|
James L. Thomas, DPM, FACFAS - Associate Professor of Orthopaedic Surgery,
- Department of Orthopaedic Surgery,
- West Virginia University School of Medicine,
- Morgantown, WV
Sildalis dosages: 120 mg
Sildalis packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

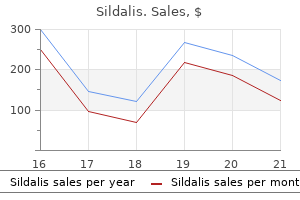
Buy cheap sildalis 120 mg lineOnce the bladder is completely mobilized off the uterus and the fistulous tract has been excised erectile dysfunction treatment massachusetts order sildalis 120 mg with visa, the bladder is closed in two layers of interrupted or continuous No. This is followed by an interrupted or continuous closure of the defect in the uterus. Laparoscopic and Robotic Repair of Vesicovaginal Fistula Laparoscopic or robotic routes can be utilized by an skilled laparoscopic/robotic surgeon for the repair of urinary tract fistulas that require an abdominal strategy. Since the primary case report of laparoscopic restore described by Nezhat and colleagues in 1994 and robotic restore described by Melamud and colleagues in 2005, there have been many printed small case collection of laparoscopic and robotic experiences with 86% to one hundred pc success rates, 8% to 12% laparotomy conversion rates, and operative occasions of 70 to 280 min. A, Vesicouterine fistula involving the decrease uterine segment and upper cervix and the again of the bladder. B, A high cystotomy has been made and sharp dissection is used to separate the bladder from the uterus. D, Bladder and uterus are every closed in two layers; omental flap is interposed between the 2 constructions (inset). If the fistula includes the cervix and bladder and could be identified and accessed by way of the vagina, the fistula could be closed vaginally by dissecting the cervix and decrease uterine segment off the bladder and identifying the fistula tract. The bladder can then be closed in layers as described earlier, followed by reapproximation of the uterus/cervix. Urinary conduits can be constructed from small or massive bowel; they might be continent or incontinent. The Kock pouch makes use of ileum with intussusception strategies, and the Miami pouch makes use of proper hemicolon and a tapered terminal ileum. Complications include stone formation, conduit leak and reflux, and metabolic disturbances. Early and late issues in continent diversions happen in 13% to 15%; reoperation is critical in 1% to 4%. Most experts and evaluate articles advocate 10 to 21 days of steady drainage through a transurethral or suprapubic catheter. Longer duration of bladder catheterization could increase the risk for urinary tract infections and other associated morbidities. This may be an much more important problem in resource-limited nations as fistula patients usually stay within the hospital until catheter removal. Longer stays within the hospital by current patients will lower hospital turnover and thereby stop extra patients from present process repair in a timely fashion.
[newline]There are retrospective research and one randomized managed trial that demonstrated no variations in repair success and postoperative infection in 189 obstetric fistula sufferers randomized to 10 days of continuous bladder drainage compared with 14 days of steady bladder drainage (Nardos et al. Risk components associated with incontinence embrace urethral involvement, small contracted bladder or a big fistula, elevated vaginal scarring or fibrosis, or recurrent fistulas (Browning, 2006; Sj�veian et al. In a couple of small case sequence of urodynamic findings on obstetric fistula patients who current with urinary incontinence after successful fistula repair, 31% to 56% had stress incontinence, 37% to 41% had blended incontinence, and 4 to 13% had voiding dysfunction, with a mean bladder capacity of 200 mL found in one study (Carey et al. Techniques such as periurethral injection of bulk-enhancing agents have been reported for women with stress incontinence signs after successful restore of a fistula. Autologous rectus or fascia lata slings and synthetic slings have been used with comparable rates of stress incontinence decision or improvement (64%-90%) however with considerably greater rates of erosion (20%) in the synthetic sling group (Ascher-Walsh, 2010; Murray et al. Another autologous sling that has been reported in the literature is the pubococcygeus sling, created by identifying the pubococcygeus muscle and surrounding connective tissue bilaterally (Browning, 2004, 2006). The muscle is detached posteriorly while leaving the anterior attachment intact on either side. Sufficient muscle should be indifferent posteriorly to permit for tension-free approximation beneath the urethra. The freed posterior ends of the muscle are then sutured in the midline beneath the urethra. In two small case sequence (12 girls and 32 women) with short-term follow-up periods (2-3 weeks), 67% to 69% of ladies have been continent, with 13% to 16% experiencing urinary retention. Complications the surgical restore of genitourinary fistulas may be difficult by dangers common to all operations, such as hemorrhage, an infection, and thromboembolism. If tissue breakdown happens at the vaginal or bladder suture lines, the fistula may persist or recur. Other delayed surgical issues include vaginal stenosis and small-bladder syndrome, osteitis pubis, and urinary incontinence (see below). Dyspareunia attributable to tenderness over the location of Martius grafts has been reported. Metabolic disturbances and recurrent pyelonephritis might develop after ureterosigmoidostomy. After profitable fistula restore of genitourinary fistula, elective cesarean supply is strongly beneficial for all subsequent births. Although most collection report a excessive remedy rate of obstetric fistula closure, persistent urinary incontinence stays a major clinical issue in these patients and has been reported in 10% to 55% of ladies after profitable fistula closure. The identical ischemic damage that led to the event of the fistula can also compromise continence mechanisms with both direct urethra/urethral sphincter harm or local soft tissue destruction and nerve damage resulting Prevention In the developed world, most urinary tract fistulas occur from complications incurred during surgery. Most commonly, the bladder is topic to trauma or damage throughout dissection from the cervix and higher vagina on the time of hysterectomy. This is evidenced by findings in one large sequence of no vesicovaginal fistulas in one thousand supracervical hysterectomies (Harki-Siren et al. Fistulas that occur because of hysterectomy are usually found in the posterior wall of the bladder superior to the interureteric ridge. Tancer (1992), in a retrospective evaluate of 151 urogenital fistulas, presented ideas and observations on avoiding harm to the bladder during whole abdominal hysterectomy. They included the usage of a two-way indwelling catheter; sharp dissection of the bladder off the uterus, cervix, and higher vagina; careful placement of sutures and clamps throughout vaginal cuff closure; extraperitoneal cystotomy when the dissection is difficult; retrograde filling of the bladder when harm is suspected; and restore of an overt bladder damage only after mobilization of the injured area. Another method of stopping bladder injury is by performing an intrafascial hysterectomy. The vesicocervical space must be fully developed, and the bladder have to be thoroughly mobilized inferiorly and laterally. In theory, the bladder has been mobilized from the location of entry into the vagina and is much less prone to be compromised because it rests on the dissected fascia. In a latest evaluate of 867 girls who underwent an intrafascial belly hysterectomy, a bladder injury incidence of zero. It is paramount to acknowledge and repair bladder and ureteral harm intraoperatively to prevent fistula improvement. In an older meta-analysis, solely 52% of bladder accidents and 12% of ureteral injuries had been detected intraoperatively with an increase in detection rate to 85% and 90% respectively if routine cystoscopy is performed intraoperatively, (Gilmour, 1999). Studies by Pettit and Petrou (1994) and Wiskind and Thompson (1995) have shown a significant prevalence of unsuspected ureteral injuries (0. When a cystotomy occurs, the first precedence is to decide the proximity of the cystotomy to the ureteral orifices and decide if the ureter is also compromised. This is finest done by way of cystoscopy, by extending the cystotomy or by making a separate extraperitoneal cystotomy during an stomach case. The authors prefer to tag the opposing poles of the cystotomy with delayed absorbable sutures, and normally a No. We prefer to embody the mucosa in the closure of excessive, nondependent cystotomies, nonetheless, we attempt to place sutures extramucosally in lower, dependent cystotomies. A second layer is normally included to imbricate the bladder muscularis over the primary layer.
