|
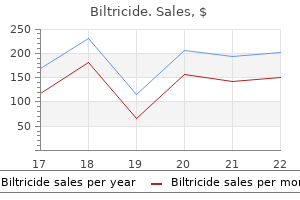
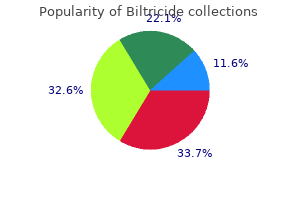
Biltricide dosages: 600 mg
Biltricide packs: 1 pills

Discount biltricide 600mg with visaTwelve patients underwent surgical reconstruction, and the remainder were managed expectantly or with percutaneous drainage with good to glorious results. Patients with recurrent strictures after reconstruction at a specialist unit may be salvaged with further intervention, both anastomotic revision or balloon dilation. Several authors have reported some measure of success with surgical revision in these patients (Chapman et al, 1995; Lillemoe et al, 1997; Stewart & Way, 1995; Tocchi et al, 1996; Walsh et al, 2004). The chance of a good end result is less than with the preliminary reconstruction, nonetheless. In the series reported by Chapman and colleagues (1995), eleven of twenty-two operative failures were treated a second time successfully and had satisfactory outcomes, but this was considerably decrease than the practically 80% success price after the preliminary repair. Other groups have reported nearly equal surgical outcomes for reoperated patients in comparison with major repairs on the similar establishment (Pottakkat et al, 2007). As mentioned beforehand, the loss of bile duct size related to a failed restore is a significant factor that limits the success of subsequent interventions. Duodenal ulceration has been reported in 10% of patients after Roux-en-Y biliary-enteric reconstruction and constitutes an extra reason for late morbidity (McArthur & Longmire, 1971; Sato et al, 1982). Most sufferers respond to antiulcer medication, but some might develop important hemorrhage. Advances in interventional radiology have resulted in a broader application of nonoperative approaches to bile duct stricture (see Chapters 13 and 52). With this technique, the biliary tree is accessed percutaneously, and a guidewire is handed through the stricture. The stricture is dilated with an angioplasty-type balloon catheter, after which a transhepatic stent is left in place for follow-up cholangiography and repeat dilation. Recent results have been encouraging, with a number of authors reporting good leads to 55% to 98% of sufferers (Lillemoe, 1997; Misra et al, 2004; Moore et al, 1987; Mueller et al, 1986; Pitt et al, 1989; Vogel et al, 1985; Williams et al, 1987). First, the imply follow-up in most of those research was lower than 3 years, which is inadequate to make a definitive remark relating to long-term efficacy. Third, complications related to balloon dilation or to the percutaneous catheter are frequent and embody hemobilia, bile leak, and cholangitis in 20% of sufferers. With this system, multiple plastic or metallic stents are placed throughout the stricture endoscopically, necessitating elimination at a later date. Other groups have reported greater success charges, albeit at shorter follow-up intervals (Kuzela et al, 2005; van Boeckel et al, 2009). As with balloon dilation, the results of stenting are tempered with caveats of short follow-up periods and no randomized studies. Comparing the results of balloon dilation or endoscopic stenting with operative reconstruction is difficult because of variations in the types of injuries selected for every sort of remedy, inconsistencies in defining successful outcomes, and variations in reporting issues and size of follow-up. In two retrospective analyses, biliary reconstruction was more likely to result in a successful consequence: 89% versus 52% (Pitt et al, 1989), 92% versus 64% (Lillemoe et al, 1997), and 94% versus 58% (Misra et al, 2004). Because balloon dilation requires multiple readmissions and repeat interventions, the overall value and morbidity appear to be just like that of operatively handled patients (Pitt et al, 1989). However, hepatic issues, together with bile leak and hepatic damage (Chow et al, 2009; Salinas et al, 2010; Zornig et al, 2009;), have occurred. Biliary Stricture and Fistula Chapter 42 Biliary fistulae and strictures 711 the umbilicus. As with any new know-how, initial results are tempered by the anticipated studying curve. Percutaneous large-bore�needle T-fasteners inserted into the gallbladder for retraction are fragile and should improve the probability of bile leakage. The evaluation by Yamazaki and colleagues (2015), inclusive of more than 5200 cases between 2008 and 2013, famous a 0. Robotic technologies have been extensively adopted by the sector of urology (Sharif et al, 2012); nevertheless, basic surgeons have been more sceptical and are solely lately implementing robotic technologies into their follow. In theory, the robot supplies the power for more refined actions and superior visualization with threedimensional views. Groups have begun reporting use of robotic surgical platforms as a salvage mechanism for completion cholecystectomy.
