|
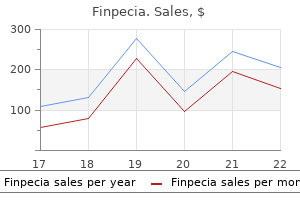
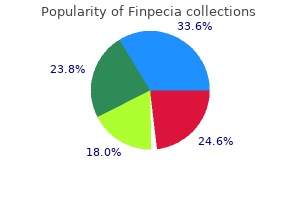
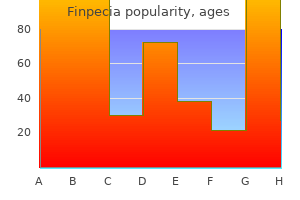
Finpecia dosages: 1 mg
Finpecia packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Cheap 1mg finpecia with amexA direct midline posterior skin incision along the spine is made, extending from L4 to S2. The fascia is incised along with the skin incision, and the paraspinal muscles are dissected off of the posterior components subperiosteally. The anesthetic and spinal monitoring group is knowledgeable before any corrective maneuvers are performed. Once the entire pedicle screws have been positioned, a mild reduction is performed, geared toward correcting the slip angle. Using reduction instruments connected to the pedicle screws, a dorsal extension pressure is applied to the lumbar backbone whereas a counterforce is applied to the sacrum. Attention to spinal twine monitoring is essential at this level in the operation to keep away from undue neurologic damage. Following correction of the slip angle, gradual correction of the slip is performed by applying stress on the sacrum whereas the lumbar spine is held and a delicate force is utilized in the different way, affording discount. The entire construct is checked after discount underneath fluoroscopy to ensure correct implant placement and enough correction of the spondylolisthesis, and last tightening is completed. The dura is gently retracted, and a cage is positioned to add anterior column support. Alternatively, fibular strut grafting could additionally be used to provide anterior column support. A cut up fibular graft is fashioned and countersunk into each drill hole bilaterally. The reduction is performed slowly and maintained over time to allow for stretch of the soft tissue. Reduction of the slip angle is much more important than reduction of the slip itself. Close consideration to spinal cord monitoring is crucial during the entire reduction maneuver. The rods are templated, reduce, and contoured, after which connected to the construct whereas reduction is maintained. The L5�S1 disc is identified and eliminated, a fusion is carried out, and the L5�S1 disc house is crammed with cancellous autograft or allograft. As another, a double cut up fibular strut graft (modified Bohlman technique) could be inserted from the sacrum to the body of L5 to add anterior column assist. The process is completed by inserting bone graft lateral to the implants alongside the transverse processes from L4 to the sacrum. Meticulous hemostasis is carried out, and a layer-by-layer closure of the operative web site is carried out. All needed and appropriate imaging studies must be evaluated rigorously to identify all aspects of the deformity-including the degree of the deformity and the sort (eg, isthmic vs congenital)-as nicely as another spinal deformity that may be present (eg, spina bifida occulta). Care should be taken, especially when pathologies corresponding to spina bifida occulta are present, to forestall iatrogenic neurologic damage. Decompression of at-risk nerve roots is a key component to exposure and operation. Instrumentation Careful preparation should be undertaken before performing instrumentation and discount. Adequate decompression of all neurologic constructions in danger should be ensured to forestall iatrogenic injury. Close attention have to be paid to neurophysiologic monitoring during both instrumentation and reduction. This procedure ought to be done over time to permit for leisure of the soft tissue structures. Reduction of the slip angle is more necessary than complete discount of the slip. In the instant postoperative interval, the hips and knees are flexed and elevated using pillows to alleviate pain. Postoperative anteroposterior and lateral standing backbone radiographs are taken before discharge. Activity restriction (ie, avoidance of bending and rotational motion) is carried out till fusion has occurred.