Discount sildalis online master cardA variety of these patients had been significantly improved what causes erectile dysfunction yahoo buy sildalis with a visa, and whereas injection remedy could only last 12 months, repeat injections were generally reproducible. A comparability of periurethral and transurethral methods of injection discovered comparable outcomes however a higher (although not statistically significant) fee of early complications in the periurethral group. Cure or improvement happens in 70% to 80% of sufferers, with complete continence in round 40%. Complications and Safety the most typical adverse events with urethral bulking are gentle pain, urinary retention, dysuria, hematuria, urinary tract infection, and erosion. If bleeding happens, it often responds to direct pressure; however, hematoma formation has been reported in this inhabitants. This can be avoided or decreased by submucosal placement of the needle approximately 1 cm into the tissue and by holding the needle in place for a number of seconds (up to 30 s) to allow the strain to dissipate. Most materials are injected through a 20-gauge needle or smaller; thus, the extent of extrusion of material is seldom an issue. After the injection, the most typical adverse occasions within the quick period are urinary retention and voiding dysfunction. It is necessary to assess voiding after the injection is full, and this can be accomplished by comparing the quantity voided with the amount of fluid infused in the course of the process, using a bladder scanner, or by performing a straight catheterization. Urinary tract infection happens in 10% to 25% of circumstances; thus, antibiotic therapy must be thought of after the injection and/or the urine ought to be checked for infection on the initial postoperative visit. Pain with urination happens in some sufferers however is self-limited, as previously discussed. Macroplastique was related to a high incidence of dysuria lasting up to 48 h. An abscess may be related to growing voiding dysfunction with or without pain. Another long-term problem is recurrent urinary tract infections requiring prolonged prophylactic antibiotics. Inherent within the discussion of indications, contraindications, and complications is the theme that the at present obtainable products used for urethral bulking are protected. The commonest event is urinary tract infection, which regularly occurs distant from the injection process. Other Durasphere the effectiveness of Durasphere was reported at 1, 2, and three years in a randomized examine in which it was compared with Contigen (Chrouser et al. The Durasphere group had 63%, 33%, and 21% cure or improvement at 1, 2, and three years, respectively, in contrast with the Contigen group, which had 63%, 19%, and 9% cure or enchancment, respectively. Defined as 1 improvement on Stamey Continence Grading, which is a 4-level scale of incontinence severity starting from 0 = continent-dry to 3 = total incontinence regardless of activity. Macroplastique A systematic review of Macroplastique by Ghoneim and Miller in 2012 demonstrated improvement rates of 73% at 6 to 18 months and 64% at longer than 18 months. The perfect bulking material has not been discovered, and despite a chronic search, nothing financially feasible as yet seems to be better than the obtainable bulking brokers. However, grownup stem cell injection remedy utilizing autologous muscle-derived stem cells for the regenerative repair of an impaired sphincter is at present on the forefront of incontinence analysis. The implanted cells fuse with muscle and release trophic components selling nerve and muscle integration. At 12 months, 63% of Coaptite sufferers compared with 57% of collagen sufferers showed improvement in urinary incontinence symptoms. Fewer patients within the Coaptite group required reinjection (62% versus 74%, p = zero. Treatment of intrinsic sphincter deficiency utilizing autologous ear chondrocytes as a bulking agent. Carbon coated zirconium beads in betaglucan gel and bovine glutaraldehyde cross-linked collagen injections for intrinsic sphincter deficiency: continence and satisfaction after prolonged followup. The tension-free vaginal tape in girls with a non-hypermobile urethra and low maximum urethral closure stress. Multicenter randomized clinical trial evaluating surgery and collagen injections for therapy of female stress urinary incontinence. Repeat midurethral sling in contrast with urethral bulking for recurrent stress urinary incontinence. Cross-linked polydimethylsiloxane injection for feminine stress urinary incontinence: outcomes of a multicenter, randomized, controlled, single-blind research. Durability of urethral bulking agent injection for feminine stress urinary incontinence: 2-year multicenter research results. A systematic review and meta-analysis of Macroplastique for treating feminine stress urinary incontinence. Three-dimensional endovaginal ultrasound examination following injection of Macroplastique for stress urinary incontinence: outcomes based on location and periurethral distribution of the bulking agent. Urethral Bulking Before, After, and Compared with Surgery for Stress Urinary Incontinence Urethral bulking has been studied in varied specific affected person populations, to embody use earlier than and after sling procedures in addition to comparability trials. A multicenter randomized trial evaluating collagen injection with surgery (6 needle suspensions, 19 Burch procedures, and 29 pubovaginal slings) demonstrated greater efficacy within the surgery group (72%) versus the collagen group (51%), though a better complication rate was demonstrated within the surgical procedure group (Corcos et al. Thirty pubovaginal slings and 13 synthetic mid-urethral slings had been positioned with an 18. Conversely, urethral bulking with collagen has been studied after prior urethral surgery (mostly bladder neck suspension) for stress incontinence, with 93% reporting treatment or enchancment. Collagen injection for feminine urinary incontinence after urethral or periurethral surgical procedure. Human amniotic fluid stem cell injection remedy for urethral sphincter regeneration in an animal model. Safety and efficacy of sling for persistent stress urinary incontinence after bulking injection. A new injectable bulking agent for treatment of stress urinary incontinence: results of a multicenter, randomized, managed, double-blind study of Durasphere. Randomized controlled multisite trial of injected bulking agents for women with intrinsic sphincter deficiency: midurethral injection of Zuidex via the Implacer versus proximal urethral injection of Contigen cystoscopically. Multicenter potential randomized 52-week trial of calcium hydroxylapatite versus bovine dermal collagen for treatment of stress urinary incontinence. Particle migration after transurethral injection of carbon coated beads for stress urinary incontinence. Bulking agents for stress urinary incontinence: short-term outcomes and complications in a randomized comparability of periurethral and transurethral injections. Periurethral collagen injection for stress incontinence with and without urethral hypermobility. Complications of sterile abscess formation and pulmonary embolism following periurethral bulking agents.
Purchase sildalis with american expressOur practice continues to supply this process within the outpatient setting for patients with mild to moderate fecal incontinence erectile dysfunction drugs singapore purchase cheap sildalis online. Additionally, we do supply this therapy to patients with inner sphincter thinning or fibrosis as seen on anal endosonography. The anal area is evaluated to rule out giant hemorrhoids using a protracted beveled anoscope. The needle is launched underneath imaginative and prescient, 5 mm above the dentate line at a 30� angle to the mucosa to a depth of 5 mm. Surgical Treatment For sphincter repairs, the bowel is totally cleansed with an agent, such as polyethylene glycol. Prophylactic antibiotics, similar to intravenous metronidazole and a third-generation cephalosporin, are given preoperatively. These antibiotics are continued postoperatively for variable durations, at the discretion of the surgeon. For surgery to appropriate a defect secondary to an injury, the tissue should be soft and pliable, and no less than 3 to 6 months should elapse after the injury for the inflammation to subside. Patients could additionally be positioned within the lithotomy position or susceptible jackknife place for procedures directly performed on the sphincter muscle. For muscle wraps or the bogus sphincter, the prone jackknife position is indicated. We prefer the prone jackknife position for nearly all anal procedures as a outcome of it permits the buttock muscle tissue to fall out of the greatest way and provides the surgical assistants optimum viewing of the surgical area. For easy procedures, similar to sphincteroplasty or postanal repair, common, epidural, or spinal anesthesia may be used. It is necessary to keep in mind that the branches of the pudendal nerves that innervate the external sphincter strategy the muscle from the posterolateral place. We prefer to initially dissect down the rectovaginal septum to keep away from harm to any remaining muscle and to keep away from buttonhole defects into the anal canal or rectum. Sometimes the only remaining perineal body is the vaginal and anal mucosa, so dissection is difficult. Placing a finger in the vagina or rectum and dissecting from lateral to medial may facilitate the dissection. The ends of the sphincter are often approximated with scar within the midline (or midportion of the injury). This scar is divided within the middle, leaving two ends of sphincter with scar hooked up. If each the interior and exterior muscles are injured, we prefer to go away them intact and repair them as one unit. The sphincter ends which were sufficiently mobilized to allow overlapping of the muscle are grasped. Some Sphincteroplasty When a defect is detected in the sphincter advanced, reapproximation of the 2 ends is tried. Usually, these defects are secondary to obstetric harm, fistula restore, or lateral inner sphincterotomy. A curved incision is made anteriorly, avoiding the pudendal nerves, which approach the external sphincter from a deep posterolateral position. During the process, irrigation of the wound is carried out with antibiotic answer. If a major amount of "useless house" is current, a half-inch Penrose drain may be inserted after which removed on postoperative day 2. This addition was made after we found dismal long-term results after the overlapping sphincter restore. Short-term results indicate no improve in wound