|
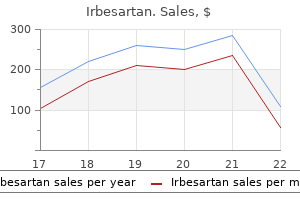
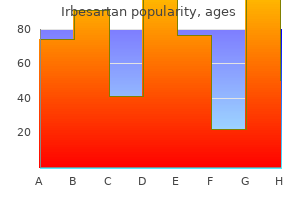
Irbesartan dosages: 300 mg, 150 mg
Irbesartan packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
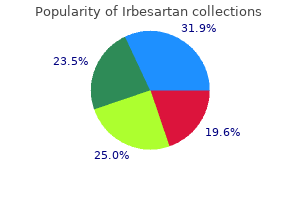
Generic irbesartan 300 mg with mastercardScaphoid delayed unions and nonunions: a potential research evaluating different treatment strategies. Vascularised bone graft from the base of the second metacarpal for refractory nonunion of the scaphoid. Chapter 20 Vascularized Bone Grafting of Avascular Scaphoid Nonunions Alexander D. Patients often complain of restricted vary of wrist movement and pain, often with grip or weight bearing. Studies of vascularity of the distal radius have recognized a quantity of sources of vascularized bone graft obtainable for nonunion remedy. Animal research of vascularized bone grafts have documented a significant enhance in blood flow present when in comparability with nonvascularized grafts. The scaphoid fracture web site fills with fibrous connective tissue and motion persists at the site of the fracture. Classic radiographic findings start at the radial styloiddistal pole of scaphoid interface and proceed to involve the complete scaphoid fossa, the midcarpal joint, and eventually the complete radiocarpal articulation. The radial styloid�scaphoid interface is the earliest website of degenerative change in scaphoid nonunions, and sufferers will often show tenderness at that location. The distal pole of the scaphoid is palpable on the base of the thumb on the palmar side of the wrist. Conflicting reviews regarding the usefulness of gadolinium enhancement have been published over the past a number of years. Investigators have tried the use of bone stimulators, which use both electrical stimulation or ultrasound. For important collapse, a nonvascular iliac crest graft could additionally be required to create a compression-resistant assemble. When early degenerative modifications are current, a radial styloidectomy should accompany using a vascularized distal radial graft. The presence of extra advanced degenerative joint disease or carpal malalignment is a contraindication to performing surgery to obtain bony union. Preoperative Planning Radiographs have to be evaluated to rule out degenerative joint modifications or carpal instability patterns, which are sometimes found in established nonunions. Positioning the patient is placed supine on the working desk with the arm positioned on an armboard. Correction of a "humpback deformity" requires intensive mobilization of the pedicle when making an attempt using a dorsally sourced graft, and a palmar vascularized graft could also be extra acceptable. Anatomic research have proven that the dorsal irrigating vessels are of higher diameter and are farther from the articular floor than irrigating vessels on the palmar surface of the radius. The irrigating department enters the distal radius and supplies bone distal and dorsal to the brachioradialis insertion. Avoidance of exsanguination earlier than tourniquet inflation facilitates its identification. The first and second compartments are unroofed on their radial and ulnar elements, respectively, to keep away from harm to this irrigating vessel. Graft Harvest the periosteum is scored with a scalpel to define the graft form, which measures 1. Graft Placement the joint capsule is incised in the distal portion of the incision and the scaphoid nonunion is identified. A radial styloidectomy significantly increases the publicity of the scaphoid and eliminates the potential for bone graft impingement. Intervening fibrous tissue and sclerotic bone are removed from the nonunion web site utilizing rongeurs and curettes to put together the scaphoid for graft placement. Cancellous bone graft from the distal radius is packed proximally and distally to fill voids created by d�briding sclerotic bone. The radial capsule is closed loosely with absorbable suture and the pores and skin is closed in a routine trend.