Purchase finpecia torontoSpondylolisthesis has been grouped into five differing types under the Wiltse-Newman classification: dysplastic, isthmic, degenerative, traumatic, and pathologic. This increase is believed to be related to the calls for of elevated stress and weight bearing positioned on the lumbosacral spine. The lumbar vertebrae are widest in transverse diameter than in the anterior-posterior aircraft. The aspect joints of the lumbar backbone are oriented more toward the sagittal aircraft, allowing for more flexion and extension motion. The neurovascular buildings in the lumbar spine run a similar course when in comparability with the thoracic backbone. The segmental vasculature arises instantly from the aorta and run dorsally across the lateral facet of each vertebral physique. These vessels run between the transverse processes, the place they may be prone to harm in additional lateral exposures. The conus medullaris extends from probably the most distal portion and goes on to innervate the bowel and bladder. Beneath the conus, the lumbar and sacral nerve roots are organized to kind the cauda equina. Each of those roots exits segmentally beneath the pedicle of the corresponding vertebrae. The pedicles are cylindrical structures that bridge the posterior components of the backbone with the vertebral body. The peak and diameter of the pedicles increases from the thoracic to the lumbar backbone. The transverse angulation of the pedicles is directed medially, increasing progressively from L1 to L5. Corresponding nerve roots are discovered each superior and inferior to every pedicle, with the inferior nerve root in closer proximity to the pedicle. In the higher a half of the lumbar spine, the orientation of the joints allows for multidirectional stabilization. This is in distinction to the lumbosacral side joint, which is flat and extra coronally oriented and acts to resist shearing forces through the joint. In a comparability of the development of the slip between isthmic and dysplastic types of spondylolisthesis, dysplastic sorts showed elevated progression. Abnormal gait exemplified by a hip-flexed, knee-flexed gait sample may be current. Hamstring tightness, which also may be current, is examined by measuring the popliteal angle. Many sufferers with high-grade slips will tend to develop tight hamstrings owing to the event of abnormal biomechanics in the lumbar backbone. Straight leg increase should be done to check for nerve root compression or hamstring tightness. A positive examination with radicular ache denotes either an L5 or S1 nerve root compression. Radicular pain elicited earlier than 70 degrees is indicative of root compression, whereas that elicited above 70 levels would possibly denote extraspinal compression of the sciatic nerve. A rectal examination ought to be done in the presence of bladder and bowel dysfunction. If the ache is exacerbated, that finding helps the analysis of a nerve root compression. The "bony hook," consisting of the pedicle, the pars interarticularis, and the inferior aspects, offers stability by resisting these shear forces and preventing ahead slippage or sliding over the inferior endplates. In the setting of congenital or dysplastic spondylolisthesis, the backbone begins to slip even when the posterior elements are intact. In the isthmic kind of spondylolisthesis, secondary to a pars defect, the high shear and compressive forces occurring via the lumbar spine and lumbosacral joint are less well resisted. This is due to the loss of posterior restraint, permitting forward displacement of 1 vertebral segment over the following more caudal degree. Beutler et al,1 in a 45-year follow-up examine of 30 sufferers recognized with spondylolysis, screened in the Nineteen Fifties from a pool of 500 first-grade kids, confirmed that no sufferers with unilateral pars defects developed spondylolisthesis. They also showed that instances with bilateral pars defects and low-grade slips follow a course much like that seen within the basic populace.