an infection, but long-term results on the efficacy and value justification are to be evaluated. Postoperatively, sufferers are kept on intravenous antibiotics for two to three days, and oral consumption is withheld. The Foley catheter is eliminated on postoperative day 2, and the affected person is allowed a highfiber food regimen simply earlier than discharge. Because they bear a whole bowel cleansing earlier than surgery, patients may not move their bowels for several days after surgical procedure. B, Three mattress sutures are positioned on both sides to maintain the muscle ends in place. This process is designed to reestablish the anorectal angle, increase the size of the anal canal, and tighten the anal canal. Optimal outcomes appear to be in sufferers with incontinence from anal sphincter stretch or lack of anorectal angulation. Sutures are placed and tied to again type a lattice, particularly posteriorly, although anteriorly the ends may also be approximated. Original outcomes by Parks (1975) demonstrated postoperative improvement in incontinence in 80% of sufferers; nonetheless, this degree of success has not been achieved by others. Further research have proven that long-term continence is restored in perhaps 30% of sufferers who bear the postanal repair. Complete disruption of the skin sutures usually heals by secondary intention with enough wound care. In sufferers undergoing repeat overlapping sphincter repair, the development price is just like those who have initially had the defect corrected. Even when patients have glorious preliminary enchancment in fecal incontinence after sphincter repair, a number of studies have discovered that long-term results are disappointing. Collectively, these research have proven that less than 40% of sufferers who endure a repair report long-term satisfactory fecal continence 5 to 10 years after surgical procedure. Additionally, some sufferers have had traumatic lack of sphincter muscle, making approximation of the ends unimaginable. To perform dynamic graciloplasty, the gracilis muscle is mobilized from the inner thigh, proximally preserving the neurovascular bundle. The tendon of insertion is divided on the knee, preserving as much tendon as possible. The muscle is wrapped around the anus, and the tendon is sewn to the opposite ischial tuberosity. Leads are tunneled from the stimulator and positioned onto the proximal portion of the nerve. The entire process is completed under cover of a stoma and normally in several stages. Patients applicable for this process embody those with incontinence caused by obstetric damage, idiopathic incontinence, traumatic loss of sphincter muscle, and congenital anal sphincter issues. In their 1995 research, about 23% achieved excellent continence for solid and liquid stool and flatus. As extra expertise is gained with this procedure, surgeons hope that the technical and studying problems might be remedied. Artificial Anal Sphincter As success with the artificial urinary sphincter was attained, efforts turned towards utilizing a modified model of this gadget for fecal incontinence. This absolutely implantable gadget incorporates a balloon that, when fully inflated, occludes the anus.

Purchase sildalis lineUsually a mix of behavioral smoking and erectile dysfunction causes discount sildalis 120 mg, cognitive, and pharmacological therapies can used to achieve this. Fluoroscopic picture taken during voiding shows a spinning prime urethra with obstruction on the degree of the external sphincter. There is an elevated incidence of dysfunctional voiding in sexual abuse victims, and it has been linked to psychological stressors and elevated Hamilton scores measuring stress and anxiety; therefore, certain individuals might profit from mental well being remedy and help as properly. Some pharmacotheraputic choices have been shown to be useful in patients with dysfunctional voiding. Several clinicians, together with ourselves, have had anecdotal success with amitriptyline. Vaginal benzodiazepine suppositories also have been used as an adjunct remedy in high-tone pelvic floor dysfunction related to dyspareunia. Finally, the function of neuromodulation in nonobstructive urinary retention has been shown to be helpful. There was a lower within the number of catheterizations by 50% and a decrease in catheterized volume from 379 to 109 mL. There was proof of scientific success in 58% and 71% of patients respectively at five years after implantation. Many of these women have a history or findings consistent with polycystic ovary, which means that the abnormal sphincter may be underneath the influence of estrogen and might be due to a hormone-sensitive channelopathy confined to the urethral sphincter; however, the precise pathophysiology of the disease remains to be unknown. Many of these girls usually have a trigger such as basic anesthesia, urinary tract infection, gynecologic surgical procedure, or childbirth. Oral agents and sphincteric Botox injections have been tried with equivocal results and no actual proof to help their use. The total success fee was 68% with 12 patients undergoing everlasting implantation; 10 patients were in a position to void usually and two sufferers still wanted to catheterize. It is usually well tolerated and safe and offers a helpful therapeutic option to restore voiding in these sufferers. There is a sustained detrusor contraction of >50 cm H2O with failure of the bladder neck to open. Marion (1933) initially described it in a male patient, however its presence in girls was discovered by Diokno et al. Another is that a continual high tonus within the clean muscle of the posterior urethra causes rigidity of the bladder neck. A principle that an elevated variety of -adrenergic receptors resulting in nonrelaxation during voiding additionally has been suggested. They confirmed that sufferers with dysfunctional voiding have larger imply most flow price (12 versus 7 mL/s, P = zero. The number of those who elect statement and have progressive signs, decompensation, and even go on to receive remedy is unknown. This could be done both unilaterally or bilaterally, but the primary concern of bladder neck incision is the development of postoperative stress incontinence. The idea of bladder neck incision initially was described by Turner-Warwick et al. A 76% success fee at mean follow-up of fifty five months was obtained; one affected person (3%) developed incontinence. Twenty-five sufferers have been available for follow-up at five years, and there was important improvement in both subjective and goal voiding functions. Voiding dysfunction attributable to pelvic prolapse can be treated by a pessary or surgical repair. Iatrogenic Postsurgical Obstruction Surgical procedures for the correction of stress incontinence are designed to restore help to the urethrovesical junction or to enhance coaptation of the urethra (in cases of intrinsic sphincter deficiency). This could be completed in varied ways, including retropubic colposuspension, and pubovaginal and midurethral sling procedures. A potential complication of all these procedures is iatrogenic outlet obstruction resulting in voiding dysfunction. The incidence of iatrogenic urethral obstruction varies widely within the literature, from 2. The wide discrepancy in reported charges could also be explained by various factors, corresponding to variations in definition, varying patient inhabitants, and surgical differences. Obstruction after incontinence surgery is often a results of technical elements, such as improper placement or excessive tensioning of sutures or slings. Even tension-free procedures just like the retropubic or transobturator midurethral slings have an estimated incidence of iatrogenic obstruction between 0% and 4% as compared with a 6. Obstruction may be brought on indirectly by a cystocele or other prolapse that either was uncorrected at the time of surgery or had occurred postoperatively. Impaired detrusor contractility, a condition that ought to have been current preoperatively, in the face of increased urethral resistance by an anti-incontinence process, may cause obstruction. Finally, the affected person who habitually voids by abdominal straining may have problem emptying after pubovaginal sling surgery because the sling acts to improve urethral resistance with increases in belly strain. Transient voiding dysfunction is frequent and anticipated after many forms of anti-incontinence surgical procedure. Most ladies will begin voiding sufficiently on their own inside a number of days to weeks, whereas others could take longer to resume regular voiding and should must learn to do intermittent catheterization. Storage symptoms of urgency, frequency, and urge incontinence are sometimes more refractory than retention as a result of they are often associated to bladder modifications. Although this timeframe is arbitrary, most information in the literature are based mostly on a ready period of a minimum of three months to guarantee enough time for retention from obstruction to resolve and to decrease the chance of recurrent stress incontinence. After three months, a really low chance is current that any persistent retention will resolve with out intervention. In the case of up to date synthetic midurethral slings, some have advocated quicker intervention, within 7 to 10 days, when complete Pelvic Organ Prolapse Prolapse of pelvic organs can have a profound effect on decrease urinary tract perform. In addition to the frequent symptoms of urinary frequency, urgency, and incontinence, bladder outlet obstruction and ranging levels of urinary retention can happen. Obstruction from prolapse could be brought on by kinking of the urethra in cases of anterior vaginal wall prolapse (cystocele) or by direct compression of the prolapsing organ on the urethra. It can be demonstrated urodynamically by evaluating patients with the prolapse unreduced. The impact of the prolapse on voiding operate can be seen further by lowering the prolapse (with a pessary, vaginal retractor, or vaginal packing) and repeating the study. Using this method, Romanzi and Blaivas (1999) found obstruction in 4% of the grades one and two cystoceles and 58% of the grades three and 4 cystoceles. After retropubic and transobturator midurethral slings, momentary voiding dysfunction resolved in 25% to 66% of patients in a single to two weeks and in 66% to 100 percent of sufferers by six weeks. Because of the immobility of the polypropylene mesh and the ingrowth of fibroblastic tissue at one to two weeks, patients with extreme signs or urinary retention are less likely to enhance after this period and the standard three-month waiting interval appears unwarranted.
