|
James L. Thomas, DPM, FACFAS - Associate Professor of Orthopaedic Surgery,
- Department of Orthopaedic Surgery,
- West Virginia University School of Medicine,
- Morgantown, WV
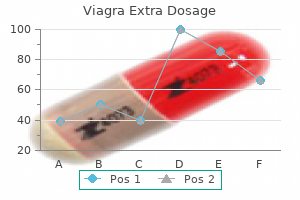
Viagra Extra Dosage dosages: 200 mg, 150 mg, 130 mg, 120 mg
Viagra Extra Dosage packs: 10 pills, 20 pills, 30 pills, 40 pills, 60 pills, 90 pills, 120 pills, 180 pills

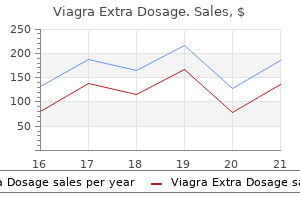
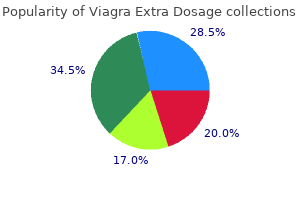
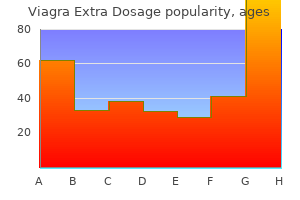
Buy 120mg viagra extra dosage fast deliveryIn one study kratom impotence order viagra extra dosage 150 mg, van Vledder et al discovered 23% of patients receiving preoperative chemotherapy had at least one disappearing liver metastases. Similarly, Benoist et al, reported the presence of residual disease on the web site of a radiologic complete response in 82%. Allows for in vivo gauge of chemoresponsiveness, facilitating postoperative chemotherapy planning 4. For instance, should sufferers be treated until disease is resectable or to a maximal response It is probably going that residual visible disease is of bene t in figuring out all preliminary websites that must be resected to forestall recurrent illness. Should patients endure surgical procedure at the moment or wait till some disease turns into radiologically evident Novel strategies for native ablation have been developed with a objective of accelerating the variety of sufferers eligible for local, doubtlessly curative remedy. With this system, a needle-probe is inserted inside the selected tumor underneath picture steerage and electric present is employed to generate heat, resulting in interstitial thermal destruction. While doubtlessly promising, these newer ablative modalities await larger managed reports to decide their function in therapy of hepatic colorectal metastases. Tumor sizes bigger than 3 cm are related to an increased incidence of local recurrence. Liver metastases positioned close to major vascular pedicles which have to be salvaged are perfect candidates. In one report, 5- and 10-year general survival rates were 33% and 23%, respectively in initially unresectable sufferers who subsequently underwent resection. Optimally, the electrode is advanced in a monitor parallel and within the plane of the transducer, so the complete path of the needle can be visualized. Typically, local miniscule gas bubble formation results in hyperechogenicity within the handled tissue. In most circumstances, a local recurrence is characterized by an increase in the lesion size on serial scans, or evidence of recent areas of contrast enhancement. Local recurrence charges printed within the literature range from less than 10% to as excessive as 40�50%. One should notice, nonetheless, that important prognostic and treatment-related variables di er between the two cohorts compared retrospectively. While response rates are excessive with this method, even following tumor development on systemic therapies, the biliary toxicity and technical aspects of implanting and maintaining an hepatic arterial pump have limited its applicability in current practice beyond few centers with expertise in this strategy. Preoperative and intraoperative assessment and planning are necessary to achieve secure and complete resection of all evident illness. Current strategies for rising the ability to o er liver resection embrace preoperative chemotherapy, staged resection, preoperative portal vein embolization, and ablative methods. Perioperative chemotherapy might play a task in the optimal remedy of initially resectable illness, however the sequencing of chemotherapy and surgery stays unclear. Minimally invasive approaches for resection, including laparoscopic resection, will likely be increasingly utilized, as well as other nonextirpative methods. However, until the position of cytoreduction or incomplete native therapies is de ned, full, curative-intent remedy should be advocated. Annual report to the nation on the standing of cancer, 1973�1999, that includes implications of age and aging on U. Accuracy of 16-channel multi-detector row chest computed tomography with skinny sections within the detection of metastatic pulmonary nodules. Radiologic imaging modalities within the prognosis and administration of colorectal most cancers. Performance of imaging modalities in diagnosis of liver metastases from colorectal cancer: a systematic evaluation and meta-analysis. Preoperative positron emission tomography to consider potentially resectable hepatic colorectal metastases. Trends in nontherapeutic laparotomy rates in patients undergoing surgical therapy for hepatic colorectal metastases. Impact of microscopic hepatic lymph node involvement on survival after resection of colorectal liver metastasis. Patient variability in intraoperative ultrasonographic characteristics of colorectal liver metastases. Predicting factors of sudden peritoneal seeding in regionally advanced gastric most cancers: indications for staging laparoscopy. Evaluation of the position of laparoscopic ultrasonography in the staging of oesophagogastric cancers. Laparoscopic staging in chosen sufferers with colorectal liver metastases as a prelude to liver resection. Selection of sufferers for resection of hepatic colorectal metastases: expert consensus statement. Shifting from clinical to biologic indicators of prognosis after resection of hepatic colorectal metastases. Hepatectomy for resectable colorectal most cancers metastases-indicators of prognosis, de nition of resectability, methods and outcomes. A important evaluation of the major indicators of prognosis after resection of hepatic metastases from colorectal carcinoma. E ect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. R1 resection by necessity for colorectal liver metastases: is it nonetheless a contraindication to surgical procedure Incidence, distribution, and signi cance of hilar lymph node metastases in hepatic colorectal metastases. Should hepatic metastatic colorectal most cancers patients with extrahepatic illness undergo liver resection/ablation Liver resection for metastatic colorectal most cancers in sufferers with concurrent extrahepatic illness: ends in 127 sufferers treated at a single center. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the pure history. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Long-term outcomes after hepatic resection for colorectal metastases in young patients. Survival after hepatic resection for metastatic colorectal most cancers: tendencies in outcomes for 1,600 sufferers during twenty years at a single institution. Rates and patterns of recurrence following curative intent surgical procedure for colorectal liver metastasis: a global multi-institutional evaluation of 1669 sufferers. Prognostic variables for resection of colorectal cancer hepatic metastases: an evolving paradigm. In uence of surgical margin on kind of recurrence after liver resection for colorectal metastases: a singlecenter expertise. Bene ts of surgery for patients with pulmonary metastases from colorectal carcinoma. Long-term results after resection of simultaneous and sequential lung and liver metastases from colorectal carcinoma. Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. Lymphadenectomy in colorectal most cancers liver metastases resection: incidence of hilar lymph nodes micrometastasis.