Purchase biltricide australiaMature flukes devour hepatocytes and duct epithelium and reside for years within the hepatic and common bile ducts and infrequently within the gallbladder. Adult fluke worms produce eggs within four months after an infection (range, 3 to 18 months); these eggs traverse the sphincter of Oddi and gut after which proceed the cycle of an infection. Contaminated water with metacercariae has been additionally described as potential source of an infection in poor rural areas with insufficient sanitation and water supplies (Cabada et al, 2014). Imported contaminated vegetables from endemic areas can be consumed by individuals dwelling in giant cities. Treatment of contaminated crops with high doses of potassium permanganate decreases metacercariae viability and could be used to forestall an infection (Ashrafi et al, 2006). Epidemiologic research have been carried out in endemic areas to measure the influence of alimentary habits on the acquisition of infection. Drinking drinks created from watercress or alfalfa leaves, known as emollients, and living close to irrigation channels have been found to be risk factors in a multivariate analysis within the Andean region (Marcos et al, 2004). In a logistic regression evaluation, an age- and gendermatched case-control study comparing 60 infected youngsters discovered that ingesting alfalfa juice carries a 4. In Mexico, aquatic vegetation and alfalfa juice have been associated with fascioliasis (Zumaquero-Rios et al, 2013). Socioeconomic components and drinking untreated water might represent extra threat elements in poor people from endemic areas (Cabada et al, 2014). Women have larger prevalence rates, more extreme infections, and extra reported liver or biliary complications (Marcos et al, 2006). Children are affected more than adults in endemic areas (Marcos et al, 2007c), which most likely displays partial acquired immunity, exposure to the metacercaria, genetic susceptibility, and different elements. Clinical Manifestations Fascioliasis has two distinct clinical phases: acute and persistent. In common, the persistent infection is normally recognized in epidemiologic research in endemic areas as a explanation for biliary obstruction or in routine stool checks. On the opposite hand, the acute an infection has a extra florid scientific picture that brings the patient to the emergency department (Table forty five. The medical manifestations are so variable that delicate proper higher quadrant stomach ache may call for a stepby-step workup that can result in the final diagnosis of fascioliasis (Behar et al, 2009). Acute Infection the primary acute or invasive section lasts from three to 5 months and is brought on by the migration of the immature larvae from the duodenum to the liver. Choledocholithiasis Eosinophiliccholecystitis Achalcolouscholecystitis *Ectopic migration and different medical manifestations. Acute stage: migratory nodule under the skin or peritoneal cavity, arthralgias, lymphadenopathies, hemolytic anemia, seizures, and pleural effusion. Migration tracks may be noticed in histologic sections, and flukes could die, leaving cavities filled with necrotic debris; these are finally replaced by scar tissue. Symptoms embody prolonged fever, hepatomegaly with belly ache, and gentle eosinophilia (early infection) or hypereosinophilia (mid- or late-acute infection). Of notice, one of the most frequent manifestations in this acute phase is hypereosinophilia, which is seen in nearly all circumstances. If no eosinophilia is detected on the initial go to, it could be too early in the acute an infection; a repeat blood cell rely three to 5 days later will detect a significant enhance in the eosinophil depend. In abstract, acute fascioliasis is a scientific syndrome similar to acute cholecystitis with vital eosinophilia. The acute section presents with subcapsular hematomas, hepatic cysts, residual hepatic calcifications, and severe anemia. Hyperbilirubinemia is absent within the acute phase (Marcos et al, 2008), which distinguishes it from other forms of acute hepatitis. Other manifestations are anorexia, weight loss, nausea, vomiting, cough, diarrhea, urticaria, lymphadenopathies, and arthralgias (Marcos et al, 2005c). Occasionally, the juvenile larvae reach other anatomic areas, such as the subcutaneous tissue, pancreas, eye, brain, and abdomen wall (Rana et al, 2007). Chronic Infection the continual part begins roughly 3 to 6 months after the consumption of the metacercariae, when the parasite reaches the bile ducts. On macroscopic examination, the liver has large, dilated, thick-walled, and calcareous bile ducts with yellowish brown bile. On microscopic examination, the bile ducts have a thickened hyperplastic wall with marked fibrosis (Haridy et al, 1999; Marcos et al, 2007c). Symptoms normally reflect biliary obstruction with colicky ache in the proper upper quadrant, epigastric area, or higher stomach (Jimenez et al, 2001; Maco et al, 2003; Rana et al, 2007).
Diseases - Hepatic ductular hypoplasia
- Kaplan Plauchu Fitch syndrome
- D-plus hemolytic uremic syndrome
- Hypothalamic dysfunction
- Megalencephalic leukodystrophy
- Hypopituitarism micropenis cleft lip palate
- Myiasis
- Glycogen storage disease type 9
Buy 600mg biltricideCopelan A, et al: Diagnosis and management of Budd-Chiari syndrome: an replace, Cardiovasc Intervent Radiol 38(1):1�12, 2015. Feng K, et al: A randomized managed trial of radiofrequency ablation and surgical resection within the therapy of small hepatocellular carcinoma, J Hepatol 57(4):794�802, 2012. Isayama H, et al: A prospective randomised research of "covered" versus "uncovered" diamond stents for the management of distal malignant biliary obstruction, Gut May 53(5):729�734, 2004. Kubo T, et al: Outcome of percutaneous transhepatic venoplasty for hepatic venous outflow obstruction after living donor liver transplantation, Radiology 239(1):285�290, 2006. Migita K, et al: Clinical consequence of malignant biliary obstruction caused by metastatic gastric cancer, World J Surg 33(11):2396�2402, 2009. Miyayama S, et al: Extrahepatic blood supply to hepatocellular carcinoma: angiographic demonstration and transcatheter arterial chemoembolization, Cardiovasc Intervent Radiol 29(1):39�48, 2006. Murkund A, et al: Percutaneous management of resistant biliaryenteric anastomotic strictures with use of a combined chopping and traditional ballon cholangioplasty protocol: a single-center expertise, J Vasc Interv Radiol 26:560�565, 2015. Nasim S, et al: Emerging indications for percutaneous cholecystostomy for the administration of acute cholecystitis-a retrospective review, Int J Surg 9:456�459, 2011. Pareja E, et al: Vascular complications after orthotopic liver transplantation: hepatic artery thrombosis, Transplant Proc 42(8):2970�2972, 2010. Rosch J, et al: Transjugular portal venography and radiologic portocaval shunt: an experimental research, Radiology 92(5):1112�1114, 1969. Tanaka T, et al: Superselective particle embolisation enhances efficacy of radiofrequency ablation: results of particle measurement and sequence of motion, Cardiovasc Intervent Radiol 36(3):773�782, 2013. Tinkoff G, et al: American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank, J Am Coll Surg 207(5):646�655, 2008. Wang X, et al: Margin measurement is an