Order sildalis 120mg overnight deliverySome surgeons advocate routinely acquiring a cystogram earlier than elimination of the catheter erectile dysfunction due to diabetes icd 9 discount 120 mg sildalis overnight delivery. Careful dosage calculation, administration, source insertion, and shielding, together with acceptable bladder drainage, can cut back the danger of radiation-induced decrease urinary tract fistulas. This complication might nonetheless come up many years after a symptom-free interval and is probably not completely preventable. In the creating world, urinary tract fistulas generally outcome from complications of childbirth. Although maternal mortality from pregnancy-related complications has decreased more than 35% prior to now 30 years, there were nonetheless an estimated 343,000 deaths per yr in 2008 (Hogan, 2010). The World Health Organization estimates that for each mother who dies, 10 to 20 are injured, with 8% struggling obstructed labor and attainable vesicovaginal fistula growth. Epidemiologic analysis is urgently needed to establish communities with a excessive prevalence of fistulas and to determine the characteristics of ladies at excessive risk for bladder or urethral injury throughout childbirth. Preventive strategies should be directed at a quantity of ranges to obtain a significant discount within the incidence of genitourinary fistulas attributable to neglected obstructed labor. Economic positive aspects will lead to improved dietary standing and decreased prevalence of pelvic contracture. Increased availability of prenatal care and institution of maternity waiting houses would improve care during pregnancy and establish situations, similar to irregular fetal presentation, before labor. Trained start attendants could perform bladder drainage in labor and determine abnormal labor patterns, utilizing portographs. Emergency transport for girls in prolonged labor to facilities staffed by skilled personnel might allow abdominal supply when vaginal delivery is unimaginable. Many experts additionally recommend inserting Foley catheters in any women who report a historical past of undergoing labor for >24 h. Until all of these targets, can be realized, genitourinary fistulas will continue to happen and girls will need superior look after surgical management. Further remarks upon a brand new and profitable mode of therapy for vesicovaginal fistula. Vesico-Vaginal Fistula from Parturition and Other Causes with Cases of Recto-Vaginal Fistula. The remedy of an intractable vesicovaginal fistula by the use of pedicled muscle graft. The restore of intensive vesicovaginal fistulas with pedicled omentum: a review of 27 circumstances. Die operative Wiederher-stellung der Volkommen fehlenden Harnrohre und des Schliessmuskels derselben. Paper introduced to the meeting of the Federation of International Gynaecology and Obstetrics World Congress, San Francisco, 1980. Ureterouterine and vesicourethrovaginal fistulae as a complication of cesarean part. Early versus late restore of vesico-vaginal fistulas: vaginal and abdominal approaches. Use of rectus abdominus muscle flap for the treatment of complex and refractory urethrovaginal fistulae. Results of early repair of vesicovaginal fistula with preliminary cortisone remedy. Combined percutaneous antegrade and cystoscopic retrograde strategy in the remedy of distal ureteral fistulae. Risk components for the development of vesicovaginal fistula after incidental cystotomy on the time of a benign hysterectomy. Ten-year experience with transvaginal vesicovaginal fistula repair using tissue interposition. The use of modified Martius graft as an adjunctive technique in vesicovaginal and rectovaginal fistula repair. Transvaginal mobilization and utilization of the anterior bladder wall to repair vesicovaginal fistulas involving the urethra. Recognition and administration of patients with high-risk vesicovaginal fistulas: implications for teaching and analysis. Surgery for the obstetric vesicovaginal fistula: a evaluation of one hundred operations in eighty two patients. Factors influencing urinary fistula repair outcomes in creating international locations: a scientific evaluate. Development and comparison of prognostic scoring techniques for surgical closure of genitourinary fistula. Comparative analysis of outcome between open and robotic surgical restore of recurrent supra-trigonal vesico-vaginal fistula. Successful restore of a big vesicovaginal fistula with associated urethral loss utilizing the anterior bladder flap approach. Vaginal reconstruction utilizing the bladder and/or rectal partitions in patients with radiation-induced fistulae. Postirradiation vesicovaginal fistula utterly resolved with conservative treatment. Full-thickness Martius grafts to preserve vaginal depth as an adjunct in the repair of large obstetric fistulas. Formation of vesicovaginal fistula: the function of suture placement into the bladder during closure of the vaginal cuff after transabdominal hysterectomy. Anatomic and useful results of transperitoneal-transvesical vesicovaginal fistula restore. Successful endoscopic closure of radiation induced vesico-vaginal fistula with fibrin glue and bovine collagen. Antibiotic use in obstetric fistula restore: single blinded randomized medical trial. Urinary and faecal incontinence following delayed main restore of obstetric genital fistula. Cyanoacrylic glue: a minimally invasive nonsurgical first line approach for the treatment of some urinary fistulas. Risk elements that predict failure after vaginal restore of obstetric vesicovaginal fistulae. Outcome of obstetric fistula restore after 10-day versus 14-day Foley catheterization. Social Consequences of Vesico-Vaginal Fistulae: Zaria Experiences, Society of Obstetrics and Gynecology of NigeriaConference, Calabar, September 5�8, 1989. Fibrin glue versus martius flap interpositioning within the repair of difficult obstetric vesicovaginal fistula. A pyelographic study of ureteric injuries sustained throughout hysterectomy for benign circumstances. Clinical analysis of a surgical approach for the correction of full urinary incontinence. Observations on prevention and administration of vesicovaginal fistula after total hysterectomy. A randomised managed trial of antibiotic prophylaxis for vesico-vaginal fistula restore.
Syndromes - Diarrhea or watery stools
- Irreversible damage to the lungs due to untreated high blood pressure in the lungs
- Nause
- Pieces of stone are left in your body. You may need more treatments.
- General anesthesia. This means you will be asleep and unable to feel pain.
- Drooling
- Try to get as much privacy as possible. Some people find that reading while sitting on the toilet helps them relax enough to have a bowel movement.