Cheap viagra extra dosage 200 mg onlineIt is useful in an try to erectile dysfunction after testosterone treatment proven viagra extra dosage 150mg localize and management the bleeding or to minimize the quantity of colonic resection. Diverticular disease causes colonic obstruction by way of either luminal stenosis because of wall edema on top of the already thick walled, brotic colon or extrinsic compression from an abscess. Small bowel obstruction can occur if a loop of small bowel turns into adherent to the in amed sigmoid colon. Caution is sensible in those with questionable underlying lively diverticulitis significantly if sophisticated by localized perforation. Direct visualization and histological exclusion of malignancy are mandatory but at times di cult. Management of colonic obstruction on this setting is determined by the mode of presentation and the medical tness of the patient. An insidious onset is characterized by pain, rising constipation, and the passage of ribbon-like stools. In those sufferers deemed un t for surgery, the endoscopic or uoroscopic deployment of a colon stent is a helpful various process with a excessive clinical success price. Most small (<5 cm) pericolic abscesses can be handled medically with bowel rest and antibiotics. More just lately, laparoscopic lavage and drainage have been taken up with enthusiasm by a quantity of teams with some promising results. Abdominal pain is the most common symptom, a ecting 70% of sufferers, whereas 10% are asymptomatic. Treatment is beneficial early, preferably soon after presentation, because of the high complication rate. Surgical therapy may both require a diverticulectomy or segmental resection, and the end result is normally good. Contrast enemas are notably helpful for demonstrating the presence and course of an enteric stula. Barium ought to be avoided in the emergency setting, as the results of barium-induced peritonitis are catastrophic. It is extremely operatordependent, however it can be used to insert drains and to measure the response of the abscess to drainage. It is normal apply following decision of the rst episode of diverticulitis to assess the colon for extent of disease and to exclude colorectal malignancy. Care have to be taken to anticipate full decision of the assault as an in amed colon is straightforward to perforate; also, at times colonoscopy may be very di cult or inconceivable due to in ammatory adhesions. Classi cation of Diverticulitis e Hinchey classi cation is a helpful grading system for diverticulitis. Management e majority of sufferers with acute diverticular illness may be managed conservatively with intravenous antibiotics. A mixture of metronidazole and cipro oxacin or a broad-spectrum antibiotic similar to meropenem or amoxicillin and clavulanate (Augmentin) is mostly used. Even then, caution ought to be exercised, as a signi cant minority of patients whose principal symptom is chronic ache will proceed to be symptomatic after resectional surgery. A giant population-based examine just lately has shown only a few patients going on to have surgery after initial conservative treatment of diverticulitis. Attempts have been made to stratify the management of diverticular disease by pathological and radiological means. Ultimately, the broad spectrum of illness encountered makes dogmatic statements about intervention unreliable, and sound clinical judgment remains to be required to determine when to intervene. Indications for operative intervention are di erent in two affected person subgroups: these younger than 50 years and the immunocompromised. Patients with polycystic kidney disease have a very excessive incidence of colonic diverticular illness. In some centers, routine colonic screening of sufferers awaiting renal allografts is carried out. Patients must be rehydrated with an intravenous infusion; in septic patients a urinary catheter is invaluable for assessing an sufficient hourly urine output. Other supportive measures include oxygen therapy, adequate opioid analgesia, and antimicrobial therapy. Early oral feeding could begin when tolerated, and a change to oral antibiotics may be made with indicators of decision of in ammation. In nearly all of patients, this conservative therapy will lead to the resolution of symptoms. Surgery is principally directed at controlling peritoneal sepsis and must be tailored to each scenario. Even in the face of advanced peritoneal signs, a number of sufferers will respond to these measures and keep away from the requirement for surgery. Resection of the a ected colon is related to a decrease morbidity and as much as 3 times much less mortality compared with nonresection procedures. More recently with the advances in laparoscopic surgical procedure, lavage and drainage of Hinchey types 1�3 have been efficiently performed. When bowel continuity is restored after a Hartmann procedure, whole sigmoid colectomy plus removing all of the diverticula- bearing colon and a rectal anastomosis has been proven to cut back the danger of recurrence by some107,a hundred and fifteen but not others. Laparoscopic surgical procedure in colon cancer is oncologically equivalent to the open strategy with better cosmesis, much less analgesic utilization, and shorter hospital stays. In over 1100 patients reported over the last 5 years, the postoperative complication rates vary from 7. Conversion charges range between four and 14%, working time from 141 to 300 minutes, and return of bowel activity takes between 2 and 2. In growing nations the peak incidence is in males within the 40- to 60-year age group that account for as much as 90%. Redundancy of a colon is due to both colonic dysmotility, excessive ber intake, or a genetic predisposition. Volvulus in Western society is often seen in institutionalized, bed-bound aged patients with an acquired megacolon. When an operation is required, the quality of the surgical procedure seems to be more essential than whether or not the operation is undertaken open or laparoscopically. Further potential trials investigating recurrence charges, and specifically threat components for recurrence, in addition to the function of prophylactic surgical procedure within the varied subgroups is required. Cecal bascule is a variant of the true cecal volvulus with the di erence being an absence of the axial twist but rather the redundant cecum folds again transversely and upward over the ascending colon. Chapter 32 Diverticular Disease and Colonic Volvulus 659 Presentation Colonic volvulus generally presents with bowel obstruction, vomiting, obstipation, belly pain, and distension. Signs of peritonitis typically point out underlying complications of perforation or gangrene. Complications Perforation of the twisted segment of bowel (closed-loop obstruction) or bowel ischemia and infarction could happen. Secondary renal failure or multiorgan failure may arise because of third-space loss or loss from vomiting. Alternatively, this could be due to reperfusion damage after the volvulus is untwisted.