independent predictor of native tumor development after ablation of colon most cancers liver metastatses, Cardiovasc Intervent Radiol 36(1):166�175, 2013. Although open exploration for biliary disease has turn into less common, particular situations, similar to obstructive common duct stones not amenable to endoscopic therapy or restoration of biliary-enteric continuity following resection of bile duct tumors, stay indications for extra invasive approaches. It is important to have an intensive understanding of biliary anatomy and familiarity with numerous options for operative publicity and management. Operative methods encompassing bile duct exploration and biliary-enteric bypass will be the focus of this chapter. There are a variety of ductal anomalies associated to the convergence of the left and proper hepatic ducts and the insertion of cystic duct. Although the left biliary system is fairly constant, the best biliary system is prone to anatomic variation; the commonest variants include the best anterior or posterior sector ducts traversing a longer extrahepatic course before becoming a member of the left biliary system (Blumgart et al, 1984). There are a selection of strategies out there for analysis and clearance of the frequent bile duct, together with percutaneous, endoscopic, laparoscopic, and open strategies. This subset consists of patients undergoing an open cholecystectomy (or a laparoscopic cholecystectomy converted to open) during which choledocholithiasis is suspected, patients with large or multiple stones, and sufferers requiring transduodenal sphincteroplasty. A current evaluation demonstrated equal duct clearance, morbidity, and mortality between endoscopic measures and open surgical techniques (Clayton et al, 2006). Because percutaneous, endoscopic, and laparoscopic modalities are discussed in different chapters, open bile duct exploration will be the focus of the subsequent part. The intrahepatic bile ducts draining the varied sectors in the end coalesce into the proper hepatic duct draining the best hemiliver and the left hepatic duct draining the left hemiliver, which then converge on the liver hilum to type the common hepatic duct, essentially the most anterior structure of the portal triad at this location. In roughly 80% to 90% of cases, the best hepatic artery courses posterior to the common hepatic duct toward the proper liver, whereas within the minority of instances, it could be discovered anterior to the duct. Segment I hepatic ducts flow into both the best and left biliary techniques, with nearly all of drainage getting into the left hepatic duct simply proximal to common hepatic duct. Safe operative conduct requires a detailed familiarity with anatomic variations of biliary drainage, as they happen in as a lot as 25% Incision and Exposure A proper subcostal incision affords satisfactory exposure of the gallbladder, portal structures, and duodenum; alternatively, an higher midline incision may be equally effective, notably in skinny patients. Division of the lateral peritoneal attachments of the proper colon, adopted by mobilization of transverse colon mesentery off of the duodenum, provides visualization of the duodenum. Additionally, cholecystectomy can improve exposure of the hepatoduodenal ligament and may facilitate intraoperative transcystic cholangiography, which might help to delineate biliary anatomy. To avoid damage to the cystic duct, the location of cystic duct insertion ought to be recognized, as this will happen in a medial or posterior location. During the incision, warning must be taken to avoid injuring the posterior wall of the duct. The size of the choledochotomy will depend upon the diameter of the duct and measurement of stones current with the lumen but is mostly 1 to 2 cm.
Generic biltricide 600mg fast deliveryVigan� J, et al: Effects of preoperative oral carbohydrate supplementation on postoperative metabolic stress response of sufferers undergoing elective abdominal surgical procedure, World J Surg 36(8):1738�1743, 2012. Voron T, et al: Sarcopenia impacts on short- and long-term results of hepatectomy for hepatocellular carcinoma, Ann Surg 261(6):1173� 1183, 2015. Walrand S, et al: Physiopathological mechanism of sarcopenia, Clin Geriatr Med 27(3):365�385, 2011. Wakai T, et al: Surgical outcomes for hepatocellular carcinoma in nonalcoholic fatty liver disease, J Gastrointest Surg 15(8):1450�1458, 2011. Wicks C, et al: Comparison of enteral feeding and complete parenteral nutrition after liver transplantation, Lancet 344:837�840, 1994. Yang Y, et al: Resistance train enhances myofibrillar protein synthesis with graded intakes of whey protein in older males, Br J Nutr 108:1780�1788, 2012. Yoshikawa T, et al: Endotoxin-induced disseminated intravascular coagulation in vitamin E-deficient rats, Toxicol Appl Pharmacol seventy four:173�178, 1984. Zhang Y, et al: Probiotic use in stopping postoperative infection in liver transplant patients, Hepatobiliary Surg Nutr 2(3):142�147, 2013. This is due partly to a trend toward surgical specialization and centralization of care at high-volume institutions, the place the inverse volume-outcomes relationship has been properly described for many complicated procedures (Finks et al, 2011; Nathan et al, 2009; Stitzenberg et al, 2009; Valero et al, 2015). Despite the observed lower in postoperative mortality, morbidity has remained essentially unchanged, with most massive collection reporting a 35% to 45% major complication rate following either pancreatic or hepatic resection (Cameron & He, 2015; Kneuertz et al, 2012; Nathan et al, 2009; Vin et al, 2008). This widening hole between morbidity and mortality implies an improved capability to handle postoperative problems after they occur, thereby rescuing sufferers who previously would have died (Bassi et al, 2001; Sohn, 2003). This is partially as a result of earlier and more practical detection based mostly on familiarity with procedure-specific issues and advances in high-quality imaging. Another cause is the shift in administration from operative reexploration to interventional and endoscopic methods which would possibly be effective with much less added morbidity (Sohn, 2003; Vin et al, 2008). Interventional radiologists now make up an indispensible a half of the multidisciplinary staff caring for sufferers undergoing advanced hepatopancreatobiliary procedures and their experience within the minimally invasive treatment of anastomotic leaks, intraabdominal abscesses, and postoperative bleeding is liable for considerably improved affected person outcomes (Mezhir, 2013; Sohn, 2003). This article will provide an summary of probably the most generally reported postoperative complications associated with main pancreatic and hepatic resections, together with a review of the current definitions and grading systems used for reporting. It will then provide an in depth dialogue of the appropriate management of each complication based on probably the most current literature and with an emphasis on interventional strategies. The reported morbidity and mortality following pancreatic resection in several massive sequence reported since 2000 is offered in Table 27. Pancreatic resection is related to a number of problems, lots of that are process specific and occur at the operative website (hemorrhage, leak, obstruction), whereas