- If you have bleeding problems
Sildalis 120mg mastercardThe reported incidence of vesicovaginal fistula after hysterectomy is approximately 1 in 1300 surgeries erectile dysfunction guide purchase 120mg sildalis otc. During the study interval, sixty two,379 hysterectomies had been performed and 142 urinary tract accidents wer reported. The incidence of vesicovaginal fistula was 1 in 1200 procedures: 1 in 455 after laparoscopic hysterectomy, 1 in 958 after whole stomach hysterectomy, and 1 in 5636 after vaginal hysterectomy. The threat of ureteral injury was greater with laparoscopic procedures than with open or vaginal procedures. Bladder and urethral injury are also identified problems of anti-incontinence procedures and restore of pelvic organ prolapse. A current improve has occurred in these kind of fistulas, mirroring the increased popularity of quite a few synthetic materials used during such procedures. Thirty-four girls in a 2-year interval required sling removal, and six had developed urethrovaginal fistulas. There are also case reviews of urethrovaginal fistula improvement after urethral diverticulectomy and periurethral injection of a bulking agent. Radiation remedy, used for carcinoma of the cervix or other pelvic malignancies, may not often result in fistula formation. Healthy tissues of the anterior vaginal wall tolerate radiation doses as excessive as 8000 rad. Fistulas could first appear through the course of radiotherapy, usually from necrosis of the tumor itself, or after therapy is completed. In planning a restore of a fistula after radiotherapy, ruling out recurrent malignancy with biopsy of the fistula margins is essential. Most genitourinary fistulas that result from gynecologic surgical procedure occur secondary to urinary tract accidents. This underscores the necessity to strongly consider routine cystoscopy to assess for bladder and ureteral integrity after hysterectomy, prolapse, or incontinence surgical procedures, in addition to another pelvic surgical procedure in which the decrease urinary tract may be in danger. Bladder accidents ensuing from complete stomach hysterectomy happen primarily during blunt dissection of the bladder off the decrease uterine phase. Devascularization or an unrecognized tear in the posterior bladder wall subsequently ends in tissue ischemia, necrosis, and fistula formation. Vesicouterine and vesicocervical fistulas are rare and are usually issues of obstetrical surgery, occurring most incessantly after a cesarean section. Vesicovaginal and urethrovaginal fistulas are greatest classified as being both simple or difficult. Complicated urethrovaginal fistulas are people who involve the proximal urethra and bladder neck and/or are radiation induced. Complicated vesicovaginal fistulas include previous radiation, pelvic malignancy, compromised vaginal length, bigger than 3 cm, and involving the trigone. Presentation and Investigation Patients with genitourinary fistulas current in some ways. Gross hematuria or irregular intraperitoneal fluid accumulation (urinoma) noted during or after surgical procedure ought to raise suspicion of an unrecognized urinary tract injury and dictates quick investigation. In the postoperative period, symptoms could develop after an interval of days, weeks (surgical and obstetric fistulas), months, and even years (radiotherapyrelated fistulas). Most sufferers have steady urinary leakage or persistent watery vaginal discharge, which is leakage of urine from the vagina. If the fistula is very small, leakage could additionally be intermittent, occurring only at maximal bladder capacity or with specific physique positions. Other indicators and symptoms include unexplained fever, hematuria, recurrent cystitis or pyelonephritis, vaginal pain, suprapubic ache, flank pain, and abnormal urinary stream. The preliminary analysis of all sufferers with symptoms of genitourinary fistulas starts with a whole physical examination. A thorough speculum examination of the vagina may reveal the supply of fluid, which can then be collected; measurement of its urea concentration might determine it as urine. Urine ought to be examined microscopically and cultured, and acceptable remedy should be instituted for infection. Further office analysis, cystourethroscopy, and imaging research similar to intravenous urography permit the doctor to localize the fistula and exclude or determine different forms of urinary tract harm. In all circumstances of suspected urinary tract fistula, it is important to evaluate for each bladder and ureteral involvement, as ureteral compromise has been reported in up to 12% of vesicovaginal fistula. Although the sensitivity and specificity of the tampon take a look at are unknown, instillation of methylene blue or indigo carmine into the bladder sometimes stains vaginal swabs or tampons within the presence of a vesicovaginal fistula. Once a vesicovaginal fistula has been excluded, intravenous indigo carmine could be given and the tampon noticed for blue staining to evaluate for a ureterovaginal fistula. Intravenous methylene blue should be used with caution because of the chance of methemoglobinemia, a rare however serious complication. In developed international locations, radiologic research are recommended in most cases and usually embrace intravenous urography, cystoscopic retrograde urography, or voiding cystourethrography. Water or regular saline cystoscopy may be impossible with massive fistulas; in such cases, a Foley catheter could additionally be positioned inside the fistula tract to lower leakage. Conservative Management Various conservative or minimally invasive therapies are available for vesicovaginal and ureterovaginal fistulas, although the true viability and success of these therapy modalities are unknown. The most conservative remedy of a vesicovaginal fistula is solely extended bladder drainage with a Foley catheter. In a retrospective evaluation of 1716 ladies with obstetric vesicovaginal fistula, steady catheter drainage resulted in spontaneous fistula closure in 15% of sufferers. Spontaneous closure occurred in 50% to 60% of patients with fistulas that had been 2 cm and who introduced for care no later than 4 to 6 weeks after supply (Waaldijk, 1994, 2004). Other much less invasive options embrace curetting, electrofulguration, and laser ablation to deepithelialize the fistula tract and allow it to spontaneously heal while the bladder is continuously drained. Once the fistula tract has been deepithelialized, agents such as fibrin glue and collagen have been successfully injected into the fistula tract to promote closure. Most of these studies report profitable therapy in fistulas that are small (5 mm), resulting from gynecologic surgery. There have additionally been reports of utilizing these strategies to successfully close radiation-induced fistula. More lately, brokers similar to cyanoacrylic glue administered percutaneously, endoscopically, or vaginally have been utilized in a collection of 13 urinary tract fistulas of differing etiology with 85% success charges after a mean follow-up period of 35 months (Muto et al. The really helpful preliminary administration of a ureterovaginal fistula is ureteral stenting. Stenting is more profitable when carried out sooner quite than later; in one research, 82% of attempts in patients whose fistulas had been <1 month old were successful, in contrast with 33% of makes an attempt with older fistulas. Stents are normally manufactured from Silastic, with the size measured in centimeters and the diameter measured in French units, with single-J or double-J ends.
Buy sildalis usExtracorporeal knot-tying is carried out after each sew is positioned erectile dysfunction see urologist generic sildalis 120 mg with amex, which is often performed concomitantly with a uterosacral ligament vaginal vault suspension so that apical suspension is reestablished. To date, most laparoscopic colposuspensions have been carried out for under major stress incontinence due to problem in dissecting retropubic adhesions. Many sufferers choose laparoscopic and robotic-assisted surgical procedure because of the smaller, extra cosmetic incisions, shorter recuperation time, and fast return to work. Access Route: Extraperitoneal or Intraperitoneal the utilization of an extraperitoneal or intraperitoneal method depends on whether or not concomitant intraperitoneal procedures are being performed, on whether the affected person has had previous abdominal wall surgical procedure, and on surgeon choice. Previous retropubic surgical procedure is a contraindication for extraperitoneal approach, and low transverse or midline incisions make the dissection tougher and susceptible to failure. Some surgeons report much less operating time, easier dissection, and fewer bladder injuries with the extraperitoneal route. This route is typically simpler as a end result of the balloon performs nearly all of the dissection. We choose the intraperitoneal strategy as a result of it allows a bigger operating space for protected, safe, snug dealing with of the suture. Furthermore, a culdoplasty or different intraperitoneal surgery may be carried out concomitantly. The intraperitoneal method begins with insertion of the 0-degree laparoscope (5 mm or 10 mm) by way of a respective 5 or 10 mm intraumbilical or infraumbilical cannula adopted by intra-abdominal insufflation. Inspection of the peritoneal cavity is performed, delineating the inferior epigastric vessels, stomach and pelvic organs, pelvic adhesions, and coexisting belly or pelvic pathology. Two extra trocars (a 5 mm and a 5/12 mm or two 5/12 mm ports) are positioned under direct visualization, one on each side, as previously noted. All trocars are nondisposable except the 5/12 mm trocar via which 5 and 10 mm devices are introduced. Some surgeons backload the suture by way of 5 mm ports and introduce and remove needles via the pores and skin incisions. However, trauma to the subcutaneous tissues and inferior epigastric vessels could result with this system. The bladder is crammed with 200 to 300 mL sterile water or saline by way of a 16 French, three-way Foley catheter (indigo carmine or methylene blue is optional). Using sharp dissection with electrocautery or harmonic scalpel, a transverse incision 2 cm above the bladder reflection between the medial umbilical folds is made. Identification of the free areolar tissue on the point of incision confirms a proper airplane of dissection. The risk of bladder harm is decreased by utilizing both blunt and sharp dissection aiming toward the posterior-superior side of the pubic symphysis. This dissection may be more difficult if prior retropubic surgical procedure has been carried out. Many investigators have modified the laparoscopic retropubic colposuspension using various numbers and forms of suture, synthetic mesh, staples, bone anchors, coils, tacks, fibrin sealant, and radiofrequency. Consequently, we suggest performing the procedure similar to the open method, utilizing only suture. Various suturing and needle gadgets have been used to simplify laparoscopic suturing and knot-tying, which are the most tough skills to purchase laparoscopically however could also be facilitated with robotic assistance. The Burch procedure may be performed via a small laparotomy incision with good long-term success and minimal morbidity. Utilization of the Burch process significantly decreased with introduction and utilization of the midurethral sling procedures. This method begins with an infraumbilical incision and modified open laparoscopy. After the anterior sheath of the rectus fascia is incised, a finger is swept across the rectus muscle over the posterior rectus