Buy genuine viagra extra dosage lineFor these tumors 5�10 cm impotence journal buy viagra extra dosage 200 mg cheap, 70% native management was achieved, but for tumors larger than 10 cm, only 40% sustained a sturdy response. Similar outcomes have been reported by Papillon and Chassard at Centre Leon Berard in France. Again, those with tumors higher than 5 cm in dimension fared significantly worse, with overall survival rates lower than 50%. Overall, local control rates of 52�87% are typical, with 5-year general survival charges starting from fifty two to 90%. Small numbers and retrospective design limits direct comparability of this method to surgery alone. Even so, Staging and Prognosis Like melanoma of the skin, anorectal melanoma is staged by depth or thickness of the lesion. Lymphatic metastases can happen within the inguinal, mesorectal, and inner iliac nodal distribution. Mesorectal lymph node metastases are found in 40�60% of sufferers at initial presentation and inguinal Chapter forty two Cancer of the Anus 893 adenopathy is current in at least 20% of patients. Regardless of stage, 5-year survival charges for patients diagnosed with anorectal melanoma are very poor, averaging about 6%. Most authors now recommend extensive local excision with negative margins for these sufferers with out anal sphincter involvement. Roumen in the Netherlands additionally reported an increased rate of native recurrence with native excision, but no total survival disadvantage. External beam irradiation for symptomatic pelvic and local recurrences and metachronous inguinal nodal illness has been included into the palliative remedy of anorectal melanoma, however again, no information are available to assess total e cacy. Although adjuvant chemotherapy is shown to be e ective in cutaneous melanoma, lack of data hinders acceptance of this remedy in anorectal melanoma. It confers a survival bene t on this group, bettering disease-free survival charges. Erythematous, pruritic, scaling plaques with well-de ned serpiginous borders are a typical characteristic of the illness. A colonoscopy and prostate examination are fundamental preventive and diagnostic tests that can be helpful. Often, the process creates massive defects that will require pores and skin grafts or aps (rotational, island, or myocutaneous). Because excision to adverse margins is critical to cure, strategies to guarantee this may be required. Surgeons might acquire frozen sections of the margins of the specimen within the operating room previous to reconstruction. Others favor to cowl the wound with saline-soaked gauze, admit the patient to the hospital, and await everlasting pathology outcomes for up to 2�3 days prior to reconstruction. If a large ap reconstruction is placed within the anal canal, some suggest diversion with a colostomy or ileostomy on the time of the perineal excision. Physical examination, including a prostate and pelvic examination, and periodic colonoscopy are probably prudent. Biopsies of recent lesions on the edges of the ap or graft might reveal residual disease. Although the natural historical past of these lesions is poorly understood, the etiology is assumed to be much like that of condyloma. Instead, they destroy surrounding tissue by growth quite than direct invasion. Deaths from untreated BuschkeL�wenstein tumors have occurred following deep invasion into unresectable pelvic structures adopted by superinfection and recurrent sepsis. Chapter forty two Cancer of the Anus 895 long-term therapy, together with one affected person who would have required hemipelvectomy with limb amputation to obtain unfavorable margins. Interferon- 2b may be a good different or complement to radical resection in select circumstances. In: World Health Organization International Statistical Classi cation of Diseases and Related Health Problems. Longterm prognosis after radical treatment for squamous-cell carcinoma of the anal canal and anal margin. Anal squamous intraepithelial lesions in human immunode ciency virus-positive women and men. Other elements corresponding to pleomorphism, tumor necrosis, and in ltration of muscularis propria and signs are indicative of extra aggressive behavior, but e ects on survival are much less clear. Local recurrence is frequent after limited resection, as a lot as 60% in a single collection,104 whereas radical resection yielded 100% recurrence-free survival. Treatment is primarily medical, with chemotherapy directed on the tumor, as properly as appropriate antiretroviral remedy. Use of external beam radiation has also been described for cutaneous anal lesions. Primary chemoradiation therapy with uorouracil and cisplatin for cancer of the anus: leads to 35 consecutive patients. Fluorouracil, mitomycin, and radiotherapy vs uorouracil, cisplatin, and radiotherapy for carcinoma of the anal canal: a randomized controlled trial. Concurrent chemotherapy and intensity-modulated radiation therapy for anal canal cancer sufferers: a multicenter experience. Experience with split-course external beam irradiation +/- chemotherapy and integrated Ir-192 high-dose-rate brachytherapy in the treatment of main carcinomas of the anal canal. E ectiveness of surgical salvage remedy for patients with domestically uncontrolled anal carcinoma after sphincter-conserving remedy. Salvage abdominoperineal resection following combined chemotherapy and radiotherapy for epidermoid carcinoma of the anus. Anal canal carcinoma: earlystage tumors < or =10 mm (T1 or Tis): therapeutic options and unique sample of native failure after radiotherapy. High-resolution anoscopy focused surgical destruction of anal high-grade squamous intraepithelial lesions: a ten-year experience. Conservative versus nonconservative therapy of epidermoid carcinoma of the anal canal for tumors longer than or equal to 5 centimeters. Results of abdominoperineal resections for failures after combination chemotherapy and radiation therapy for anal canal cancers. Malignant tumors of the anal canal: the spectrum of disease, treatment, and outcomes. Preoperative chemotherapy and radiation therapy within the administration of anal epidermoid carcinoma. De nitive irradiation and chemotherapy for radiosensitization in management of anal carcinoma: interim report on Radiation erapy Oncology Group research no. Respective roles of radiotherapy and surgical procedure within the management of epidermoid carcinoma of the anal margin. Depth of invasion, location, and measurement of most cancers of the anus dictate operative treatment. Melanoma metastatic to the colon: case series and review of the literature with outcome evaluation.
Buy online viagra extra dosageCurative resection for esophageal adenocarcinoma erectile dysfunction urethral medication order 120mg viagra extra dosage otc, evaluation of one hundred en bloc esophagectomies. Extended transthoracic resection in contrast with restricted transhiatal resection for adenocarcinoma of the esophagus. Modern 5-year survival of resectable esophageal adenocarcinoma: single institution expertise with 263 sufferers. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the mid/distal esophagus: ve-year survival of a randomized medical trial. Predicting systemic disease in sufferers with esophageal most cancers after esophagectomy: a multinational study on the signi cance of the number of concerned lymph nodes. Delayed esophagogastrostomy: a safe strategy for management of sufferers with ischemic gastric conduit at time of esophagectomy. Swanstrom Descriptions of the techniques and causes for esophageal resections are presented by three leaders in esophageal surgery, working at major, high-volume esophageal centers. A thorough evaluate of the epidemiology (such as is known) and international variations in approaches and outcomes for esophageal cancer remedies is made by Dr Law who points out the ever-increasing differences between the Western and Eastern hemispheres. In the East and Middle East, mid and proximal squamous cell cancers are by far essentially the most prevalent, related to the persistence of carcinogenic environmental exposures. It is more related to the incredibly speedy development in the incidence adenocarcinoma-now probably the most rapidly rising cancer in North America. Dr Law presents the arguments towards screening very well-basically, too uncommon a cancer in too giant an "at-risk" inhabitants. There remains a movement, nonetheless, that argues strongly for screening of high-risk people. Save the plain holdout,7 there seems to be a gradual move to a more aggressive node-removing strategy with a very gradual shift in outcomes information to support higher cancer outcomes with en bloc resection at the worth of markedly elevated operative morbidity. The majority of institutions, nevertheless, are confronted with the referral dilemma engendered by the perception of esophagectomy being a extremely morbid process, with poor long-term quality of life and having no survival advantage over chemoradiation. An precise quote from a quantity one medical periodical states "Recent trials fail to establish any vital benefit associated with the routine use of surgical procedure for many sufferers. As each Dr Sugarbaker and Dr Luketich have emphasised, esophagectomy is all about the particulars. Our group has explored