others occur remotely as a consequence of major surgical procedure rather than the precise sort of surgery (deep venous thrombosis, cardiac arrhythmia, pneumonia). This article is primarily concerned with the most common extreme complications directly related to the technical features of the operation itself. The reported frequencies of those issues are listed in the reported frequencies for these issues in a quantity of large series since 2000 are presented in Table 27. Defining and Grading Complications After Pancreatectomy Postoperative problems are notoriously tough to research because of the inconsistent definitions and imprecise terminology used to designate them (see Chapter 66). They comprise three overlapping manifestations of the identical underlying problem, which is breakdown and leakage at the pancreatic anastomosis (or pancreatic closure web site for distal and central pancreatectomies). For instance, an intraabdominal fluid assortment requiring drain placement could moderately be reported as an abscess. If the drainage was studied and found to be amylase wealthy, it could be considered a leak. If drainage from the leak continued during a period of time, it is also thought of a fistula. However, the absence of any standardized, quantifiable measures for reliably differentiating these from one another meant that the same complication could presumably be reported in three different ways. They generated 4 consensus definitions consultant of those mostly used in the literature and utilized each to the identical management group of pancreatectomies. Using these 4 definitions, the incidence of pancreatic fistulae various within the same group of patients from 10% to 29%. This lack of consistency is mirrored in the literature, the place the precise reported incidence of pancreatic fistulae varies similarly from 2% to 29% (Braga et al, 2011; B�chler et al, 2000; Muscari et al, 2006; Reid-Lombardo et al, 2007).
Buy biltricide once a dayThe inflated balloon is maintained till the "waist" corresponding with the biliary sphincter disappears, normally for 15 to 30 seconds. The primary advantage of sphincteroplasty is that it leads to transient widening of the biliary sphincter such that the biliary sphincter will stay intact and functional postprocedure. This may be advantageous in children, as an intact biliary sphincter will presumably decrease the chance of recurrent choledocholithiasis. The primary drawback of performing sphincteroplasty alone is its affiliation with a higher danger of pancreatitis and lower charges of stone clearance in contrast with sphincterotomy (Baron & Harewood, 2004; DiSario et al, 2004). Furthermore, balloon sphinctero plasty following sphincterotomy has been proven to be protected, with comparable complication rates compared with sphincterotomy alone (Maydeo & Bhandari, 2007; Weinberg et al, 2006). Transpancreatic Precut Sphincterotomy (Goff Technique) Transpancreatic precut (transeptal) sphincterotomy for biliary entry was first described by Goff et al (1995). In this technique, following selective cannulation of the pancreatic duct, precut sphincterotomy is carried out by cutting the septum between the pancreatic and bile duct with the standard sphincterotome directed cephalad towards the bile duct. Additional superior tech niques for biliary access, together with those in patients with surgi cally altered anatomy, will be coated later on this chapter. Choledocholithiasis is concomitantly current in up to 20% of patients with cholelithiasis at the time of cholecystectomy (Menezes et al, 2000). The fundamental technique of sphincterotomy has not changed significantly since its preliminary description. The commonplace sphincterotome, the Erlangen "pulltype" mannequin, consists of a catheter containing an electrosurgical cutting wire exposed 20 to 25 mm near the tip of the sphincterotome. Once deep biliary can nulation has been achieved, the sphincterotome is retracted slowly, until one fourth to one half of the wire length is uncovered outside the papilla. The sphincterotome is barely bowed in order that the slicing wire is in contact with the roof of the papilla. A, Cholangiogram showing diffusely dilated biliary system with stone in the commonbileduct(arrow). The extraction balloon is inflated (to the diameter of the bile duct) above the stone and pulled back gently to the level of the papilla. In the setting of multiple stones, it may be very important remove the stones individually starting with probably the most distal one, to avoid stone impaction. Similarly, there are additionally a big selection of wire baskets in different sizes and configurations. The stone is entrapped between the wires when the basket is closed, and subsequent removal is achieved by traction removing of the basket in the axis of the bile duct. Conversely, the extraction balloon may be more suitable for the removing of small stones/fragments which are tough to entrap between the wires or when opening of the basket is constrained by duct caliber. Lithotripsy Standard stone extraction techniques could fail when a stone is massive, impacted, proximal to a stricture, or when stones are a quantity of. A number of modalities are presently out there to fragment these tough stones earlier than extraction, including mechanical lithotripsy, endoscopic intraductal lithotripsy, and extracorporeal shockwave lithotripsy. Mechanical Lithotripsy Mechanical lithotripsy has been probably the most regularly used litho tripsy method, given its ease of use and availability, with success rates of 90% and better (Chang et al, 2005; Stefanidis et al, 2011). There are two variations to the technique of mechanical lithotripsy: an externaltype lithotriptor methodology and an integrated throughtheendoscope method. Using the externaltype lithotriptor, the stone is captured inside a standard Dormia basket, the basket handle is cut off, and the endoscope is eliminated. A coiled metallic sheath is inserted over the wire until its tip is in touch with the stone, and mechanical lithotripsy is performed by turning the crank handle, crushing the stone between the basket wires and the steel tip of the sheath. Once the stone is captured within the basket, forceful traction on the wires towards the metallic sheath results in stone fragmentation. The most common causes for failure embody giant stones exceeding 2 cm in measurement and stone impaction. Basket impaction throughout the duct or rupture of the traction wires has been reported in up to 4% of the instances, which may require external salvage lithotriptor or surgical retrieval of the retained basket and stone (Garg et al, 2004). The goal is to relieve the biliary obstruction that can probably result in complications, similar to jaundice, pruritus, cholangitis, continual liver disease, and liver failure. Biliary stricture characterization could be a diagnostic chal lenge that requires a multidisciplinary method with the inte gration of laboratory testing, noninvasive and invasive imaging, and tissue sampling strategies. This part focuses on the tech nical elements and outcomes associated with endoscopic man agement of benign and malignant biliary strictures. Advances in endoscopic imaging and tissue sampling for the prognosis of biliary strictures might be coated later in this chapter.
