keep away from problems. Congenital umbilical hernias result from a failure of the umbilical ring to heal and are fully lined by umbilical pores and skin. They not often incarcerate, resolve spontaneously in most sufferers and wish restore in solely a minority of patients. The examination of a painful groin mass of pain should embrace which of the following Examination of the groins ought to be carried out with the patient in the upright and supine positions. The abdomen, groins and higher thighs should be examined utilizing visual inspection and palpation. The location of the hernia, mass or area of tenderness must be noted in relation to the anatomical landmarks (specifically the umbilicus, pubic tubercle and inguinal ligament). Examine the testicles and spermatic cords in males and the labia majora in females. A differentiation should be made between a hernia, lymphadenopathy and a scrotal mass. The presence of inguinal lymphadenopathy mandates an examination of the extremities, lower torso, external genitalia and anorectal region. Avoid repeated and aggressive makes an attempt to cut back an incarcerated groin hernia; immediate surgical consultation must be obtained. No try ought to be made to cut back a hernia with overlying inflammatory changes that suggest an underlying strangulated hernia. Obturator hernias may be difficult to diagnose until they prolong onto the thigh or can be palpated through the vagina.
References - Blount WP. Don't throw away the cane. J Bone Joint Surg 1956; 38(A):695-8.
- Bedros AA, Mann JP. Lymphadenopathy in children. Adv Pediatr. 1981;28:341-76.
- Kitchener HC. Survival from cancer of the ovary in England and Wales up to 2001.
- Landon MB, Lynch CD. Optimal timing and mode of delivery aft er cesarean with previous classical incision or myomectomy: a review of the data. Semin Perinatol. 2011;35(5):257-61.
- Alexander JH, Granger CB, Sadowski Z, et al, for the GUSTO-I and GUSTO-IIb investigators: Prophylactic lidocaine use in acute myocardial infarction: incidence and outcome from two international trials. Am Heart J 1999;137:799-805.
- Abrahams DG, Wood P. Pulmonary stenosis with normal aortic root. Br Heart J. 1951;13:519-48.
- Wheeler AP, Rice TW. Coagulopathy in critically ill patients. Part 2-soluble clotting factors and hemostatic testing. Chest. 2010;137(1):185-194.
- Shorter, B., Lesser, M., Moldwin, R.M., Kushner, L. Effect of comestibles on symptoms of interstitial cystitis. J Urol 2007;178:145-152.
|