the potential of using laparoscopy or thoracoscopy to replicate en bloc esophagectomy in a less morbid way-either by transhiatal laparoscopic en bloc esophagectomy for distal tumors or thoracoscopic formal en bloc resections. While the latter is perhaps irrefutably true, but not insurmountable, the time factor may require progressive thinking to overcome. Our current protocol requires laparoscopic staging, celiac/hepatic node dissection, left gastric division, and placement of a feeding jejunostomy. Changes in the thoracic portion of the process are an attention-grabbing change from a normal strategy. Cadier has popularized the efficiency of the thoracic mobilization in the susceptible place. A nal remark is made relating to the width of the gastric conduit or "neoesophagus. We have favored a slender conduit as per Akiyama, all be it at a cost of a better leak price due to elevated intraluminal pressures during the period of mucosal edema. Surgery has been sluggish to react to this modification and is in danger of changing into increasingly irrelevant within the face of improvements in noninvasive early most cancers therapies (mainly endoscopic), de nitive chemoradiation, and, in the future, extremely focused novel therapies. It is sweet that leaders in the eld are exploring improvements in commonplace surgery outcomes as nicely as novel minimally invasive approaches-providing patient-friendly alternate options will assist ensure the continued relevancy of surgeons in esophageal cancer treatments. E cacy of Nissen fundoplication versus medical remedy in the regression of low-grade dysplasia in patients with Barrett esophagus: a potential examine. A histologically de ned subset of high-grade dysplasia in Barrett mucosa is predictive of related carcinoma. En bloc esophagectomy reduces local recurrence and improves survival in contrast with transhiatal resection after neoadjuvant remedy Perspective on Malignant Esophageal Disease 439 9. Elective surgical procedure for ulcer disease has largely been deserted in favor of medical administration with surgical procedure being utilized primarily for complications after failed medical remedy. Most elective (and some emergent) gastric procedures can now be carried out with laparoscopy if native experience is on the market, augmented by both radiologic (mainly by way of intra-operative ultrasound) or endoscopic guidance for more accurate localization. Epidemiological knowledge indicate that the prevalence of an infection in the United States has been declining because the second half of the 19th century, with the decreases corresponding to improvements in sanitation. Direct transmission from individual to person occurs through saliva and feces, and infection also occurs via contact with contaminated water. Because spontaneous treatment is unusual for most contaminated individuals, which means H. Antral gastritis is present histologically in patients with duodenal ulcer, and H. Gastric metaplasia of the duodenal bulb is a nonspeci c response to injury, which develops after infestation of the gastric mucosa. Gastric metaplasia is extraordinarily widespread in duodenal epithelium surrounding areas of ulceration. Half of patients evaluated for dyspepsia have histologic proof of bacterial infection. In developed countries, one- fth of wholesome volunteers harbor the micro organism, and the incidence of bacterial infestation will increase with age in the healthy, asymptomatic population. Noninvasive methods embody the urea breath check, serology, and detection of antigen in stool samples. Overall outcomes have been corresponding to these obtained utilizing the urea breath test methodology. During endoscopy, antral biopsies could be obtained and the organism cultured in agar containing each urea and a pH-sensitive colorimetric agent. More than 2000 articles report the results of antibiotic trials, and numerous abstract articles and meta-analyses are available. It is necessary to note that none of the therapeutic regimens reported to date cure H. To be e ective, antimicrobial drugs have to be mixed with gastric acid secretion inhibitors or bismuth salts. Chapter 21 Benign Gastric Disorders 445 decreases the prevalence of metronidazole-resistant H. Dyspepsia is among the many most typical disorders encountered by primary care physicians and gastroenterologists in the United States and Western nations. It is estimated that roughly 25% of the inhabitants will expertise dyspepsia and that this problem accounts for 5% of visits to major care providers. Symptoms might include heartburn, however a symptom complex limited to this grievance suggests gastroesophageal re ux disease and excludes the diagnosis of dyspepsia. Investigation of nonulcerative dyspepsia and its therapy represent a big financial burden.
Buy viagra extra dosage 200mg lowest priceDe nition of the cause is essential as prognosis depends on the underlying liver illness erectile dysfunction in females generic viagra extra dosage 150 mg with amex, and a full analysis to permit improvement of a remedy plan for variceal bleeding, ascites, or end-stage liver illness is paramount at initial presentation. Nicolai Eck, a Russian Army surgeon, performed an end-to-side portacaval shunt in 1883 in an animal mannequin. Pavlov, the good Russian physiologist, conducted animal studies that showed the detrimental e ect of diverting portal ow, describing meat intoxication (encephalopathy) and liver failure. Vidal, a French surgeon is credited with performing the rst portal systemic shunt in a human in 1903. Morison and Talma operated on patients with portal hypertension with procedures such as omentopexy and splenic transposition, but their failure to recognize cirrhosis as the reason for portal hypertension led to poor outcomes. In the Forties, Whipple and the Columbia Presbyterian group in New York initiated an period of success for portal e subsequent 40 years saw many re nements decompression. Endoscopic therapy was the next main advance in managing variceal bleeding, being rst done by surgeons with inflexible esophagoscopes. Another surgeon, Steigmann,eleven moved the eld ahead by introducing variceal band ligation. Over the last three decades, the newer advances have been made by nonsurgeons. A higher understanding of the pathophysiology, the ability to better consider liver diseases, the introduction of pharmacologic remedy, improvement of the radiologic shunt, and coming of age of liver transplantation are the principle contributors to this progress. Lebrec and his colleagues within the Eighties introduced beta-blockers to cut back portal hypertension,12 and this has turn into the primary therapy for lowering the chance of an preliminary variceal bleed and rst-line remedy for many who have bled. However, two surgeons, Starzl14 and Calne,15 revolutionized the whole eld of hepatology with their persistence in growing liver transplantation through the 1960s to Eighties, and bringing it to a clinical actuality. Transplantation has not only o ered a therapy for sufferers with end-stage liver illness and portal hypertension, however has additionally opened the doors to further investigation. It is round this history of portal hypertension that many of the investigative and treatment choices mentioned in this chapter are constructed. It is necessary for the managing physician to understand these pathophysiologic modifications and their influence on patient care. An important distinction in sufferers with portal hypertension is between these with ascites and encephalopathy, that are markers of superior liver illness, and patients with variceal bleeding, which can happen in patients with a traditional liver (portal vein thrombosis) or early in the midst of cirrhosis. Worldwide, schistosomiasis is a crucial etiology Portal vein Hepatic vein Extrahepatic Sinusoid 1. In the United States and Europe, most sufferers have a sinusoidal block secondary to cirrhosis. Chapter 47 Portal Hypertension 983 of portal hypertension, occurring primarily in the Middle and Far East and South America. It is characterised by brosis of the terminal portal venules, and in the absence of concurrent hepatitis, these sufferers have normal liver function. Whatever could be the etiology of the cirrhosis, full analysis of exercise and stage of the illness is a vital part of preliminary patient analysis. Di erent etiologies may have different pure histories which is essential in developing a remedy plan. Imaging is initially with ultrasound to present general liver morphology and doubtlessly to choose up focal lesions suggestive of hepatoma. Liver biopsy may be required to con rm that some patients do have underlying cirrhosis, and in instances of focal lesions, to di erentiate hepatocellular carcinoma from regenerative nodules. In the latter case a biopsy of the uninvolved liver is carried out as nicely as the focal lesion to assess for cirrhosis. Vascular anatomy is evaluated with imaging modalities of escalating complexity relying on information required for management. Documenting dimension, directional ow, velocities, and wave-form patterns of the portal and hepatic veins is a normal procedure. Tributaries to the portal vein-the superior mesenteric and splenic veins, and huge collaterals such as the coronary and umbilical