Purchase 600mg biltricide fast deliveryAlthough closure over a T-tube is usually the popular strategy, a recent evaluation suggested that the duct could be closed primarily with out increased morbidity or mortality (Gurusamy et al, 2013). If a T-tube is used, dimension 14 Fr or bigger will permit cholangiography and choledochoscopy. These embody identification of a wholesome phase of bile duct tissue proximal to the positioning of obstruction; preparation of a phase of alimentary tract such as duodenum or, more generally, Roux-en-Y jejunal limb; and construction of a mucosa-to-mucosa anastomosis. It is due to this fact essential to use preoperative imaging to clearly delineate the biliary anatomy previous to endeavor operative intervention for biliary decompression. Cross-sectional imaging with magnetic resonance imaging/magnetic resonance cholangiopancreatography, and even thin-cut computed tomography scans, can accurately characterize the anatomy of the biliary tree and underlying pathology (see Chapter 19). Invasive imaging of the biliary tree with endoscopic or percutaneous cholangiography permits stent placement, which might facilitate intraoperative identification of right and left hepatic ducts (see Chapters 20, 29, and 30). It can be essential to recognize that instrumentation of the biliary tree introduces bacterial contamination that, in a setting of biliary stasis, can end result in cholangitis, periductal inflammation, and a better threat of postoperative infections. Caution must even be exercised to keep away from percutaneous drainage whether it is unlikely that the stent may be passed throughout the obstructing lesion. These complexities underscore the important importance of an skilled multidisciplinary staff reviewing and treating advanced biliary obstruction, significantly at the biliary confluence. Depending on the underlying pathology, there are a selection of options for restoration of biliary continuity with the alimentary tract. For occasion, choledocholithiasis refractory to native exploration may require choledochoduodenostomy. Other benign etiologies, such as iatrogenic bile duct injury, strictures from previous biliary-enteric operations, choledochal cysts, or inflammatory strictures, may require restoration with Roux-en-Y choledochojejunostomy or hepaticojejunostomy. Additionally, benign proximal biliary strictures in addition to malignancy (cholangiocarcinoma) could require anastomosis between intrahepatic ducts and jejunum. Finally, the gallbladder can also be utilized to facilitate drainage (cholecystoduodenostomy and cholecystojejunostomy). Although nonoperative measures can be utilized in most situations, familiarity with the assorted surgical strategies can allow appropriate restoration of biliary-enteric continuity when the scenario demands (see Chapter 42). Caution have to be exercised within the setting of long-standing biliary obstruction or circumstances related to ipsilateral hepatic atrophy and contralateral hypertrophy. In the situation of marked proper hemiliver atrophy, the liver hilum and portal constructions will turn into rotated in a counterclockwise method. In cases of very profound proper liver atrophy, access to the biliary confluence might require a thoracoabdominal incision. Hepaticojejunostomy Despite the necessity for a further anastomosis (at the jejunojejunostomy), Roux-en-Y hepaticojejunostomy is the most common surgical reconstruction for biliary obstruction. The jejunum is usually anastomosed to the widespread hepatic duct just distal to the confluence of the best and left hepatic ducts. Disadvantages include necessity for two anastomoses and exclusion of bile from the duodenum. Access to the best portal pedicle containing the proper hepatic duct may be achieved by isolating the pedicle in an extrahepatic location or by exposing the pedicle via intrahepatic dissection. By continuing this airplane of dissection to the best (onto the cystic plate), the best hepatic duct may be exposed (Strasberg et al, 2008). If the extrahepatic portion of the right hepatic duct is simply too short to be visualized on this way (as is usually the case), the intrahepatic approach could additionally be used. This requires hepatotomies within the caudate process just posterior to the porta hepatis and alongside the bottom of the gallbladder fossa. Incision and Exposure A right subcostal incision with or with out an higher midline extension or a left subcostal extension followed by upward elevation and cephalad retraction of the costal margin provides sufficient publicity for construction of any biliary-enteric anastomosis. The ligamentum teres is ligated and divided, and the falciform ligament is split to its most cephalad extent on the diaphragm. If direct decompression of the gallbladder is not to be undertaken, cholecystectomy may be advantageous for identification of the cystic duct, which could be dissected to its point of insertion onto the common hepatic duct. Cholecystectomy will also expose the cystic plate, which runs in continuity with the hilar plate. Because of its longer extrahepatic course, the left hepatic duct is the preferred goal. After ligation of the ligamentum teres with a agency tie, retraction is utilized to elevate the left hemiliver.
Buck Qi (Astragalus). Biltricide. - What is Astragalus?
- Common cold; chest pain; diabetes; chronic fatigue syndrome (CFS); hepatitis; HIV/AIDS; fibromyalgia; and cancer including breast cancer, lung cancer, and cervical cancer.
- Dosing considerations for Astragalus.
- Are there safety concerns?