Finpecia 1mg discountRefracture is common however manageable with cast immobilization if deformity is minimal. In the presence of recurrent deformity, revision surgery using a larger-diameter, longer rod, bone graft, and osteotomy, if needed, is beneficial. Use of an intramedullary rod for the remedy of congenital pseudarthrosis of the tibia. Use of an intramedullary rod for remedy of congenital pseudarthrosis of the tibia: a long-term follow-up study. Use of an intramedullary rod for the remedy of congenital pseudarthrosis of the tibia: surgical method. Congenital pseudarthrosis of the tibia: outcomes of technical variations in the Charnley-Williams procedure. Once the ankle is no longer transfixed, an ankle rehabilitation program is implemented that includes vary of motion and calf strengthening. Once skeletal maturity is reached, the orthotic use is beneficial for sports activities and high-stress actions. Both studies emphasised the significance of listening to particulars relating to the technique of rod insertion, continued orthotic use, and long-term follow-up care. In the Ilizarov methodology, lengthening is completed by gradual bone distraction via a low-energy, atraumatic corticotomy web site. The bone fragments are controlled by way of secure bone fixation utilizing half-pins and tensioned wires via bone which are rigidly fixed to an external ring fixator or arch. The most commonly lengthened bones within the lower extremity embody the tibia and fibula, the femur, and the metatarsal. In the higher extremity, essentially the most generally lengthened bones are the humerus, the radius and ulna, and the metacarpal bones. Consideration is given to lengthening of the surrounding soft tissues, which include the muscle tendon unit, neurovascular bundle, and skin. Tibial lengthening could cause knee or ankle subluxation and progressive equinus deformity of the foot. Metatarsal and metacarpal lengthening may cause metatarsoor metacarpophalangeal subluxation. The new bone is formed largely by intramembranous ossification and, to a lesser extent, through endochondral ossification. Distraction is an efficient device for influencing reparative regeneration of both the bone and the delicate tissue ("stretching rigidity," as described by Ilizarov). Gradually eradicating distraction and applying delicate compression will increase the speed of transforming. To stop any shortening of the section from compression, preliminary over-distraction of up to zero. Functional load is a powerful stimulus for the advance of blood flow and allows organic transforming of the regenerated osseous part. The extent of load is dependent upon the steadiness of fragments and the amount of regenerate. Infection: Physeal destruction might outcome from physeal invasion from adjacent metaphyseal or epiphyseal bacterial osteomyelitis, or direct physeal involvement within the case of intracapsular joint physes such as on the hip and shoulder. Paralysis: Poliomyelitis and cerebral palsy as properly as other nervous system afflictions in children usually result in shortening on the more affected side. In traditional hemihypertrophy, upper extremity hypertrophy in addition to hemifacial asymmetry may be current. Vascular overgrowth syndromes could also be associated with cutaneous or deep hemangiomas, which may alter surgical approaches to tried limb equalization. Discrepancies as small as 2 cm are precisely detected by this method, and detection of discrepancies is essentially unaffected by affected person dimension or body mass. Direct measurement of leg length from anterosuperior iliac backbone to the tip of medial or lateral malleolus is considerably much less accurate. Apparent leg length is measured with the affected person supine with the legs parallel to one another. True leg length is measured from the anterior superior iliac backbone to the tip of the medial malleolus. It is important to place the legs in identical positions to measure true leg length. If the affected person has a 20-degree abduction deformity of proper hip, the left hip is placed in 20 levels of abduction to measure true size.
Buy finpecia amexNext, utilizing a blunt pin or straight instrument, mark on the skin the desired strategy trajectory to the physeal bar. Exsanguinate the limb and incise the skin longitudinally where an internervous plane can be utilized. Remove and save the cortical window and superficial metaphyseal bone to be used for later closure. As the tip of the reference Kirschner wire is approached, use a motorized burr to carefully remove bone until the middle of the physeal bar is reached, as confirmed fluoroscopically. Before making a skin incision, fluoroscopy is introduced into the surgical field and the surgeon draws on the pores and skin the physis location, the physeal bar location, the surgical method trajectory, and the pores and skin incision location that can permit the specified strategy. Under fluoroscopic steering a Kirschner wire is superior to the level of the physeal bar along the desired surgical approach trajectory. Multiple drill holes are then made that incorporate the Kirschner wire into the periphery of an elliptical cortical window. The Kirschner wire will act as a information to the situation and depth of the physeal bar. Multiple drill holes are connected with a narrow osteotome to create a cortical window. After removing metaphyseal bone with a curette, a burr is guided by fluoroscopy to expand the bar resection cavity until regular physis is visualized throughout the cavity. A surgical headlight is helpful to visualize the physis throughout the resection cavity. Topical liquid thrombin may be applied to the resection cavity bone surface to scale back hematoma formation, which in concept might promote recurrent bar formation. Within the resection cavity the physis should appear easy, flat, and