vein may be readily de ned. Hepatic artery patency, course, and resistive index may be assessed with Doppler ultrasound. Finally, angiography still performs a job for direct stress measurement and clari cation when the prior modalities are unclear. Direct portal stress measurement additionally could be carried out by the transjugular, transhepatic route. Jaundice, ascites, encephalopathy, and malnutrition de ne a affected person with end-stage liver illness. Laboratory tests add objectivity, essentially the most useful indicators being serum bilirubin, albumin, prothrombin time, and creatinine. Speci c serologic markers could also be helpful in de ning etiology for viral hepatitis, or for a few of the metabolic diseases with antimitochondrial antibody, iron studies, 1-antitrypsin, or ceruloplasmin levels. Endoscopy ought to focus on the presence of varices; the size, extent, and tortuosity; and the presence or absence of purple color signs. Following an acute variceal bleed, the extent of varices must be assessed after stabilization. Grading techniques for varices have been developed and validated by the Japanese25 and Italians. Pharmacologic remedy plays a job in preventing the preliminary bleed, managing the acute variceal bleed, and as rst-line remedy in preventing rebleeding. Noncardioselective beta-blockers (Inderal [propranolol hydrochloride] or nadolol) have been shown by Lebrec and his colleagues within the early Eighties to cut back portal hypertension. Not all patients tolerate beta-blockers or are responsive to them, with a noncompliance or fallout fee of about 20%. Many different pharmacologic brokers have been evaluated similar to long-acting nitrates, serotonin antagonists, and calcium channel blockers. None of these have been proven to be as e cacious because the beta-blockers, and whereas combination remedy has been bene cial in some studies, it has been limited by facet e ects. It has been largely replaced by terlipressin, or somatostatin or considered one of its analogs. Endoscopic Therapy e present commonplace for endoscopic therapy for esophageal varices is endoscopic banding. Multiband ligators could be tted on the end of the endoscope and allow the ring of six to eight bands in a spiral style onto columns of Chapter forty seven Portal Hypertension 985 varices. Endoscopic banding can be utilized in the patient with acute variceal bleeding if the bleeding varix may be identi ed. A course of banding-usually two to three sessions-is then applied over the subsequent month to 6 weeks in an try and obliterate the varices on the gastroesophageal junction. Many potential, randomized managed trials have documented better control of bleeding with endoscopic banding than sclerotherapy, with decrease morbidity.
Langwort (White Hellebore). Viagra Extra Dosage. - Dosing considerations for White Hellebore.
- What is White Hellebore?
- Treating cholera, gout, hypertension, and herpes (cold sores).
- How does White Hellebore work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96361
Cheap generic viagra extra dosage ukEvaluation of probability of bile duct stone presence by using of non-invasive procedures erectile dysfunction gene therapy treatment buy viagra extra dosage 150mg amex. Ultrasonic analysis of frequent bile duct stones: potential comparison with endoscopic retrograde cholangiopancreatography. Preoperative ultrasonographic evaluation of the quantity and dimension of gallbladder stones: is it a helpful predictor of asymptomatic choledochal lithiasis Diagnosis of frequent bile duct stones by intravenous cholangiography: prediction by ultrasound and liver perform tests in contrast with endoscopic retrograde cholangiography. Abnormal widespread bile duct sonography: the best predictor of choledocholithiasis before laparoscopic cholecystectomy. Scoring system to predict asymptomatic choledocholithiasis earlier than laparoscopic cholecystectomy: a matched case-control research. Predictive elements for synchronous widespread bile duct stones in patients with cholelithiasis. Selection standards for preoperative endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy and endoscopic remedy of bile duct stones: results of a retrospective, single heart examine between 1996�2002. Role of endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in patients present process laparoscopic cholecystectomy. Noncontrast helical computed tomography versus endoscopic ultrasound for suspected choledocholithiasis and common bile duct dilation: a prospective blind comparability. Prospective evaluation of magnetic resonance cholangiography in sufferers with suspected widespread bile duct stones earlier than laparoscopic cholecystectomy. Magnetic resonance imaging of the frequent bile duct to exclude choledocholithiasis. Evaluation of magnetic resonance cholangiography within the management of bile duct stones. Treatment of bile duct stones: value of laser lithotripsy delivered through percutaneous endoscopy. Percutaneous transhepatic papillary balloon dilatation as a therapeutic option for choledocholithiasis. Methods, indications, and results of percutaneous choledochoscopy: a sequence of 161 procedures. Gallbladder motility and lithogenicity of bile in sufferers with choledocholithiasis after endoscopic sphincterotomy. Duodenoscopic sphincterotomy for widespread bile duct stones in patients with gallbladder in situ. Fate of the gallbladder with cholelithiasis after endoscopic sphincterotomy for choledocholithiasis. Risks of leaving the gallbladder in situ after endoscopic sphincterotomy for bile duct stones. Impact of gallbladder status on the outcome in patients with retained bile duct stones handled with extracorporeal shockwave lithotripsy. Clinical utility of a new mechanical lithotripter for smashing widespread bile duct stones. Outcome of mechanical lithotripsy of bile duct stones in an unselected sequence of 704 sufferers. Electrohydraulic lithotripsy in 111 sufferers: a protected and e ective remedy for di cult bile duct stones. Extracorporeal shock wave lithotripsy for clearance of bile duct stones proof against endoscopic extraction. Randomized research of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for di cult bile duct stones. Long-term follow-up after treatment of widespread bile duct stones by extracorporeal shock-wave lithotripsy. Fluoroscopically guided laser lithotripsy versus extracorporeal shock wave lithotripsy for retained bile duct stones: a prospective, randomised research. Extracorporeal shock wave lithotripsy for di cult widespread bile duct stones: preliminary New Zealand expertise. Endoscopic treatment mixed with extracorporeal shock wave lithotripsy of di cult bile duct stones. Extracorporeal shockwave lithotripsy of common bile duct stones without preliminary endoscopic sphincterotomy. Biliary sphincterotomy plus dilation with a big balloon for bile duct stones that are di cult to extract. Treatment of non-extractable frequent bile duct stones with mixture of ursodeoxycholic acid plus endoprostheses. Biliary endoprostheses in elderly sufferers with endoscopically irretrievable common bile duct stones: report on 117 patients. Retained common bile duct stones: a comparability between biliary stenting and full clearance of stones by electrohydraulic lithotripsy. Long-term follow-up of sufferers with gallbladder in situ after endoscopic sphincterotomy for choledocholithiasis. Choledocholithiasis in non-cholecystectomized patients: Endoscopic sphincterotomy and afterwards. Late biliary problems after endoscopic sphincterotomy for widespread bile duct stones in patients older than 65 years of age with gallbladder in situ. Endoscopic management of widespread bile duct stones leaving the gallbladder in situ: a cohort research with longterm follow-up. Evaluation of the biliary tree throughout laparoscopic cholecystectomy: laparoscopic ultrasound versus intraoperative cholangiography: a prospective examine of 150 cases. A prospective comparability of laparoscopic ultrasound vs intraoperative cholangiogram throughout laparoscopic cholecystectomy. Primary closure versus Ttube drainage after laparoscopic choledochotomy for common bile duct stones. Laparoscopic transcystic bile duct stenting in the management of common bile duct stones. Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and peroperative endoscopic sphincterotomy. Choledochoduodenostomy, transduodenal sphincteroplasty and sphincterotomy for calculi of the frequent bile duct. Choledochoduodenostomy an necessary surgical tool in the administration of widespread bile duct stones: a review of 126 instances. Choledochoduodenostomy and sphincterotomy in the therapy of choledocholithiasis. Long-term results of choledochoduodenostomy within the remedy of choledocholithiasis: evaluation of 225 cases. Long-term follow-up of sufferers with side-to-side choledochoduodenostomy and transduodenal sphincterosplasty. Long-term follow-up after choledochojejunostomy for bile duct stones with complex clearance of the bile duct. A strategy of biliary tract reconstruction with full follow-up in forty four consecutive cases. Recurrent biliary stricture: patterns of recurrence and outcome of surgical therapy. Laparoscopic choledochoduodenostomy: an e ective drainage procedure for recurrent pyogenic cholangitis.