- How does Astragalus work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96925
Effective biltricide 600mgBirlouez-Aragon I, et al: Antioxidant nutritional vitamins and degenerative pathologies: a review of vitamin C, J Nutr Health Aging 7:103�109, 2003. Braga M, et al: Oral preoperative antioxidants in pancreatic surgery: a double-blind, randomized, scientific trial, Nutrition 28:160�164, 2012. Braga M, et al: Enhanced restoration after surgery pathway in patients present process pancreaticoduodenectomy, World J Surg 38:2960�2966, 2014. Brennan M, et al: A potential randomized trial of complete parenteral nutrition after major pancreatic resection for malignancy, Ann Surg 220:436�444, 1994. Bruera E, et al: Cachexia and asthenia in most cancers patients, Lancet Oncol 1:138�147, 2000. Bruix J, Sherman M; American Association for the Study of Liver Diseases: Management of hepatocellular carcinoma: an update, Hepatology 53(3):1020�1022, 2011. Bulger E, et al: Enteral vitamin E supplementation inhibits the cytokine response to endotoxin, Arch Surg 132:1337�1341, 1997. Bulger E, Helton W: Nutrient antioxidants in gastrointestinal disease, Gastroenterol Clin North Am 27:403�419, 1998. Burra P, et al: Hepatic malondialdehyde and glutathione in finish stage persistent liver illness [abstract], Hepatology 16(4 Pt 2):266, 1992. Buzby G, et al: Prognostic nutritional index in gastrointestinal surgery, Am J Surg 139:160�167, 1988. Cabr� E, et al: Effect of total enteral diet on the short-term end result of severely malnourished cirrhotics, Gastroenterology ninety eight:715�720, 1990. Cerwenka H, et al: Normothermic liver ischemia and antioxidant remedy during hepatic resections, Free Radic Res 30:463�469, 1999. Cho M, et al: Vitamin D deficiency and prognostics among patients with pancreatic adenocarcinoma, J Transl Med 11:206, 2013. Clugston A, et al: Nutritional threat index predicts a high-risk population in patients with obstructive jaundice, Clin Nutr 25(6):949�954, 2006. Cohendy R, et al: Preoperative dietary evaluation of aged sufferers: the Mini Nutritional Assessment as a sensible software, Clin Nutr 18(6):345�348, 1999. Curran R, et al: Multiple cytokines are required to induce hepatocyte nitric oxide production and inhibit protein synthesis, Ann Surg 212:460�471, 1990. Cywes R, et al: Effect of intraportal glucose infusion on hepatic glycogen content material and degradation and consequence of liver transplantation, Ann Surg 216:235�247, 1992. Dolais-Kitabgi J, et al: Effect of insulin and glucagon on amino acid transport in isolated hepatocytes after partial hepatectomy within the rat, Endocrinology 109:868�875, 1981. Eigler N, et al: Synergistic interactions of physiologic increments of glucagon, epinephrine and cortisol in the canine: a mannequin for stressinduced hyperglycemia, J Clin Invest sixty three:114�123, 1979. Fan S, et al: Perioperative nutritional assist in patients undergoing hepatectomy for hepatocellular carcinoma, N Engl J Med 331:1547� 1552, 1994. Fong Y, et al: Total parenteral nutrition and bowel rest modify the metabolic response to endotoxin in people, Ann Surg 210:449�457, 1989. Foschi D, et al: Hyperalimentation of jaundiced patients on percutaneous transhepatic biliary drainage, Br J Surg 73(9):716�719, 1986. Fowler F, et al: Characterization of sodium-dependent amino acid transport exercise throughout liver regeneration, Hepatology sixteen:1187� 1194, 1992. Fride E, et al: Endocannabinoids and meals intake: newborn suckling and urge for food regulation in adulthood, Exp Biol Med (Maywood) 230(4):225�234, 2005. Fukushima R, Yamazaki E: Vitamin C requirement in surgical sufferers, Curr Opin Clin Nutr Metab Care 13(6):669�676, 2010. Fusai G, et al: Incidence and risk components for the event of extended and severe intrahepatic cholestasis after liver transplantation, Liver Transpl 12(11):1626�1633, 2006. Gianotti L, et al: Artificial vitamin after pancreaticoduodenectomy, Pancreas 21:344�351, 2000. Glen P, et al: Evaluation of an inflammation-based prognostic rating in patients with inoperable pancreatic most cancers, Pancreatology 6(5):450� 453, 2006. Goode J, et al: Reperfusion damage, antioxidants and hemodynamics during orthotopic liver transplantation, Hepatology 19:354�359, 1994. Gunsar F, et al: Nutritional standing and prognosis in cirrhotic sufferers, Aliment Pharmacol Ther 24(4):563�572, 2006.