wholesome after bar resection. At the conclusion of bar resection, normal physis should be visualized as a continuous cartilage line around the full circumference of the resection cavity. Marker place within the middle of the bone prevents the metaphyseal marker from becoming extraosseous with future remodeling. The first titanium marker has been placed centrally within the metaphysis proximal to the physis. Cranioplast confers quick structural power to the resection area, allowing full weight-bearing after surgery. Cranioplast may be injected into the resection defect in its liquid state, or it can be allowed to polymerize to the consistency of putty, then gently digitally pressurized into the cancellous bone of the resection mattress, preventing displacement. Most sufferers require harvesting fats from a distant site, and the gluteal area is usually used. Fat works well as an interposition materials for peripheral bars (C) as a end result of bone reworking and progress might end in cranioplast changing into prominent with time. For older patients with limited development remaining, the surgeon should consider epiphysiodesis to forestall angular deformity or limb- or bone-length discrepancy from occurring. Scanogram demonstrates the presence of a Harris progress "resumption" line on the proper however absent on the left and a 9mm limb-length discrepancy. Technique Placement of a reference Kirschner wire along the road of resection into the middle of the physeal arrest is very helpful in offering steering while the surgeon is working "blind" until regular physis is uncovered. Removing initial bone with a curette and saving it to fill the resection cavity after interposition materials has been placed facilitates speedy therapeutic and return to full strength. Inadequate resection Inadequate follow-up Insufficient physeal bar resection might result in recurrent bar formation. The physis should appear comparatively normal across the whole circumference of the resection cavity, not narrowed and irregular. On average, every affected person is prone to benefit from no much less than one additional procedure as a consequence of their physeal bar. Patients are allowed to bear weight as tolerated with crutches as needed for comfort, and early active joint vary of movement is encouraged. Noncontact sports activities are typically permitted three months after surgery and full-contact sports activities are allowed 6 months postoperatively in most patients. Restored physeal progress was, on average, 86% of the contralateral physeal growth price.
Diseases - Carnosinase deficiency
- Scholte Begeer Van Essen syndrome
- Hutchinson Gilford Progeria syndrome
- Quadriceps tendon rupture
- Lymphangiomatosis, pulmonary
- American trypanosomiasis
- Hearing disorder
- Johnston Aarons Schelley syndrome
Finpecia 1 mg with mastercardThe psoas tendon is visualized by retracting the iliacus medially with an Army-Navy retractor. For ambulatory patients, this is sometimes the one tissue that ought to be lengthened. If necessary, for nonambulatory patients and for more severe neuromuscular hip dysplasia, a partial or full division of the adductor brevis and different contracted tissues could be carried out. A quick transverse incision (pubis left, knee right) exposes the tendinous origin of the adductor longus (pectineus laterally, gracilis medially). On the opposite hand, identification of pathology and indications for psoas lengthening within the ambulatory cerebral palsy patient are less properly agreed upon. As a end result, I imagine that psoas lengthening is simply too typically not included within the surgical plan. In the Nineteen Seventies, Bleck recognized that release of the iliopsoas tendon on the lesser trochanter in the ambulatory patient resulted in excessive weak spot. In nonambulators, the iliopsoas combined tendon can be launched from the lesser trochanter, but care have to be taken not to violate the apophysis of the lesser trochanter so as to avoid heterotopic bone formation alongside the iliopsoas tendon sheath postoperatively. If important spasticity is current, ache and spasm may lead to difficulty in sustaining postoperative positioning in extension and abduction, leading to recurrence of hip flexion or adduction contractures. Botulinum toxin injected into the hip flexors and adductors on the time of surgery, effective pain administration, and meticulous care to avoid postoperative positioning in flexion and adduction are essential. Because of this iatrogenic danger with restricted corrective choices, this process should be deserted. The femoral nerve, artery, and vein are very near the psoas tendon however are anterior to the iliacus muscle. The iliacus muscle stomach can provide protection for these structures if the surgical approach is deep to it. Other safety is afforded by performing the lengthening of the tendon with the hip in the flexed position to chill out the neurovascular structures, instantly visualizing the tendon within the muscle stomach, and stimulating the tissue with electrocautery first before slicing (if the nerve is nearby, the knee will extend). The combination of femoral anteversion with hip and knee flexion deformity results in the visible look of a scissoring gait in ambulatory cerebral palsy sufferers and is more commonly the purpose for scissoring. In ambulators, solely adductor longus tenotomy should be performed, and it ought to be carried out not often. The adductors are more commonly spastic and contracted in additional extreme hemiplegic cerebral palsy. Adductor lengthening An abductor pillow is used full time for three weeks and half time for the next three weeks, and early range of motion is instituted. These procedures are commonly carried out in conjunction with osteotomy surgery, in which case weight bearing is typically begun three to four weeks postoperatively. When