sheath and into the preperitoneal house. The area of Retzius is dissected by tunneling the tip of the dissector to the posterior superior side of the pubic symphysis. Two additional ports are positioned beneath direct vision lateral to the inferior epigastric vessels, taking particular care to avoid entry into the peritoneal cavity. Burch Colposuspension After the area of Retzius is uncovered, the surgeon locations two fingers within the vagina and identifies the urethrovesical junction by putting gentle traction on the Foley catheter. With elevation of the vaginal fingers, the vaginal wall lateral to the bladder neck is uncovered by utilizing a laparoscopic blunt-tipped dissector. As recommended by Tanagho (1976), no dissection is performed inside 2 cm of the bladder neck to keep away from bleeding and injury to the periurethral musculature and nerve supply. The exterior iliac vessels are positioned roughly 1 cm lateral to the obturator canal, and 7. Additionally, arterial and venous anastomotic networks between the inferior epigastric and obturator vessels have been described on this anatomic area (Drewes et al. With simultaneous vaginal elevation, the suture is tied with six extracorporeal square knots. Two granny half-hitches (equivalent to a surgical knot) and a flat square knot secure the stitch. Of note, when performing a concurrent paravaginal restore with a Burch colposuspension, we suggest performing the paravaginal defect restore first. The goal is to elevate bilaterally the vaginal wall to the level of the arcus tendineus fasciae pelvis in order that the bladder neck is supported and stabilized by the vaginal wall that acts as a hammock between each "white traces. When double-armed needles are used, application of two 5/12-mm ports can streamline the procedure. A surgeon can use one port for suture and needle introduction and the opposite port for needle exit and knot-tying. The second stitch is removed and extracorporeal knot-tying is carried out after placement of Gelfoam. A cystourethroscopy is performed after the sutures are handed to affirm ureteral patency and absence of urinary tract injury. If this process is carried out concomitantly with the Burch colposuspension, the paravaginal defect repair ought to be carried out first as a outcome of exposure of the lateral defect decreases after the Burch sutures are tied. We first place the stitch on the stage of the ischial spine after which place subsequent distal stitches as needed. After all sutures are placed and tied, transurethral cystoscopy or suprapubic telescopy is completed to doc ureteral patency and absence of sutures within the bladder. The surgeon must re-inspect the area of Retzius for bleeding whereas reducing the carbon dioxide insufflation. Clinical Results and Complications A recent Cochrane evaluation in contrast laparoscopic Burch colposuspension for treatment of stress urinary incontinence to open Burch colposuspension (Lapitan and Cody, 2012). When the Ankardal information was removed, which utilized mesh and staples throughout laparoscopic colposuspension and showed considerably higher results with open Burch (Ankardal et al. Only one trial with sixty four individuals was included in long-term analysis (Morris et al. In this trial, however, there was a >50% incontinence price after open Burch, which was much greater than that reported in other trials.
Purchase sildalis torontoStories offered on this context are often negative erectile dysfunction caused by hemorrhoids order 120 mg sildalis free shipping, full of issues, and difficulties. Positive regard and respect for the affected person are important for growth and adjustment. Aspiring medical doctors need to learn to pay attention to what their patients are saying and to understand the way in which their own feelings have an result on their perceptions and ultimately their clinical practice. How usually does a patient attempt to tell a doctor what happened in a sickness and the physician interrupts with, "What was the pain like, sharp or uninteresting Today, medical colleges are attempting to insert the missing communication expertise in medical school syllabi that may facilitate more humane patient-care supplier interaction. Research has proven how the narrative is suited to revealing worlds which are in any other case closed to professional practitioners- corresponding to those burdened with a chronic illness. It is conceivable that the narrative will enable professionals and their companies to convert tales into action which will help facilitate the provision of a model new service. There is paucity of data within the literature on how best to use storytelling as a means for gaining a holistic understanding of affected person predicaments and its impact on the person and his/her group. When affected person complaints are ignored or their expressions interrupted, the focus of attention is once more on the care supplier and the patient feels ignored. The research reported that patients appeared to be more confident and empowered, whereas physician confidence in patient self-management remained more modest. The researchers conducted 2506 interviews with sufferers and 1201 interviews with primary care suppliers in 2002 in 6 countries-the United States, United Kingdom, Canada, Germany, South Africa, and Japan. Some of the findings included: � All countries agreed that authoritarian paternalistic relationships between physicians and sufferers have been on the decline; they have been being changed by mutual partnerships. In one other examine, Dibben and Lean29 offered empirical research from a study of trust and cooperation between chronically ill sufferers and their physicians. The paper detailed fashions of belief and cooperative habits designed to aid interpretative analysis. The paper offered 16 examples from interactions noticed between patients and their care suppliers. It reported that physicians appeared to make in-clinic alternatives for constructing resilient trust relations with sufferers based mostly on widespread understanding and experience, engendering extra speedy patient compliance. The researchers cited vital affected person empowerment and improved health-care supply due to the compliance achieved. Patients want the chance to apply asking questions and interpreting the answers. Physicians have to adapt therapy plans and services that meet culturally unique needs since cultural competence is the considerate utility of cultural data to practice. The problem to health-care practitioners is to develop sensitivity that recognizes that information, understanding, and acceptance of cultural and human variety are stipulations for effective work with minority patients. It is an ethical obligation for physicians to develop sensitivity to cultural differences if they hope to make interventions that are consistent with the values of their patients. Patients could also be very sluggish to disclose information and have different expectations concerning the patient� physician interaction. Patients may come to you with various beliefs associated to social roles and id. Plumpness can additionally be associated with healthiness and a large urge for food is thought to be regular in many cultures. Different individuals will place totally different emphases on the significance of healthy consuming and even upon the importance of good health itself. The awareness of the dynamics that end result from cultural differences corresponding to worth preferences, perceptions of sickness, well being beliefs, and communication fashion will assist practitioners adapt remedy plans that meet culturally unique wants. The integration of those elements into skilled determination making might improve affected person adherence. Failure of sufferers to return for visits or adhere to a health-care routine is a serious barrier to the delivery of efficient medical services. The ignorance of cultural issues will increase social distance, breaks down communication, and precipitates misconceptions between minority sufferers and their care suppliers. Contemporary interplay between care provider and affected person originated in Euro-American tradition and is grounded on a core set of values. It is a fable that these approaches are value-neutral and are relevant to all human beings. For instance, some of the values implicit in most conventional interactions include an emphasis on individualism, the separate existence of the self, individuation as the foundation for maturity, and decision making and responsibility as resting with the individual quite than the family. There is a danger of imposing these values of individual selection and autonomy as being the one "right" values and as having universal applicability. In some cultures, the key values are collectivist and consider what is good for the household. In interviews with compliant minority sufferers, they attribute their progress of adherence to a medical protocol to feelings of trust in their care provider, being understood by him/her, and the feelings engendered once they felt empowered to make knowledgeable choices on their own behalf. Health-care providers are helping sufferers kick dangerous habits and start new regimens by turning the tables on the normal doctor�patient relationship. They are using a method known as motivational interviewing, which is developed and used in the Nineteen Eighties in substance abuse and dependancy counseling. It has since been tailored for chronic illness management, medication adherence, and weight-loss counseling by well being techniques including Aetna and Weight Watchers. Doctors who lecture or give scary warnings could cause patients to turn out to be defensive and disengage. Care suppliers are being skilled to supply choices quite than prescriptions and keep away from terms similar to "should," "should," and "should. Autonomy offers the inspiration for knowledgeable consent by which a patient totally knowledgeable about her medical situation and the available options for care freely chooses to settle for or decline therapy. Two situations are essential for autonomy: (1) independence from controlling influences and (2) the ability to make decisions. The ideal of patient autonomy is that physicians should ask their sufferers in the event that they wish to obtain data and make decisions or if they prefer that their families handle such issues. The central doctrine in the area of bioethics and well being regulation is that of informed consent. Providing shoppers with information they should make knowledgeable decisions tends to promote the energetic cooperation of sufferers of their adherence plan. Informed consent occurs when a affected person is competent to act, receives a thorough (disclosure) explanation, understands the reason, is knowledgeable of obtainable alternate options, acts voluntarily, and consents to the intervention. By educating patients about their rights and duties, care providers enhance affected person empowerment and in the end affected person adherence. Whether we concentrate on threat behaviors of individuals or the suitable use of the most recent biomedical know-how, consideration to behavior results in better outcomes. Behavioral interventions and treatments have largely been ignored as cost-effective methods to identify and alter health-related behaviors. There are efficient interventions that improve food plan, enhance participation in diabetes screening programs, reinforce behaviors that prevent added risks for harm to the diabetic patient, and promote self-management of diabetes. Behavioral interventions might help change physician conduct, cut back stress-related visits to providers, and decrease client turnover.