Buy 150mg irbesartan fast deliveryApproximately 20% of patients currently surviving have extreme phantom limb ache requiring narcotic analgesics every day. Because of the vascular nature of this flap, the surgical wound heals quickly within the overwhelming majority of sufferers. Modified hemipelvectomy: conservation of the higher iliac wing and an anterior musculocutaneous flap. The quadriceps musculocutaneous flap: a dependable, sensate flap for the hemipelvectomy defect. Femoral artery based mostly myocutaneous flap for hemipelvectomy closure: amputation after failed limb-sparing surgical procedure and radiotherapy. Hemipelvectomy for buttock tumors using an anterior myocutaneous flap of quadriceps femoris muscle. The complete thigh and rectus abdominis myocutaneous flap for closure of intensive hemipelvectomy defects. Popliteal-based filleted lower leg musculocutaneous free-flap coverage of a hemipelvectomy defect. Although most tumors of the lower extremities are amenable to limb-sparing methods, some tumors of the femur and thigh are so intensive that hip disarticulation is required for adequate tumor resection. With advances in prosthetic design, patients can ambulate with a prosthesis regardless of the bigger power expenditure wanted to ambulate after a hip disarticulation compared to more distal amputations. Even without prosthetic use, most patients are very profitable in ambulating and finishing up daily activities. Performing a hip disarticulation could additionally be extra preferable in some circumstances instead of leaving a affected person with a very quick above-knee amputation stump website, which might make prosthesis fitting tough. It may show extension into the gentle tissues, especially within the ischiorectal fossa, hip joint, and groin. Familiarity with these constructions can minimize intraoperative bleeding if they are often recognized and ligated as needed. These arteries embody the profunda artery, the medial and lateral circumflex arteries, and the obturator and superior and inferior gluteal arteries. The tensor fascia lata, gluteus maximus, and iliotibial band type an outer muscular envelope across the hip, and at least certainly one of these structures normally must be break up to acquire access to the hip. The femoral triangle should be identified to entry the primary neurovascular buildings encountered in this process. The femoral triangle is bordered superiorly by the inguinal ligament, laterally by the sartorius muscle, and medially by the adductor longus muscle. This sturdy fibrous layer covers the anterior hip to the intertrochanteric line but leaves most of the femoral neck uncovered posteriorly. The ischiorectal fossa is an area bounded medially by the sphincter ani externus and anal fascia, laterally by the tuberosity of the ischium and obturator fascia, anteriorly by the fascia masking the transversus perinei superficialis, and posteriorly by the gluteus maximus and sacrotuberous ligament. Assessment for tumor extension to this area is particularly important in planning the flaps that might be used. Bone Scan A bone scan is useful in evaluating the bony involvement of the femur, pelvis, and acetabulum. Angiography and Other Studies Angiography can help determine the external iliac, widespread femoral, and profundus arteries when making ready for surgical procedure. However, given the potential practical limitations and prosthetic wants of a hip disarticulation, a biopsy is unquestionably recommended earlier than performing a hip disarticulation. Lymph node involvement is a relative contraindication to performing a hip disarticulation until the procedure is done for palliation. Hip disarticulations are sometimes required after poor chemotherapy response or tumor aggressiveness. These conditions enhance the probability for shut surgical margins, which might result in native recurrences. If possible, fasciocutaneous flaps must be constructed to promote would healing.