psoas lengthening is performed in conjunction with femoral derotation osteotomy, extreme anterior pelvic tilt may also improve. Postural and gait abnormalities caused by hip-flexion deformity in spastic cerebral palsy: therapy by iliopsoas recession. Intramuscular psoas lengthening improves dynamic hip perform in youngsters with cerebral palsy. This disruption is characterized by delayed and diminished peak knee flexion in swing phase. From a functional perspective, the quadriceps muscle group is definitely two groups, the primary consisting of the rectus femoris muscle and the second consisting of the triceps femoris muscle tissue (remaining three muscles). The muscular tissues usually exhibit a purely dynamic dysfunction through the first 6 years of life, characterised by a standard resting size and an exaggerated response to an utilized load or stretch. With time, between 6 and 10 years of age, the muscular tissues develop a onerous and fast or myostatic shortening, resulting in a permanent contracture. It has its origin on the anterior inferior iliac spine (direct head) and the innominate portion of the pelvis just proximal to the superior margin of the acetabulum (reflected head) and its insertion on the superior pole of the patella. The rectus femoris muscle fuses with the underlying vastus intermedius muscle a quantity of centimeters proximal to the superior pole of the patella.
Order 1mg finpecia otcBoth of those could be affected by neuromuscular conditions similar to cerebral palsy or myelomeningocele. Even so, with good neuromuscular perform, varusizing the femur may be nicely tolerated and can enhance the containment of the diseased femoral head. Contributing elements to the hip joint pathology could embrace musculotendinous contractures, ligamentous laxity, and coexistent acetabular dysplasia. Adductor lengthening, psoas lengthening, open reduction of the hip with capsulorrhaphy, and acetabuloplasty may must be thought of. Proximal femoral deformity can have an adverse impact on hip joint growth and exacerbates or contributes to muscle imbalance concerning the hip. Hip flexion and adduction deformities could be recognized by asymmetries in femoral place or uneven pelvic place. An examination under anesthesia can guide determination making relating to concurrent tendon lengthening. The impact on leg size could be managed by altering the amount of varusization and the scale of the wedge of bone removed (if any) relying on preoperative leg-length evaluation. This allows ease of exposure posterior to the muscle stomach of the vastus lateralis. The susceptible position additionally permits accurate management of femoral torsion comparable to the susceptible physical examination for femoral anteversion by palpation, thereby enhancing consistency of surgical realignment. The procedure involves placing the chisel for the blade plate in the applicable place within the femoral neck comparable to the quantity of varus to accomplish (eg, 20-degree varus correction corresponds to 70-degree chisel placement relative to the lateral femoral cortical surface: 90-degree blade plate minus 70 degrees equals 20 levels varusization), finishing the osteotomy, and placing the 90-degree blade plate as detailed in the Techniques part. The quantity of varusization could be determined based mostly on radiographs preoperatively or on intraoperative findings. The vastus lateralis is reflected from its proximal and posterior origins and elevated to expose the proximal femur subperiosteally. The fascia of the vastus lateralis is split transversely at the higher trochanteric apophysis and posteriorly in the periosteum of the intertrochanteric area and longitudinally adjoining to the insertion on the linea aspera (in the susceptible place, up is posterior). The vastus lateralis is elevated subperiosteally, and Crego retractors are positioned circumferentially on the intertrochanteric level. The entry point is just below the larger trochanteric apophysis if the patient is skeletally immature and through the higher trochanter after maturity. The entry level is chosen to allow insertion of the guidewire and chisel without violating the medial calcar. If preoperative planning indicated a 15-degree varusization goal, a 75-degree triangle could be used (see the Approach part above). Alternatively, dedication could be made primarily based on preoperative and desired postoperative alignment; for instance, the preoperative neck�shaft angle (150 degrees) minus the desired postoperative neck�shaft angle (120 degrees) equals 30 levels of varusization. In this case, the guidewire can be placed at a 60-degree angle to the femoral shaft when using the 90-degree plate. Intraoperative C-arm view displaying the guidewire at a 110-degree angle to the femoral shaft. The ideal lateral projection with femoral neck, femoral shaft, and guidewire coplanar improves accuracy and consistency. The chisel ought to be dislodged 5 to 10 mm before the osteotomy to permit for ease of later removal. Alternatively, a wedge of bone can be eliminated to accomplish a medial closing osteotomy. The entry point for the osteotomy noticed blade is decided by the implant (distance between the blade and the next angle within the plate for medialization). The beginning stage for this osteotomy varies relying on the specified quantity of shortening of the extremity. A starting point equivalent to the entry point for the primary osteotomy achieves full contact of the osteotomy after fixation. An entry level proximal (within the minimize of the primary osteotomy) results in less shortening, but incomplete ultimate apposition of the osteotomy surfaces. Alignment is checked after placement of the first screw each radiographically and by bodily examination. Correction of deformity by reducing the plate to the femoral shaft with a Verbrugge clamp.