Trusted biltricide 600 mgEither focal fatty sparing or fatty substitute of the pancreas can seem masslike, in addition to focal pancreatitis, such as groove pancreatitis. Additional pitfalls include congenital contour abnormalities, complicated pseudocysts, and lipomas which will mimic pancreatic masses. Cystic Neoplasms of the Pancreas Cystic pancreatic neoplasms (see Chapter 60) fall into two major classes: serous and mucinous cystic neoplasms. Differentiation could also be made on imaging research primarily based on the inner architecture and size of the cysts. Serous cystadenomas are generally benign neoplasms with well-circumscribed lobulated borders. Chapter 15 Ultrasound of the liver, biliary tract, and pancreas 275 from 1 to 20 mm in size. Serous tumors composed of comparatively larger cysts will seem as partially strong plenty with peripheral cystic areas on sonography. A central stellate scar is a characteristic characteristic of many serous cystadenomas and could also be visible as an echogenic or calcified focus with shadowing (Hutchins & Draganov, 2009; Yeh et al, 2001). Mucinous cystic neoplasms often seem as unilocular or multilocular cystic lesions, with thick septations and thick partitions, and are usually situated in the pancreatic body and tail. Mucinous cystic neoplasms have malignant potential, and a strong mural nodule is suspicious for malignancy. Endoscopic ultrasound is useful in analysis of cystic pancreatic neoplasms because of higher demonstration of inside cyst structure and potential for fluid aspiration (see Chapter 16). In particular, the gallbladder and biliary tree have inherently wonderful contrast decision because of their cystic nature relative to adjoining stable organs. Doppler ultrasound is an important and useful element of the hepatic vascular evaluation. Abdominal sonography is usually used as an initial examination to decide the positioning of abnormality and might typically present a prognosis or a short differential prognosis. Albrecht T, et al: Guidelines for using distinction brokers in ultrasound, Ultraschall Med 25(4):249�256, 2004. Araki J, et al: Natural course of autoimmune pancreatitis without steroid remedy exhibiting hypoechoic lots within the uncinate process and tail of the pancreas on ultrasonography, J Ultrasound Med 25(8):1063�1067, 2006. Ardelean M, et al: Contrast enhanced ultrasound in the pathology of the pancreas-a monocentric expertise, Med Ultrason 16(4):325� 331, 2014. Arena U, et al: Acute viral hepatitis increases liver stiffness values measured by transient elastography, Hepatology 47(2):380�384, 2008. Bartolozzi C, et al: Differentiation of hepatocellular adenoma and focal nodular hyperplasia of the liver: comparability of energy Doppler imaging and conventional shade Doppler sonography, Eur Radiol 7(9):1410�1415, 1997. Bekker J, et al: Early hepatic artery thrombosis after liver transplantation: a scientific review of the incidence, consequence and risk elements, Am J Transplant 9(4):746�757, 2009. Bolondi L, et al: Sonography of continual pancreatitis, Radiol Clin North Am 27(4):815�833, 1989. Bolondi L: Screening for hepatocellular carcinoma in cirrhosis, J Hepat 39(6):1076�1084, 2003. Brancatelli G, et al: Benign regenerative nodules in Budd-Chiari syndrome and other vascular issues of the liver: radiologic-pathologic and medical correlation, Radiographics 22(4):847�862, 2002. Caturelli E, et al: Hemangioma-like lesions in continual liver illness: diagnostic analysis in patients, Radiology 220(2):337�342, 2001. Coco B, et al: Transient elastography: a brand new surrogate marker of liver fibrosis influenced by major changes of transaminases, J Viral Hepat 14(5):360�369, 2007. Cura M, et al: Diagnostic and interventional radiology for Budd-Chiari syndrome, Radiographics 29(3):669�681, 2009. Ding H, et al: Imaging of focal liver lesions: low-mechanical-index real-time ultrasonography with SonoVue, J Ultrasound Med 24(3): 285�297, 2005. Ferraioli G, et al: Shear wave elastography for analysis of liver fibrosis, J Ultrasound Med 33(2):197�203, 2014. Ghittoni G, et al: Intrabile duct metastasis from colonic adenocarcinoma with out liver parenchyma involvement: distinction enhanced ultrasonography detection, Abdom Imaging 35(3):346�348, 2010. Goyal N, et al: Non-invasive evaluation of liver cirrhosis utilizing ultrasound, Clin Radiol 64(11):1056�1066, 2009. Grazioli L, et al: Hepatic adenomas: imaging and pathologic findings, Radiographics 21(4):877�892, dialogue 892-874, 2001.
Order 600mg biltricide otcThe combination of decreased or absent bile in the intestine and impaired cellular immunity and reticuloendothelial cell perform appears to be a major factor contributing to more frequent infective issues within the jaundiced affected person. Acute cholangitis is a bacterial an infection of the biliary ductal system, and it varies in severity from mild and self-limited to severe and life threatening (see Chapter 43). The scientific triad related to cholangitis-fever, jaundice, and pain-was first described in 1877 by Charcot. Cholangitis outcomes from a combination of two components: significant bacterial concentrations within the bile and biliary obstruction. Although bile from the gallbladder and bile ducts is normally sterile, in the presence of frequent bile duct stones or different obstructing pathology, the incidence of positive cultures will increase; likewise, instrumentation of the biliary tree additionally tremendously increases charges of bile colonization. The most typical organisms recovered from the bile in sufferers with cholangitis embody Escherichia coli, Klebsiella pneumonia, the enterococci, and Bacteroides fragilis (Thompson et al, 1990a). In the presence of bacteribilia and normal biliary pressures, hepatic venous blood and perihepatic lymph are sterile. However, with partial or complete biliary obstruction, intrabiliary pressures rise to 20 to 30 cm H2O, and organisms rapidly appear in both the blood and lymph. The fever and chills associated with cholangitis are the result of systemic bacteremia attributable to cholangiovenous and cholangiolymphatic reflux. The most typical causes of biliary obstruction are choledocholithiasis (see Chapter 36), benign strictures (see Chapter 42), biliary-enteric anastomotic strictures (see Chapters 31), and periampullary or proximal biliary cancers (see Chapters 49 to fifty one and 59). Before 1980, choledocholithiasis was the purpose for approximately 80% of the reported circumstances of cholangitis. In latest years, however, malignant strictures have turn out to be a frequent cause, especially after the location of biliary stents. Endoscopic cholangiography, percutaneous transhepatic cholangiography, and stent placement by way of both the endoscopic or percutaneous route are all identified to cause bacteremia, and these procedures are frequently performed in sufferers with a presumptive analysis of malignant obstruction. The sufferers with jaundice had only 11% of the pores and skin propylhydroxylase activity of the controls. In the subgroup of sufferers with jaundice secondary to malignancy, propylhydroxylase exercise was lower than 7% of controls. Interestingly, in patients with jaundice secondary to benign obstruction, the exercise elevated to one hundred pc of controls. Other Factors Other issues that face sufferers with jaundice are anorexia, weight reduction, and malnutrition. Appetite is adversely influenced by the dearth of bile salts within the intestinal tract. In addition, patients with pancreatic or periampullary malignant lesions might have partial duodenal obstruction or irregular gastric emptying, in some instances secondary to tumor infiltration of the celiac nerve plexus. Patients with pancreatic or ampullary tumors also could have pancreatic endocrine and exocrine insufficiency. This latter downside might additional compound other dietary defects that, in flip, might exacerbate the immune deficits of the affected person with jaundice. Several recent observations suggest that the various physiologic derangements induced by obstructive jaundice take a very lengthy time to reverse. This similar extended effect of obstructive jaundice has been famous with lymphocyte, polymorphonuclear, and Kupffer cell function. Moreover, a latest evaluation by Strasberg and colleagues (2014) means that preoperative jaundice could adversely have an effect on long-term survival in sufferers with resected pancreatic most cancers. Management Historically, the one option for the reduction of obstructive jaundice was operative intervention; however, with the development of therapeutic strategies corresponding to percutaneous (see Chapters 30 and 52) and endoscopic stenting (see Chapter 29), balloon dilation, and endoscopic sphincterotomy, many nonoperative choices for the relief of obstructive jaundice are now available. The surgeon must decide the most secure and best therapy for every particular person patient and must adequately prepare every affected person for surgical procedure or nonoperative therapeutic intervention. Patients with obstructive jaundice and those with hepatocellular disease extreme sufficient to trigger jaundice are vulnerable to many secondary issues. Patients with jaundice are at elevated risk for the development of kidney injury, gastrointestinal bleeding, infections, and wound problems (see earlier part on Pathophysiology). Cardiac, pulmonary, and renal function must be considered in every affected person present process major stomach surgical procedure. Complications related to portal hypertension, such as ascites, varices, and encephalopathy, may develop in patients with continual liver illness and cirrhosis, and these Wound Healing Delayed wound healing and a excessive incidence of wound dehiscence and incisional hernia have been observed in sufferers with jaundice undergoing surgery.