Purchase irbesartan cheapAll tissues had been removed through a mix of the anterior and posterior parts of the utilitarian shoulder girdle incision. Intraoperative photograph taken before reconstruction and reattachment of the muscular tissues of the again and anterior pectoralis major. This photograph demonstrates the advantage of a transpectoralis method anteriorly mixed with a posterior method. Reattachment of the conjoint tendon and pectoralis minor to the coracoid with using mattressed, nonabsorbable sutures covers the brachial plexus and axillary vessels. Defects of the chest wall may be covered with native rotation flaps utilizing the latissimus dorsi or pectoralis major muscle, which may be tenodesed to the subscapularis tendon as wanted. Careful wound closure over closed suction drains and placement of absorptive padding within the axilla reduce the danger of pores and skin maceration and wound infection. Functional deficits resulting from resection of parts of the brachial plexus may require delayed reconstruction after completion of adjuvant remedy. Detachment of the humeral insertion is vital to opening up the complete axilla and permits exploration of all essential structures. Injury due to over-retraction of the conjoint tendon might occur, leading to lack of elbow flexion and resulting incapacity. Operative view via the anterior incision showing a big tumor surrounding the axillary sheath. Lymphedema could end in important incapacity and continual pain; early aggressive treatment might reduce the severity or duration of swelling. Infections and flap necrosis following axillary tumor resections rarely occur, because of the substantial network of subcutaneous blood vessels perfusing the shoulder girdle. Upper extremity limb salvage with microvascular reconstruction in sufferers with advanced sarcoma. Upper extremity reconstruction following resection of soft tissue sarcomas: a practical outcomes analysis. Soft tissue sarcoma of the higher extremity: a 5-year expertise at two institutions emphasizing the position of sentimental tissue flap reconstruction. Cost evaluation of useful restoration surgery for extremity soft-tissue sarcoma. Loss of shoulder movement leads to gentle disability, which is well compensated for by use of the opposite arm for overhead activities. Use of nerve sheath catheters with postopera Chapter 14 Forequarter Amputation Jacob Bickels and Martin M. Forequarter amputation often is contraindicated when the tumor extends to the chest wall or to the posterior triangle of the neck and paraspinal muscular tissues. This surgical procedure may be considered in chosen cases with no metastases, in which concomitant chest wall resection or neck dissection can obtain adverse margins and sufferers can face up to the physiologic influence of these combined main surgical procedures. All of these must be transected to enable the efficiency of a forequarter amputation. The axillary vessels and infraclavicular portion of the brachial plexus pass just inferiorly to the coracoid course of, which is well palpable, and lie below the deltopectoral fascia. These constructions must be evaluated earlier than surgery to decide the segment that can be safely transected and ligated, particularly as a end result of large tumors could come near the thoracic outlet. Large tumors of the periscapular area may easily extend into the posterior triangle of the neck, the adjacent paraspinal muscles, and the underlying chest wall. Tumor extension into these anatomic websites should be evaluated carefully before surgical procedure in case en bloc resection of a chest wall section or a concomitant neck dissection is required. Angiography is extremely useful in locating the anatomic place of the axillary and brachial vessels, and in evaluating whether these structures are concerned by tumor. Physical anomalies (eg, a duplicate axillary artery) often are recognized as properly. Angiography also makes it potential to decide precisely the best level of ligation of the axillary vessels.
Cheap irbesartan amexLeave the lateral portion of the joint intact to keep away from disrupting the blood provide to the head of the primary metatarsal. The first minimize includes eradicating the distinguished medial eminence with an osteotome, beginning distally at the sagittal groove (groove of Clark). The second reduce is made on the distal metaphyseal�diaphyseal junction of the first metatarsal. The third, proximal cut is made about 2 to 3 mm proximal to the primary cut, and is created fully throughout the first metatarsal. The prominence of the distal portion of the metatarsal shaft is smoothed off with a rongeur, and a capsulorrhaphy is carried out with absorbable sutures. Sterile dressings are applied and the toe is splinted in impartial to slight plantarflexion. The first reduce of the osteotomy is performed two thirds of the finest way via the primary metatarsal on the junction of the metaphysis and diaphysis and is oriented perpendicular to the long axis of the primary metatarsal (line 2). The second bone reduce (line 3) is made fully through the bone and completes the osteotomy. It should be made 2 to four mm proximal to the primary minimize and is perpendicular to the long axis of the second metatarsal. When seen from the medial facet, the osteotomy must be oriented so that a small plantar-based wedge is produced. This helps keep away from dorsiflexion of the distal fragment when the osteotomy is lowered. The surgeon should keep away from resecting greater than about 3 mm of bone to stop shortening of the first metatarsal. It ought to create a slight plantar-based wedge with the distal minimize to avoid dorsiflexion of