Order cheap finpecia lineFixation of grafts to host bone requires interfragmentary screws and small plates, which ought to be readily available. Two or extra graft specimens must be out there for distal femoral allograft replacement in order that the closest measurement can be chosen. Oversized grafts will current issues with wound closure; verify gentle tissue rigidity earlier than final fixation of the graft to host bone. Be sensible about surgeon experience, help, equipment, and sources out there to perform complicated distal femoral reconstruction. Specialized training and intense tools and personnel calls for successfully preclude smaller community establishments from doing such surgical procedure. Either avoid using a tourniquet, or be wary of the tourniquet time in lengthy total knee reconstructions. If essential, the tourniquet may be let down for selected elements of the process to decrease limb ischemia time. Accordingly, the surgeon should aim for weight bearing as soon as potential after surgical procedure. If allograft reconstruction of the femur is critical, healing to host bone happens over a protracted time. Therefore, protected weight bearing will be required for an prolonged period of time in such cases. Range of motion should be assessed intraoperatively following distal femur reconstruction. Usually, the range of motion will depend on the standard of the delicate tissues and integrity of the extensor mechanism, assuming mechnical stability of the reconstruction has been achieved. If knee vary of motion have to be limited for a time period, a knee brace that enables motion only via a prescribed arc of motion could also be needed. Straight leg raises, isometric workouts, and ankle and calf rehabilitation must be potential quickly in spite of everything distal femoral reconstructions. A multimodal deep venous thrombosis prevention regimen should be instituted after surgical procedure, and the affected person monitored as appropriate. Early analysis and aggressive wound d�bridement might salvage the state of affairs in some cases, but removal of all allograft, cement, and implants in preparation for a staged reconstruction normally is important. Late deep infections with a virulent organism in a knee with massive bone loss and allograft reconstruction of deficient host bone might necessitate a limb amputation. Mechanical failure of distal femoral reconstructions normally occurs if the surgeon fails to achieve initial mechanical stability. Repeat surgical procedure is necessary to rebuild the femur and obtain rotational and axial stability to allow protected weight bearing after the process. If a tense hematoma develops, or new wound drainage is encountered, aggressive surgical decompression should be thought-about early, to keep away from the danger of an infection. Distal femoral allograft reconstruction for large osteolytic bone loss in revision complete knee arthroplasty. Treatment of main defects of bone with bulk allografts and stemmed elements during whole knee arthroplasty. Morsellized bone grafting compensates for femoral bone loss in revision complete knee arthroplasty. Radiographs ought to be assessed for stability of the reconstruction, and for healing of bone on the allograft�host bone junction. Bulk allografts heal to dwelling host bone, and allograft bone away from this healed junction stays non-viable over the long run. In load-sharing configurations, the place the allograft is supported by host bone or by metallic implants, the long-term outcomes are wonderful. If allograft bone is used in load-bearing configurations, late failure of the non-viable bone from repetitive loading is predictable. In some advanced reconstructions involving distal femur replacements with bulk allograft or limb salvage implants, the patient must be recommended to use protected weight bearing for a chronic time, such as 6 months or longer. Awareness and correct management of bone loss, by way of cement fill, metal augments, or bone grafting, are crucial for achieving stability and longevity of the newly implanted revision parts. The most typical areas of deficiency contain the posterolateral and medial tibial plateau. Smaller contained defects can usually be addressed with morselized bone graft or cement alone.