Purchase sildalis 120 mg free shippingThe endopelvic fascia (also referred to as the anterior pubocervical fascia and posterior rectovaginal fascia) contributes to the integrity of the wall of the vagina zantac causes erectile dysfunction buy discount sildalis line. All pelvic support defects-whether anterior, apical, or posterior-represent a break in the continuity of the endopelvic fascia and/or a lack of its suspension, attachment, or fusion to adjacent structures. The targets of pelvic reconstructive surgical procedure are to appropriate all defects, thus reestablishing vaginal support at all three ranges, and to preserve or restore regular visceral and sexual operate. Operative Technique for Laparoscopic Sacral Colpopexy Operative Setup and Instrumentation Patent positioning is particularly essential for laparoscopic and robotic instances. A padded strap may be positioned throughout the chest to further secure the affected person (Alistrap, AliMed, Inc. Shoulder braces are another choice, but these have been related to brachial plexus injuries in some circumstances. Careful attention is paid to extremity positioning to stop peripheral nerve accidents. The arms are tucked with the draw sheet with the wrist in a neutral, thumbs-up place. If wanted, padding of the ulnar prominence and sled arm boards are used to further safe the arms. The lateral knee near the fibular prominence is usually padded to reduce threat of nerve harm in skinny sufferers. The monitor screens must be placed laterally to the legs in direct view of the surgeon standing on the opposite aspect of the table. The scrub nurse must be within the heart if two monitor screens are used; otherwise, the scrub nurse is situated behind one surgeon and the electrosurgical unit or the harmonic scalpel on the opposite facet. After the three-way Foley catheter and uterine manipulator (if needed) have been placed, the vaginal tray with cystoscope is set aside, if needed, for later use. A sterile pouch hooked up to each thigh is equipped with generally used devices, corresponding to unipolar scissors, bipolar cautery, graspers, and laparoscopic blunt-tipped dissectors. For the standard suturing technique, the needle holder desire is set by comfort of the surgeon. Conventional and 90-degree self-righting German needle holders (Ethicon Endo-Surgery, Inc. However, the handles are difficult to maintain and may pop open after extended use. Disposable suturing devices, such as the Endo-stitch (Covidien Surgical, Dublin, Ireland), have been launched, however extracorporeal knot-tying is preferred due to technical facility and the flexibility to hold more rigidity on the suture. The alternative of an open-ended or close-ended knot pusher for extracorporeal knot-tying depends on surgeon desire. Some surgeons have chosen to keep away from knot-tying altogether by securing the mesh with a barbed suture (Quill by Angiotech, Vancouver, B. The use of barbed sutures is currently under investigation and is being compared to the standard laparoscopic or robotic-assisted suturing approach (Tan-Kim et al. Although using barbed suture may greatly enhance efficiency, there are potential risks of bowel obstruction with using barbed suture to close the peritoneum and vaginal cuff. Lumbosacral osteomyelitis and spondylodiscitis are uncommon but devastating issues of sacral colpopexy. Less than 30 instances are currently reported within the literature, and most are associated to sutures, not tacks, positioned within the presacral space (Grimes et al. Bone tacks, nevertheless, may penetrate the intervertebral disc or disc house to a larger depth than suture and could, theoretically, lead to lumbosacral osteomyelitis and spondylodiscitis. Both reusable and disposable ports could also be secured with circumferential screws to stop port slippage. Intraperitoneal Anatomy Assessment After the insertion of a 0-degree laparoscope (5 or 10 mm) by way of a respective 5 or 10 mm intraumbilical or infraumbilical cannula followed by intra-abdominal insufflation, an inspection of the peritoneal cavity is performed, delineating the inferior epigastric vessels just lateral to the medial umbilical folds, stomach and pelvic organs, pelvic adhesions, and coexisting stomach or pelvic pathology. Two further trocars (5/12 mm disposable trocars) are placed beneath direct visualization in the right and left decrease quadrants, lateral to the inferior epigastric vessels, and one or two additional 5 mm ports are positioned on the degree of the umbilicus, lateral to the rectus muscle, as previously noted. After the position of the ancillary ports, the key anatomic landmarks of sacral colpopexy are noted: the center sacral artery and vein; the sacral promontory with anterior longitudinal ligament; the aortic bifurcation and the vena cava (at the L4 to L5 level); the right common iliac vessels and proper ureter (at the proper margin of the presacral space); and sigmoid colon, which is at the left margin. The left frequent iliac vein is medial to the left frequent iliac artery and could be broken throughout dissection or retraction. The rectovaginal septum is the posterior level of attachment of the sacral colpopexy mesh. The pubocervical fascia is the anterior point of mesh attachment during sacral colpopexy. During a sacral colpoperineopexy, the dissection is carried right down to the perineum and bilateral levator ani muscle tissue to which the inferior and lateral segments of a T-shaped mesh are attached. We use two further trocars: a 5/12 mm disposable trocar with reducer in the proper decrease quadrant (if knot-tying from the right) lateral to the right inferior epigastric vessels and a reusable 5 mm port or a further 5/12 mm disposable trocar, with reducer in the left lower quadrant lateral to the left inferior epigastric vessels. Trocars are placed laterally to the rectus muscle, roughly three cm medial to and above the anterior superior iliac backbone. Anterior dissection is performed (taking care to keep away from injury to the bladder) if a mesh is to be sutured to the pubocervical fascia or if enterocele repair is needed. Sponge sticks have been positioned within the vagina (superiorly) and rectum (inferiorly). Before re-peritonealization, the mesh extends from the vagina to the sacral promontory. Suture may additionally be passed through a number of sigmoid epiploica and brought via the left decrease quadrant lateral to the left decrease quadrant port site with a Carter Thomason suture carrier. Both suture ends are secured with minimal tension on the skin floor with a Kelly clamp, retracting the sigmoid laterally. Once the sigmoid is adequately retracted, the peritoneum overlying the sacral promontory is incised longitudinally with laparoscopic scissors and extended to the cul-de-sac. A laparoscopic dissector or hydrodissection is used to expose the periosteum of the sacral promontory. If blood vessels are encountered through the dissection, coagulation or clip placement is used to obtain hemostasis. Some surgeons choose to first dissect the presacral space, thus eliminating essentially the most technically difficult portion of the procedure. A Halban process or Moschcowitz culdoplasty could also be carried out based on surgeon desire or when a deep cul-de-sac is famous. Performance of a culdoplasty is controversial as a result of review of the literature shows no improved treatment or decreased danger of recurrence with concomitant culdoplasty at the time of sacral colpopexy (Nygaard et al. A 15 � 4 to 5 cm light-weight, macroporous, polypropylene mesh is introduced by way of a 5/12 mm port. The mesh is sutured anteriorly to the vaginal apex with two to three pairs of sutures. Efficiency of mesh arm placement may be improved by first inserting the suture, after which back-threading the mesh via the suture ends on the abdominal surface. We sometimes use 2-0 polydioxanone distally, closest to the bladder base, adopted by continued use of 2-0 polydioxanone or 2-0 polypropylene more proximal to the vaginal apex.