the osteotomy. The modified Mitchell osteotomy (described above) produces 81% passable results, with no instances of malunion, nonunion, avascular necrosis of the first metatarsal head, an infection, or switch metatarsalgia. In older kids and adolescents there shall be painful dorsal callosities about 50% of the time. There may be issue find shoes that match appropriately in older children and adolescents. Positioning the affected person is supine, ideally with a bolster beneath the ipsilateral hemipelvis to make the lateral foot extra accessible. The plantar handle should be barely longer than the dorsal handle and directed barely laterally. The extensor tendon is split, and a dorsomedial launch of the fifth metatarsophalangeal joint is carried out. There should be no pressure on the toe, and the toe ought to relaxation throughout the plantar handle of the racquet incision. The neurovascular bundles should be protected through the process, and traction on the fifth toe is averted. It stabilizes the arch of the foot and protects the underlying neurovascular constructions from damage. During the gait cycle, the plantar fascia assists in the dynamic adjustments of the arch. At toe off the plantar fascia helps lock the midtarsal joints to help the foot to be a inflexible lever for forward propulsion. Clinical muscle testing shows that though each peroneal muscles are weak, the bigger peroneus longus muscle retains relatively extra strength. Differential peroneal nerve compression at the proximal fibula is postulated to cause relative sparing of the peroneus longus innervation. The first metatarsal turns into much more plantarflexed by the action of the peroneus longus and with time becomes fastened in this place. The cavus foot remains a rigid lever all through stance section, resulting in elevated stress and lack of shock absorption, ache, and callosities. This can lead to a relative overpull of the peroneus longus and posterior tibialis muscular tissues. Cavus right foot deformity with high arch, plantar crease, apex of deformity on the midfoot, and claw toes. If the plantar tissues tighten and turn into shorter, the fixed length of the arch forces it to become taller.
Generic 150mg irbesartan visaPlanning needs to take into consideration the outcomes of preoperative radiographs of the wrist, hand, and cervical spine in addition to electromyographic tests. If the findings on electromyography are unfavorable and the surgeon is certain that tendon rupture is responsible for the dearth of lively finger movement, plans ought to be made to transfer expendable existing tendons to people who have ruptured. If radiographs reveal important joint destruction and instability, acceptable arthrodesis or arthroplasty ought to be thought-about somewhat than tendon transfer. Instruments and suture wanted for tendon weaves and repairs are extremely priceless. The hemostat then grasps the transferred tendon, weaving it through the recipient tendon. Positioning Most tendon transfers are done with the affected person within the supine place on the operating table. The contralateral arm or decrease extremity may be sterilely draped within the event that a tendon graft is required. Make a second 2- to 3-cm incision over the mid-dorsal wrist (unless a dorsal wrist incision has already been made for another procedure). A single weave, whereas normally enough for smaller tendons, must be supplemented with an additional one or two weaves if attainable. If inadequate distal tendon is current for a weave, both an end-to-end restore or a weave in which the transferred tendon is brought by way of a transverse incision in the distal recipient stump from volar to dorsal is an efficient option. The distal incision within the palm is used to isolate the sublimis tendon as far distal as possible by flexing the finger so that the chiasm of Camper is visible within the wound. The tendon is split simply proximal to the chiasm, leaving enough distal tendon to contribute to the steadiness of the proximal interphalangeal joint in extension and thereby avoiding a secondary instability of that joint and attainable swan-neck deformity. In basic the radial path is most well-liked to minimize ulnar deviation of the digits. Adjust rigidity such that with slight wrist flexion, the fingers are maintained in full extension. Splinting the proximal interphalangeal joint in flexion postoperatively will also help to minimize the danger of creating a swan-neck deformity. The transferred tendon sits on the radius using the bone as a pulley to enhance the effectiveness of the transfer. The amount of flexion attainable is judged within the operating room by passive flexion of the finger until a minimal quantity of tension is seen at the repair website. Weave the distal flexor pollicis longus via the brachioradialis in a Pulvertaft style. Pulvertaft weave proven sequentially as a sharp tendon passer is used to puncture the tendon through and thru and then grasp the tendon being transferred and weave it by way of the recipient tendon. Carefully defend the intrinsic tendon, which can now be the only extensor for the thumb interphalangeal joint. The surgeon must pay attention to the potential threat of extensor lag, and we recommend attention to the defect by suture repair. When suturing tendon grafts at the web site of tendon weave (ie, where a graft or switch is handed via one other tendon), one or two sutures must be enough. Cutting needles should by no means be used as they place each the suture and the tendon in danger. In the case of tendon transfer to restore lack of finger extensors, the hand and wrist are immobilized with the wrist extended about forty levels. More