Biltricide 600mg fast deliveryAmouyal P, et al: Diagnosis of choledocholithiasis by endoscopic ultrasonography, Gastroenterology 106:1062�1067, 1994. Christoforidis E, et al: Endoscopic administration of retained bile stones with an indwelling T-tube, Surg Endosc 18:1582�1586, 2004. Collins C, et al: A potential study of widespread bile duct calculi in sufferers undergoing laparoscopic cholecystectomy: pure historical past of choledocholithiasis revisited, Ann Surg 239:28�33, 2004. Demartines N, et al: Evaluation of magnetic resonance cholangiography in the management of bile duct stones, Arch Surg 135:148�152, 2000. DenBesten L, Berci G: the current status of biliary tract surgery: a world examine of 1072 consecutive sufferers, World J Surg 10: 116�122, 1986. Escourrou J, et al: Early and late issues after endoscopic sphincterotomy for biliary lithiasis with and without the gallbladder in situ, Gut 25:598�602, 1984. Fogli L, et al: Laparoscopic cholecystectomy without intraoperative cholangiography: audit of long-term outcomes, J Laparoendosc Adv Surg Tech A 19:191�193, 2009. Garrow D, et al: Endoscopic ultrasound: a meta-analysis of check performance in suspected biliary obstruction, Clin Gastroenterol Hepatol 5:616�623, 2007. Kondo S, et al: Detection of widespread bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography, Eur J Radiol 54:271�275, 2005. Orloff M: Importance of surgical approach in prevention of retained and recurrent bile duct stones, World J Surg 2:403�410, 1978. Polkowski M, et al: Helical computed tomographic cholangiography versus endosonography for suspected bile duct stones: a potential blinded study in non-jaundiced patients, Gut forty five:744�749, 1999. Ramirez P, et al: Choledochoduodenostomy and sphincterotomy within the treatment of choledocholithiasis, Br J Surg 81:121�123, 1994. Seifert E, et al: Lanseitresulate nach endoskipischer Sphinkterotomie, Dtsch Med Wochenschr 107:610�614, 1982. Sgourakis G, et al: Predictors of frequent bile duct lithiasis in laparoscopic period, World J Gastroenterol 11:3267�3272, 2005. Shanmugam V, et al: Is magnetic resonance cholangiopancreatography the new gold standard in biliary imaging Speranza V, et al: Transduodenal papillostomy as a routine procedure in managing choledocholithiasis, Arch Surg 117:875�878, 1982. Sugiyama M, Atomi Y: Endoscopic ultrasonography for diagnosing choledocholithiasis: a potential comparative study with ultrasonography and computed tomography, Gastrointest Endosc 45:143� 146, 1997. Topal B, et al: the worth of magnetic resonance cholangiopancreatography in predicting common bile duct stones in patients with gallstone illness, Br J Surg ninety:42�47, 2003. Trondsen E, et al: Prediction of frequent bile duct stones previous to cholecystectomy. A potential validation of a discriminant evaluation operate, Arch Surg 133:162�166, 1998. The majority of cases of choledocholithiasis are secondary, the result of stones that initially formed in the gallbladder. Choledocholithiasis can lead to a big selection of scientific manifestations, together with biliary colic, obstructive jaundice, ascending cholangitis (see Chapter 43), and pancreatitis (see Chapters fifty four and 55). These scientific scenarios can differ significantly in presentation and morbidity, starting from minimal to important illness and demise. If left untreated, continual choledocholithiasis can even cause inflammatory strictures, recurrent infections, or cirrhosis. The management of choledocholithiasis has changed radically over the last several decades. It was not until the introduction of the laparoscopic cholecystectomy in the late 1980s that the function for an related less invasive methodology of treating choledocholithiasis turned a priority. In addition, the aptitude and experience of the out there personnel will have an result on the treatment algorithm. The commonest clinical scenarios encountered by surgeons embrace identified or suspected stones prior to cholecystectomy, the prognosis of stones intraoperatively, and stones recognized subsequent to cholecystectomy. In most patients, our most popular technique is laparoscopic cholecystectomy with selective intraoperative cholangiogram (see Chapter 23).
|