Purchase finpecia 1 mg without prescriptionTibial tray augmentation with modular steel wedges for tibial bone stock deficiency. The elastic moduli of human subchondral, trabecular, and cortical bone tissue and the size-dependency of cortical bone modulus. Osteolysis after total knee arthroplasty: influence of tibial baseplate surface finish and sterilization of polyethylene insert. Bone loss with revision whole knee arthroplasty: defect classification and options for reconstruction. Articulating versus static spacers in revision complete knee arthroplasty for sepsis. The influence of tibialpatellofemoral location on perform of the knee in patients with the posterior stabilized condylar knee prosthesis. Revision complete knee arthroplasty with use of modular elements with stems inserted with out cement. Injury to the popliteal artery and its anatomic location in whole knee arthroplasty. Magnetic resonance imaging with steel suppression for evaluation of periprosthetic osteolysis after whole knee arthroplasty. Chapter 23 Revision Total Knee Arthroplasty With Femoral Bone Loss: Distal Femoral Replacement B. Deficient bone in the distal femur could be changed by bone cement (polymethylmethacrylate), metal augments fixed to the revision femoral part, particulate bone graft or substitutes, bulk allograft to increase one or both femoral condyles, and full substitute of the distal femur with allograft or metal. The patient historical past is helpful in that findings in any of the following classes can alert the surgeon to the likelihood that vital bone loss may be encountered during revision surgery: the time elapsed because the index arthroplasty; the type of implant and fixation used; any historical past of diseases such as osteoporosis; superior age; corticosteroid use; use of cytotoxic medicine; irradiation; rheumatoid arthritis; and periprosthetic femoral fracture. The femoral condyles represent the structural columns that assist the revision femoral element. Previous implants fixed to bone with cement or by porous ingrowth require dissection for mobilization and extraction; this process incurs a finite amount of bone loss. Even fantastic osteotomes and saws used to develop a aircraft between the implant and bone are space-occupying and cause bone loss from the distal femur. Aggressive extraction of wellfixed femoral components without first developing a plane between exposed metal and bone can end result in avulsion of one or both femoral condyles. Correction of inside rotation of the previous femoral part will end in bone loss each anteriorly and posteriorly as the new component is oriented within the proper rotation. Osteopenia from stress-shielding of the periprosthetic femur, as nicely as osteolysis associated to wear debris particles, can end result in cavitary lesions in the distal femur that result in vital bone loss. The true lateral view of the knee joint can show the location and extent of osteolysis and bone loss in the distal femur. Oblique views of the knee usually end in obscuring of bony element by the steel implants. Therefore, a real lateral view of the knee ought to be obtained in 90 levels of knee flexion, by putting the complete leg, including the knee and ankle joints, flat on the radiograph desk. Intraoperative statement of bone loss after earlier element removal and thorough d�bridement of osteolytic lesions and inflammatory membrane is one of the best determinant of the nature and extent of bone loss. The surgeon should be ready for the worst-case scenario, as a outcome of preoperative radiographs can underestimate the extent of bone loss adjacent to the existing femoral element. Accordingly, allograft bone, a variety of revision implants, steel augments, and revision equipment ought to be out there. When this happens, the present femoral part can migrate into varus or valgus relative to the femoral shaft. Surgical therapy is directed at augmenting this bone loss following removal of the previous unfastened, unstable femoral part. Preoperative nuclear medication imaging, laboratory information, knee aspiration, and intraoperative frozen sections of periprosthetic tissues can assist in excluding sepsis. Infection should be dominated out earlier than reconstructing the distal femur in anticipation of implanting a revision femoral component. Stress-shielding of bone adjacent to the femoral component can lead to bone loss from the distal femur. When the existing femoral component is extracted, severe lack of bone could also be discovered in such circumstances. Severe medical comorbidities, integrity of the extensor mechanism, poor situation of the soft tissue, radiation necrosis of adjoining bone, immunosuppression, and metabolic bone problems should be evaluated rigorously to determine whether reconstruction of the distal femur is a reasonable option. Where main knee surgical procedure is contraindicated, nonoperative measures similar to analgesics, limited ambulation, assistive units corresponding to a walker or wheelchair, and knee bracing are different concerns.
|