could additionally be fascinating in sure situations, but an extreme quantity of extension might injury already fragile joints. Immobilization is continued for six weeks, at which time a mild lively range-of-motion program is begun without resistance. Tendon switch should at all times be delayed in patients with active illness as results shall be poor. The only surgical process to be performed in poorly managed patients is synovectomy, and with the caveat that success hinges on eventual good medical management of the disease. Rupture of extensor tendons by attrition at the inferior radio-ulnar joint: report of two circumstances. With good medical administration of rheumatoid arthritis, when the disease is properly managed, and in cooperative Chapter 62 Operative Reconstruction of Boutonni�re and Swan-Neck Deformities Mark Wilczynski, Martin I. The synovial tissue in rheumatoid arthritis is characterised by a proliferation of synovial lining cells, angiogenesis, and relative lymphocytosis. The lumbrical muscle (L) on the radial facet of the digit varieties the indirect fibers (O) of the extensor apparatus, which join with the lateral slip of the extrinsic extensor tendon to kind the conjoined lateral band.
Purchase irbesartan 300 mg otcAngulation of the articular surface on the lateral view is measured as the angle between a line connecting the dorsal and palmar lips of the distal radius articular surface on the lateral view and a line perpendicular to the radius shaft. Ulnar variance is a better measure of shortening of the radius than radial length. Loss of articular floor alignment may be measured on radiographs as gap, step, or subluxation. Sources of variability in radiographic measurements include variation in the radiographs, imprecision in the measurement techniques, and imprecision in the number of the points of reference. Risk components for fracture instability embrace age, metaphyseal comminution, dorsal tilt, ulnar variance, and lack of practical independence. Limitations of assorted remedy strategies could contribute to creation of a malunion. External fixation alone without ancillary percutaneous pin fixation of the fracture Early removal of pins or an exterior fixator. Lack of forearm rotation could additionally be associated to capsular contracture or bony malalignment. A malaligned healing fracture may be considered a malunion within 4 to 6 weeks of injury. Risk factors for fracture instability, loss of discount, and malunion include age over 60 years, greater than 20 degrees of dorsal angulation, dorsal metaphyseal comminution, comminution extending to the volar metaphyseal cortex, associated fracture of the ulna, and displaced articular fracture. The distance between B and D is the articular step, and the gap between A and C is the utmost articular hole. Displaced intra-articular fractures of the distal facet of the radius: long-term leads to younger adults after open reduction and internal fixation. Articular incongruity or subluxation in comparatively nonarticular areas may be reasonably properly tolerated, but in most cases intraarticular incongruity will lead to arthrosis, pain, and dysfunction. Neurophysiologic checks (nerve conduction velocity and electromyography) are ordered to consider any symptoms or indicators of carpal tunnel syndrome that may need to be addressed. It is important that there be a direct correlation of the pain with a clear operative target. Range of movement: A goniometer is used to measure wrist flexion, extension, radial and ulnar deviation, supination, and pronation. Ulnocarpal compression: the carpus is forcefully ulnarly deviated toward the ulna. Patience is warranted in plenty of conditions, notably for sufferers with ulnar-sided wrist pain thought as a end result of an extraarticular malunion. This discomfort is the last ache to go away after a distal radius fracture and routinely lasts as much as a 12 months. The surgeon should be wary of ache as the first criticism, as a result of ache is strongly influenced by psychosocial factors, and pain aid is an achievable goal only when according to an objective, correctable anatomic deformity similar to discomfort clearly related to a substantial ulnocarpal impingement. Intra-articular osteotomies ought to be thought of only when the malalignment is easy and the planned correction is straightforward. The affected person should have demonstrated glorious exercise abilities and full finger motion, and there ought to be no important nerve or tendon dysfunction or edema. In that way each contingency is anticipated and the surgery is more probably to go extra easily. Positioning the affected person is positioned supine with the arm supported on a hand table. A nonsterile pneumatic tourniquet is used and inflated after exsanguination and earlier than the skin incision. Approach the operative approach is either dorsal or volar, relying on the deformity and the chosen surgical method. The extensor pollicis longus is mobilized and transposed dorsoradially into the subcutaneous tissues. A distractor or small external fixator could facilitate realignment and provisionally stabilize the fracture. The distal threaded pin is drilled at an angle equal to the specified correction of the lateral tilt of the distal radius articular floor so that distraction of the 2 pins will bring this pin parallel to the proximal pin (perpendicular to the radius), thereby restoring alignment. The pins should be drilled so that additionally they assist restore the appropriate ulnarward inclination of the distal radius articular floor when distracted. The osteotomy is made with a noticed as close as attainable to the unique fracture site.