Syndromes - Check blood flow in the veins
- Coma
- Stroke
- Bleeding
- The need to have a bowel movement
- Strep throat
- Severe headache
Buy generic viagra extra dosage canadaAnd final impotence yahoo answers generic 150mg viagra extra dosage visa, excessive ranges of luminal IgA and greater distribution of lymphoid tissue within the small intestinal epithelium and submucosa could provide a further protective mechanism via an immune surveillance mechanism. Bile acids and their metabolites have been implicated in the pathogenesis of small bowel adenocarcinoma. Carcinoids are unusual tumors in Asian collection, 611 612 Part V Intestine and Colon Postcholecystectomy patients could additionally be at larger threat for the event of small bowel malignancy. In one examine of sufferers with small intestinal malignancy, 12% had a historical past of cholecystectomy, and of those with duodenal adenocarcinoma, 25% had prior cholecystectomy. However, a causative relationship between cholecystectomy and small intestinal adenocarcinoma stays unproven. High-Risk Population Several heritable and in ammatory gastrointestinal situations are associated with an increased risk for development of small bowel tumors. Patients on chronic immune suppression remedy are at specific threat for small bowel malignancies, especially lymphomas and sarcomas. Most are extranodal and the gastrointestinal tract is the involved site in 10�25% of circumstances. In most sequence, the average length of symptoms prior to prognosis ranges from weeks to many months. Initial evaluation to exclude more frequent situations, including evaluation of the gastroduodenum, colon, and biliary tract are accomplished, but, when adverse, further evaluation of the small bowel is delayed or deferred. Benign lesions hardly ever cause stomach pain or obstruction; quite, their presence is often heralded by acute gastrointestinal hemorrhage. Benign neoplasms may develop to a big measurement prior to detection and will simply be discovered by the way on a radiological examination or at laparotomy. Such ndings, while rare, would warrant resection somewhat than bowel-preserving approaches. In addition to the fact that these are uncommon tumors that produce nonspeci c gastrointestinal complaints, the power to fully picture and observe the small gut is proscribed. Despite the introduction of capsule endoscopy, which allows for luminal visualization of the whole small bowel mucosal floor, correct preoperative prognosis is in reality unusual previous to surgical procedure. Abdominal mass, heme-positive stool, or indicators of intestinal obstruction are often absent. Celiac disease is associated with elevated threat of lymphoma and is seen in as much as 14% of patients. Surveillance is indicated, as these lesions are susceptible to malignant transformation into adenocarcinoma. Tumors of the distal small bowel may trigger jejunoileal or ileocolic intussusception. During intussusception, the small bowel tumor serves because the lead point to pull the small bowel into the distal small bowel or colonic lumen; the mass lesion precludes spontaneous reduction. Rather, prompt surgical exploration and resection of the nonreduced intussuscepted bowel phase with mesenteric resection should be completed without intraoperative makes an attempt at complete discount; quite, the intestine ought to be lowered gently to the palpated lead level, adopted by intestinal resection and primary anastomosis. Attempts at full reduction usually lead to inadvertent enterotomy or publicity of a perforation within the intussusception. A small bowel follow-through examine will show an abnormality in 53�83% of instances, although direct proof of a tumor is detected in solely 30�44%. Intraoperative enteroscopy permits a means more full evaluation of the small bowel. While diagnostic strategies continue to enhance, many patients with small bowel neoplasms still have preliminary presentation as a surgical emergency, and more than half of patients with malignant illness have metastatic spread on the time of operation. Half the patients with benign tumors are symptom free, and most might be diagnosed at the time of presentation with a surgical emergency such as obstruction, gastrointestinal hemorrhage, or perforation. Gastrointestinal bleeding is the commonest presenting complication, presumably a consequence of spontaneous necrosis when the benign lesion outgrows the obtainable blood supply. Increased dimension correlates with malignant potential, and excision is suggested when prognosis is established, often as an incidental nding. Adenomas larger than 2 cm in diameter must be considered worrisome for malignancy. In these circumstances ultrasound will reveal evidence of biliary obstruction, prompting upper endoscopy with endoscopic retrograde biliary and pancreatic duct analysis (endoscopic retrograde cholangiopancreatography), which is able to reveal the presence of the ampullary lesion. Endoscopic ultrasound is changing into important in the analysis of duodenal adenomas to consider depth and to determine if mucosal excision or surgical resection is extra applicable. Transduodenal native excision for small lesions is appropriate, whereas lesions larger than three cm in dimension have a high price of associated malignancy and are most appropriately handled with either pancreas-sparing duodenectomy, or pancreaticoduodenectomy for larger lesions or periampullary tumors in appropriate operative candidates. Adenomas As in the colon, small bowel adenomas are histologically classi ed as tubular, tubulovillous, or villous. Local recurrence is common for periampullary adenomas handled with excision only: 40% at 10 years, 25% of which had been malignant, in a latest retrospective sequence from the Mayo clinic. For those handled with excision solely, annual surveillance with endoscopy is suitable. Small tumors beneath 2 cm require no intervention, whereas bigger lesions or growing lesions should be resected to rule out malignant liposarcoma. Malignant tumors are much more likely to elicit symptoms than benign tumors, together with belly ache, weight loss, anorexia, and acute or chronic blood loss. As a bunch, sufferers with malignant small bowel tumors current at advanced stages and have a poor prognosis. Up to 30% of patients with small bowel malignancy develop a second primary tumor in another organ. Large tumors form the traditional circumferential annular "apple core" constriction resulting in obstruction with symptoms of anorexia, vomiting, and crampy ache. Arising from the submucosal vascular plexuses, hemangiomas are often solitary and never at risk for malignant transformation. Hemangiomas related to bleeding ought to be regionally excised or resected with a restricted small bowel resection. Endoscopic sclerotherapy or angiographic embolization has also been reported as a treatment possibility relying on the scale and place of the tumor. Metastatic tumors could come from some other cancer, but the most typical metastatic lesions are from melanoma and lymphomas. In absent advanced or strategically placed lesions with obstruction, the only complaint may be obscure, persistent abdominal pain. Most small bowel lymphomas are distributed within the jejunum and ileum re ecting the distribution of lymphoid tissue in the bowel. At surgical procedure, disease have to be restricted to the first tumor with mesenteric lymph node involvement. Despite diagnostic methods, preoperative prognosis of cancers beyond the duodenum is achieved in solely 20�50% of circumstances. Many sufferers have intra-abdominal metastases at preliminary surgery, with R0 resection (ie, no gross or microscopic disease left) achieved in only 50�65% of cases. In the third and fourth portions of the duodenum and within the mesenteric small bowel, a segmental resection with lymphadenectomy should be carried out. Palliative procedures to relieve obstruction or management hemorrhage ought to be completed at the time of exploration for patients with metastatic disease.