Buy cheapest sildalis and sildalisSecretagogues (lubiprostone and linaclotide) accelerate transit and ease of defecation by stimulating a web efflux of ions and water into the intestinal lumen erectile dysfunction medicine purchase 120 mg sildalis free shipping. Biofeedback Patients with rectal evacuation issues manifested only by a hold-up of markers in the rectum through the colonic transit research as nicely as these sufferers with defecation problems diagnosed by balloon or anorectal manometry testing ought to be managed with biofeedback-augmented pelvic floor therapy. Biofeedback strategies goal to instruct sufferers the way to adequately contract the abdominal wall whereas relaxing the pelvic floor muscular tissues throughout defecation. In hyposensory patients, sensory training may be utilized by steadily reducing the quantity of the rectal balloon, allowing sufferers to acknowledge earlier sensations of rectal filling. Controlled trials show that pelvic floor retraining with biofeedback is simpler in sufferers with defecatory problems than in sufferers with sluggish colonic transit. One research demonstrated that 71% of sufferers with dyssynergic defecation however solely 8% of sufferers with isolated gradual colonic transit achieved sufficient aid after biofeedback remedy (Chiarioni et al. Additionally, some sufferers with sluggish colonic transit seem to enhance after pelvic ground remedy and biofeedback remedy, reinforcing the idea that delayed colonic transit could also be secondary to pelvic ground dysfunction (Chiarioni et al. Moreover, three controlled studies confirmed that biofeedback remedy is more effective than polyethylene glycol (Chiarioni et al. These trials used 5 to six training sessions lasting 30 to 60 min at 2-weekly intervals. In summary, biofeedback remedy is essential in managing evacuation disorders because of pelvic flooring dysfunction. In up to 41% of sufferers, stomach pain will persist after surgical procedure, 14% of sufferers will develop diarrhea and/or fecal incontinence, and up to 18% will develop an adhesionrelated small bowel obstruction. Thus, sufferers who fail medical administration are candidates for subtotal colectomy with ileorectal anastomosis. Sacral Nerve Stimulation It has lengthy been appreciated that patients present process sacral neuromodulation for urinary problems also see improvement in bowel dysfunction. Because of this, sacral neuromodulation has been used for patients with constipation resistant to conservative remedy for over 10 years. Although the mechanism of motion is unclear, there are findings that neuromodulation alters the representation of the lower gastrointestinal tract in the sensory cortex. Test stimulation was profitable in 42% to 100% of sufferers, and of those that proceeded to permanent implant, up to 87% confirmed an improvement in bowel symptoms with a median follow-up of 28 months. Symptomatic improvement also correlated with enchancment in quality of life and total satisfaction. Most antagonistic occasions are much like those seen in fecal incontinence and are related to reprogramming, ache, or an infection. Defecatory Disorders Dyssynergic Defecation Surgical division of the pelvic floor or sphincter muscular tissues has been tried for nonrelaxing or paradoxical puborectalis contraction. However, long-term enchancment is seen in few patients, and biofeedback has turn into the mainstay of treatment for this drawback. Surgical Treatment Surgical therapy for sufferers with constipation could be divided into procedures for gradual transit constipation and for defecatory issues. Rectal Prolapse Rectal prolapse or intussusception could be entirely internal (occult) or external and protrude via the anal sphincter advanced. Patients with rectal prolapse and constipation ought to endure a complete analysis earlier than surgical procedure. If diffuse slow-transit constipation is found, a colectomy with ileorectal anastomosis and rectopexy will be the process of choice. Patients with a normal transit and delicate constipation may benefit from a sigmoid resection with a colorectal anastomosis and rectopexy. Operative selections include colectomy with ileosigmoid, ileorectal, or cecorectal anastomosis. Ileorectal anastomosis seems to be the process with the best efficacy in correctly chosen patients (Hassan et al. Ileosigmoid anastomosis appears to result in persistence or recurrence of slow transit constipation, whereas anastomosis to the center or lower rectum could lead to abnormally high stool frequency and sometimes fecal incontinence (Pemberton et al. Symptoms of rare and tough evacuation are more than likely to improve after colectomy with ileorectal anastomosis. This is a situation that leads to the protrusion of the posterior vaginal wall and anterior rectal wall into the lumen of the vagina. Although scientific examination has demonstrated good sensitivity within the detection of rectoceles, there appears to be no correlation between bowel perform and the scale of the rectocele. Thus, indications for surgical repair of rectocele are variable and never well outlined. Because of this, investigators have tried varied exams to obtain perception into important dynamic data that may or could not enhance with surgery. Defecography is helpful in determining dimension and place of rectoceles, perineal descent, rectal intussusception, and pelvic floor dyssynergia. However, there are limitations utilizing this imaging modality in sufferers with rectocele. For occasion, knowledge on whether size of a rectocele on defecography correlates with signs are conflicting. Although defecography is useful in evaluating how well a person evacuates the rectum, no correlation is discovered between ladies who retain contrast and signs of defecatory dysfunction or scientific outcome of surgical repair. Defecography could additionally be useful in patients with pelvic flooring dyssynergia, however the results of this on the outcomes of rectocele restore are contradictory. Outcomes of surgical intervention for rectocele are restricted by a lack of standardized definitions within the literature. Gynecologists usually function on patients who are suffering from the presence of a vaginal bulge or particular symptoms, similar to splinting. Investigators need to standardize subjective, anatomic, testing, and world satisfaction outcomes on this area. Conclusion Constipation is a standard, complex constellation of symptoms with unclear pathophysiology that may produce gentle or incapacitating symptoms. Further laboratory, anatomic, and practical testing rely upon the history and bodily examination and the response to initial remedy. If the initial evaluation is regular or adverse, an empiric trial of fiber (and/or dietary changes) can be adopted by over-the-counter osmotic or stimulant laxatives. Most laxatives (and dietary fiber) are usually efficient, cheap, and safe even for long-term use. Behavioral remedy ought to be offered to patients with a documented defecatory disorder; if unresponsive, surgical therapy could additionally be provided. For sufferers with continued constipation, newer agents such as secretagogues must be thought-about. Sacral neuromodulation may enhance sufferers with constipation refractory to conservative therapies. Women with a rectocele current with complicated scientific photos and infrequently report blended gynecologic and anorectal signs. Lack of standardized definitions and unclear information regarding testing modalities complicate the suitable medical or surgical administration in these sufferers. Colonic lavage solution (polyethylene glycol electrolyte lavage solution) as a therapy for continual constipation: a doubleblind placebo-controlled examine. An examination of the reliability of reported stool frequency within the prognosis of idiopathic constipation.
References - Yamazaki K. Pulmonary welldifferentiated fetal adenocarcinoma expressing lineage-specific transcription factors (TTF-1 and GATA-6) to respiratory epithelial differentiation: an immunohistochemical and ultrastructural study. Virchows Arch 2003;442:393-9.
- Fujita K, Fukuhara T, Munemasa M, et al. Ampulla cardiomyopathy associated with aneurysmal subarachnoid hemorrhage: report of 6 patients. Surg Neurol 2007; 68:556-561.
- Shankar-Hari M, Deutschman CS, Singer M. Do we need a new definition of sepsis? Intensive Care Med. 2015 May;41(5):909-911.
- Buznikov GA, Lambert HW, Lauder JM. Serotonin and serotonin-like substances as regulators of early embryogenesis and morphogenesis. Cell Tissue Res. 2001;305:177-186.
- Loeb S, Shin SS, Broyles DL, et al: Prostate Health Index improves multivariable risk prediction of aggressive prostate cancer, BJU Int 120:61n68, 2017.
- Fries BC, Riddell SR, Kim HW, et al. Cytomegalovirus disease before hematopoietic cell transplantation as a risk for complications after transplantation. Biol Blood Marrow Transplant. 2005;11: 136-148.
- Clayton HA, Davies JE, Pollard CA, et al. Pancreatectomy with islet autotransplantation for the treatment of severe chronic pancreatitis: the first 40 patients at the Leicester general hospital. Transplantation 2003;76:92-8.
|