150 mg irbesartan with amexThis type is difficult to diagnose on plain radiographs and should go undetected for an extended time frame. Peripheral chondrosarcoma is definitely acknowledged as a large mass of characteristic calcification protruding from a bone. Correlation of the medical, radiographic, and histologic data is important for correct prognosis and analysis of the aggressiveness of cartilage tumor. In common, proximal or axial location, skeletal maturity, and pain level towards malignancy, although the cartilage may seem benign. The sites of origin and the reality that chondrosarcomas are probably to be low-grade often make them amenable to limb-sparing procedures. The 4 most typical sites are the pelvis, proximal femur, shoulder girdle, and diaphyseal parts of the lengthy bones. Variants of Chondrosarcoma There are three less-common variants of basic chondrosarcoma. Clear cell chondrosarcoma, the rarest type of chondrosarcoma, is a slow-growing, locally recurrent tumor resembling a chondroblastoma but with some malignant potential that usually occurs in adults. The most difficult medical problem is early recognition; it usually is confused with chondroblastoma. Mesenchymal chondrosarcoma is a rare, aggressive variant of chondrosarcoma characterized by a biphasic histologic pattern, ie, small, compact cells intermixed with islands of cartilaginous matrix. This tumor has a predilection for flat bones; lengthy tubular bones not often are affected. Grading and Prognosis Chondrosarcomas are graded 1, 2, and 3; most are both grade 1 or grade 2. Ten-year survival rates among these with peripheral lesions are 77% with 32% among those with central lesions. The a number of forms of benign osteochondromas or enchondromas have the next price of malignant transformation than the corresponding solitary lesions. The lesion is characterized by poorly differentiated, small, spherical cells with marked homogeneity. The clinical and biologic behavior is significantly completely different from that of spindle cell sarcomas. Within the previous 2 decades, the prognosis of patients with Ewing sarcomas has been improved dramatically because of a combination of adjuvant chemotherapy, improved radiation therapy strategies, and the choose use of limited surgical resection. Microscopic Characteristics the histologic spectrum of chondrosarcomas varies tremendously. High-grade examples are easy to identify, whereas certain low-grade tumors are exceedingly troublesome to distinguish from chondromas. Areas of elevated cellularity with extra marked variation in cell size, important nuclear atypia, and frequent pleomorphic forms define a grade 2 lesion. Grade 3 chondrosarcomas, which are relatively uncommon, present even larger cellularity, usually with spindle cell areas, and reveal prominent mitotic activity. Clinical Characteristics and Physical Examination Ewing sarcomas tend to happen in young youngsters, though rarely in those youthful than 5 years. Another unique finding with Ewing sarcomas is systemic indicators, ie, fever, anorexia, weight loss, leukocytosis, and anemia. Note the big chondrosarcoma within the left hip and a normal-appearing osteochondroma in the proper hip. The pelvis, shoulder girdle, and ribs are the most typical sites of malignant transformation of osteochondromas. Secondary low-grade chondrosarcomas, arising from osteochondromas of the proximal humerus (B), proximal femur (C), and proximal tibia (D; arrows point to the area of the cartilage cap that has undergone malignant transformation). Secondary chondrosarcoma arising from the left proximal femur in a patient with a quantity of hereditary enchondromatosis. Plain radiograph exhibits a big, benign-appearing enchondroma arising from the best proximal femur and a large, poorly demarcated cartilage tumor, arising from the left. The affected person underwent modified hemipelvectomy and remains disease-free after greater than 10 years of follow-up.