Viagra extra dosage 130mg without prescriptionOften health erectile dysfunction causes order viagra extra dosage 200mg amex, clear uid (in the unfed patient) may be seen welling up within the space and should lead one to a laceration of the thoracic duct. In such cases, the leak should be repaired directly with pledgeted 4-0 Prolene sutures. Prophylactic ligation of the thoracic duct following esophagectomy is usually carried out. In this maneuver, all tissue between the aorta, backbone, and azygos vein on the stage of the hiatus is ligated with a large (0 or 1) ligature. A triglyceride level greater than 1 mmol/L is strongly suggestive of a chyle leak, as is a lymphocyte rely greater than 90%. If chylomicrons may be con rmed by electrophoresis, the prognosis can additionally be established. A good bedside check entails feeding the affected person cream enterally 200�300 mL over 2 hours and observing for a change in character of chest tube e uent, from serous to milky white. Once the analysis is con rmed, and even if it is strongly suspected, patients ought to be brought to the operating room and the thoracotomy incision reopened. A cautious inspection for other leaks must be carried out before closure, and mass ligation of the duct at the hiatus ought to be thought-about as well. In a broadcast trial of 42 sufferers (including 9 postesophagectomy patients), the thoracic duct might be embolized in 26 and sixteen of those cases have been cured. Meta-analyses have shown that estimates of blood loss are barely larger with the transthoracic group versus the transhiatal group. Intraoperatively, arterial branches from the aorta to the esophagus should be clipped every time potential. If blunt dissection is used, staying immediately in opposition to the esophagus should assist keep away from bigger arteries, because the esophageal arterioles are most likely to type a ne plexus of vessels roughly 1�2 cm away from the wall of the esophagus. A notorious web site of bleeding through the transhiatal dissection is the azygos vein or certainly one of its branches. A widespread website of bleeding after any thoracotomy is the chest wall itself, including intercostal vessels; these should be inspected after eradicating the retractor. Impaired Conduit Emptying Numerous elements a ect conduit emptying postesophagectomy. Studies objectively taking a glance at conduit emptying following esophagectomy give con icting results as to the e ect of pyloroplasty on gastric conduit emptying time. A prospective trial studied 200 sufferers and randomized half to pyloroplasty and half to no pyloroplasty following Ivor Lewis esophagectomy. Six months after the procedure, gastric emptying was 6 minutes in the pyloroplasty group versus 24 minutes within the group without pyloroplasty. A thin gastric tube has been proven to have a decrease incidence of symptoms related to poor gastric emptying (3%) than sufferers both with the whole abdomen (38%) or distal two-third abdomen (14%) performing because the conduit. Excess conduit length or angulation may also impair emptying, and extra colon conduit length or angulation is thought to cause quick or delayed issues with emptying. Analysis of the relationship between quantity and mortality reveals a big variance in mortality from virtually 25% in low-volume and low-experience facilities to as little as 2. Excision of the thoracic esophagus for carcinoma of the esophagus with construction of an ex-trathoracic gullet. Carcinoma of the decrease thoracic esophagus: report of a profitable resection and esophagogastrectomy. Staging of carcinoma of the esophagus and cardia: a comparison of di erent staging criteria. Chemoradio-therapy adopted by surgery in comparison with surgery alone in squamous-cell most cancers of the esophagus. Randomized trial of preoperative chemoradialion versus surgery alone in sufferers with locoregional esophageal carcinoma. Staging of esophageal cancer with 18- uorodeoxyglucose positron emission tomography. Improvement in staging of esophageal cancer: 100 consecutive positron emission tomography scans. Transthoracic versus transhiatal resection for carcinoma of lhe esophagus: a meta-analysis. Oesophagectomy by a transhiatal approach or thoracotomy: a potential randomized trial. A prospective randomized comparison of transhiatal and transthoracic resection for lower-third esophageal carcinoma. Management of unremitting chylothorax by percutaneous embolization and blockage of retroperitoneal lymphatic vessels in forty two sufferers. Delayed postoperative emptying after esophageal resection is dependent on the scale of the gastric substitute. Cancer of the esophagus: esophagogastric anastomotic leak-a retrospective study of predisposing components. Comparison of hand-sewn and stapled esophagogastric anastomosis after esophageal resection for most cancers. Benign anastomotic strictures after transhiatal esophagectomy and cervical esophagogastrostomy: threat components and management. Transthoracic esophagectomy with radical mediastinal and stomach lymph node dissection and cervical esophagogastrostomy for esophageal carcinoma. While proponents of minimally invasive surgical procedure declare decreases in perioperative pain and size of stay, critics often specific concerns over compromised outcomes, prolonged operating instances, and increased value. These stories and the advantages of minimally invasive surgery perceived by the common public have increased referrals to surgeons who offer these approaches to esophageal issues, even though different medical therapies can be found. Concerns concerning the excessive diploma of technical complexity, vital operator learning curves, reproducibility of outcomes in lower-volume facilities, and equivalence of oncologic outcomes are on the forefront of the discussion. Despite evolving techniques and enhancements in both the transhiatal and Ivor Lewis surgical approaches, esophagectomies are complex operations which are associated with significant morbidity and mortality. Furthermore, surgical candidates are sometimes elderly sufferers with coexisting medical comorbidities, including respiratory and cardiovascular diseases. Nationwide, the mortality charges from esophagectomies range from 8% in high-volume centers to as excessive as 23% in low-volume facilities. First, open esophagectomy, even in skilled facilities, continues to be related to a big morbidity, lengthy hospital stay, and 19 delay in returning to preoperative actions. Consequently, for some patients, different approaches corresponding to definitive chemoradiation alone, palliative photodynamic remedy, or stents could also be chosen by well being care providers. Minimally invasive approaches to esophagectomy that promise to lower perioperative morbidity and permit for sooner postoperative recovery are, therefore, interesting to sufferers and referring physicians. There has been a big evolution in approach because the initial descriptions of hybrid approaches to esophagectomy that employed thoracoscopic esophageal mobilization with a laparotomy. In this chapter, we evaluate our experience with minimally invasive surgical procedure for esophageal cancer, as well as detail surgical methods for several different ailments of the thoracic esophagus, corresponding to resection of benign esophageal tumors and thoracoscopic treatment of esophageal dysmotility. Laparoscopic approaches to different advanced esophageal operations, together with achalasia and paraesophageal hernia, are coated in Chapters 14 and 15.