Purchase irbesartan lineInjuries to the lunotriquetral ligament happen in a spectrum of severity starting from partial tears with dynamic dysfunction (most common) to complete dissociation with static collapse. If the ligament is stretched and attenuated from persistent or inflammatory degradation, instability can occur in the absence of ligament dissociation (complete disruption). When the dorsal radiotriquetral ligament (and different secondary restraints) can be compromised and the entire ligament advanced is disrupted, carpal collapse results. Rupture of the lunotriquetral interosseous ligament and the dorsal secondary restraint. These findings illustrate the "balanced lunate" idea, which describes the lunate as torque suspended between the scaphoid and triquetrum. Through the lunotriquetral and scapholunate ligaments the 2 forces are balanced and the whole proximal carpal row is balanced concerning the lunate. Wrist arthrography displaying distinction dye pooling, indicative of a lunotriquetral ligament damage. Bone scan of a affected person with lunotriquetral ligament damage demonstrates elevated radiotracer uptake centered at the lunotriquetral joint. Real-time videofluoroscopy can illustrate the positioning of a "clunk" that happens with wrist deviation. Dorsal lunotriquetral joint tenderness ought to be elicited in lunotriquetral joint accidents. A palpable wrist click on is sometimes significant, notably if painful and occurring with radioulnar deviation. Provocative tests that demonstrate lunotriquetral laxity, crepitus, and ache are helpful to accurately localize the positioning of pathology. Three useful exams to carry out embrace: Ballottement11: the test is constructive if increased anteroposterior laxity and pain occur. Osseous accidents embody the sequelae of fractures (ie, nonunion or malunion) and degenerative processes. Fracture nonunions can affect the hamate, pisiform, triquetrum, base of the fifth metacarpal, ulnar styloid course of, and distal part of the ulna or radius. Degenerative processes at the pisotriquetral joint, midcarpal (triquetrohamate) articulation, fifth carpometacarpal joint, or distal radioulnar joint can even lead to substantial ulnar-sided wrist ache. Ligamentous injuries can happen in any of the ulnar-sided intrinsic (lunotriquetral or capitohamate) or extrinsic (ulnolunate, triquetrocapitate, or triquetrohamate) ligaments in addition to the triangular fibrocartilage complex. Lunotriquetral dissociation results in lessened triquetral movement and increased movement of the lunate, scaphoid, and distal row. Initially the wrist is immobilized in a long-arm cast for four weeks and then a short-arm solid for an additional four weeks. Acute accidents with out radiographic adjustments may be successfully handled nonoperatively. Midcarpal injections with local anesthetic and corticosteroid often present important reduction for a prolonged time. Anterior interosseous and posterior interosseous nerve neurectomies can be carried out presently as properly. The findings of the arthroscopy are mentioned with the patient at a second meeting and a reconstructive or salvage process can then be carried out 6 weeks later. Alternatively, a definitive surgical procedure can be carried out at a single surgical setting following a radical preoperative discussion with the patient. When a lunotriquetral dorsal ligament restore is planned, preparations also wants to be made to proceed with ligament reconstruction if the standard of the lunotriquetral ligament is poor. The goal of surgical procedure is to return rotational stability of the proximal carpal row and restore the pure alignment of the lunocapitate axis. Functional reconstruction of the lunotriquetral ligament may be achieved with direct ligament repair, ligament reconstruction with a strip of extensor carpi ulnaris tendon graft, or arthrodesis. Our desire, based mostly on outcomes research carried out at our institution, is tendon restore or reconstruction.
|