Order 130mg viagra extra dosage mastercardPatients with sphincter of Oddi stenosis are vulnerable to erectile dysfunction treatment with viagra discount 200 mg viagra extra dosage overnight delivery (1) frequent bile duct obstruction from brosis and stenosis of the papilla, (2) recurrent pancreatitis, and (3) recurrent proper upper quadrant belly pain in the absence of jaundice or pancreatitis. Many instances are thought to be brought on by trauma from the passage of multiple small stones or sludge from the common bile duct by way of the ampulla, leading to in ammation, brosis, and stricture formation. Patients with di use stricturing from 5- uorouracil are managed by simple discontinuation of infusion, and in some cases percutaneous transhepatic drainage. Surgery must be reserved for patients with persistent evidence of biliary obstruction. Presentation Primary sclerosing cholangitis is predominantly a disease of young males. Approximately 70% of sufferers are male, and the typical age at the time of analysis is 40 years. Other widespread symptoms may include proper higher quadrant ache, weight reduction, fever, pruritus, and fatigue. Despite its name, a minority have acute cholangitis, and blood cultures are not often constructive, approximately 10% are very symptomatic at the time of diagnosis; nonetheless, asymptomatic sufferers can have deceptively advanced illness. Patients could have an elevated alkaline phosphatase, and during exacerbations may have elevated bilirubin. At the time of diagnostic cholangiography, brushings for cytology must be obtained to help distinguish between benign and malignant strictures. Patients ought to be monitored intently with cholangiography, liver biopsy, and cytologic brushings, to detect disease development and improvement of malignancy or biliary cirrhosis. Most medical therapies are aimed toward symptomatic relief or antibiotic therapy in the setting of cholangitis. Cytologic brushings at the time of endoscopy should also be obtained to investigate for cholangiocarcinoma. Operative biliary reconstruction with transhepatic stenting for primarily extrahepatic and/or hilar disease in noncirrhotic patients has been demonstrated to have wonderful longterm outcomes. Primary indicators for referral for liver transplant include persistently elevated bilirubin or decreased high quality of life from disabling fatigue, severe pruritus, muscle wasting, or bacterial cholangitis. Resection of the hepatic duct bifurcation at the aspect of long-term transhepatic stenting in noncirrhotic sufferers with primarily extrahepatic and/or hilar disease can delay or even stop the need for hepatic transplantation. Transplant is really helpful in patients with primarily intrahepatic strictures or advanced cirrhosis. Congenital bile duct cysts: classi cation, operative procedures, and review of thirty-seven cases together with cancer arising from choledochal cyst. Endoscopic biliary manometry in sufferers with suspected sphincter of Oddi dysfunction and in sufferers with cystic dilatation of the bile ducts. Experimental production of cystic dilatation of the common bile duct in neonatal lambs. Embryogenesis of pancreaticobiliary maljunction inferred from development of duodenal atresia. Action of pancreatic juice on the bile duct: pathogenesis of congenital choledochal cyst. Biliary manometry in choledochal cyst with abnormal choledochopancreatico ductal junction. Immunohistochemical analysis of cyclooxygenase-2 and vascular endothelial growth factor in pancreaticobiliary maljunction. Ras gene point mutations in gallbladder lesions related to anomalous connection of pancreatobiliary ducts. Proliferative potential and K-ras mutation in epithelial hyperplasia of the gall-bladder in patients with anomalous pancreaticobiliary ductal union. Nuclear cyclin D1 overexpression is a crucial event related to cell proliferation and invasive development in gallbladder carcinogenesis. K-ras and p53 gene mutations in noncancerous biliary lesions of patients with pancreaticobiliary maljunction. Laparoscopic administration of choledochal cysts: method and outcomes-a retrospective research of 35 patients from a tertiary heart. Symptomatic choledochoceles in adults endoscopic retrograde cholangiopancreatography recognition and administration. An external audit of laparoscopic cholecystectomy within the steady state performed in medical remedy services of the Department of Defense. Complications of cholecystectomy: risks of the laparoscopic strategy and protective e ects of operative cholangiography: a population-based study. Cues related to laparoscopic cholecystectomy bile duct injuries: con rmation bias could inhibit early prognosis. Morphologic, biophysical, and biochemical consequences of ligation of the common biliary duct in the canine. Microstructural and ultrastructural changes in the therapeutic means of bile duct trauma. Major bile duct injuries throughout laparoscopic cholecystectomy: follow-up after combined surgical and radiologic management. Surgical management of bile duct accidents sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Right hepatic artery injury related to laparoscopic bile duct injury: incidence, mechanism, and penalties. Bile duct injury following laparoscopic cholecystectomy: a trigger for continued concern. Long-term outcomes of a main end-to-end anastomosis in peroperative detected bile duct harm. Long-term results for biliary reconstruction after laparoscopic bile duct accidents. Long-term follow-up after bilioenteric anastomosis for benign bile duct stricture. Impaired quality of life 5 years after bile duct harm during laparoscopic cholecystectomy: a prospective analysis. Major bile duct injuries related to laparoscopic cholecystectomy: e ect of surgical restore on high quality of life. Quality-of-life evaluation of surgical reconstruction after laparoscopic cholecystectomyinduced bile duct injuries: what happens at 5 years and beyond Long-term detrimental e ect of bile duct harm on health-related quality of life. Analysis of surgical success in stopping recurrent acute exacerbations in chronic pancreatitis. Persistent obstructive jaundice, cholangitis, and biliary cirrhosis as a outcome of common bile duct stenosis in persistent pancreatitis. Medium-term results of endoscopic remedy of common bile duct strictures in persistent calcifying pancreatitis with increasing numbers of stents.
References - Grasso, M., Bagley, D. Small diameter, actively deflectable, flexible ureteropyeloscopy. J Urol 1998;160:1648-1653.
- Little WC, Downes TR: Clinical evaluation of left ventricular diastolic performance, Prog Cardiovasc Dis 32:273-290, 1990.
- Druss BG, Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA 1999;282(7):651-656.
- Minagar A, David NJ. Bilateral infarction in the territory of the anterior cerebral arteries. Neurology. 1999;52(4): 886- 888.
- Atlee JL 3rd, Alexander SC: Halothane effects on conductivity of the AV node and His-Purkinje system in the dog, Anesth Analg 56:378-386, 1977.
- Neff TA, Hudgel DW. Miliary tuberculosis in a renal transplant recipient. Am Rev Respir Dis. 1973;108:677-678.
- Pittendrigh CS, Daan S. Circadian oscillation in rodents: a systematic increase of their frequency with age. Science 1974;186:548-50.
- Gali B, Whalen FX, Schroeder DR, et al. Identification of patients at risk for postoperative respiratory complications using a preoperative obstructive sleep apnea screening tool and postanesthesia care assessment. Anesthesiology 2009;110:869.
|

