|
Hydrea dosages: 500 mg
Hydrea packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
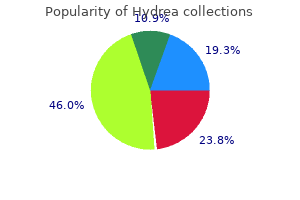
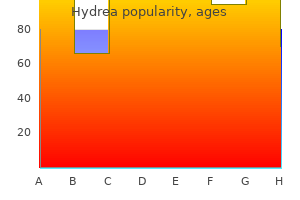
Order 500 mg hydrea mastercardChoice of instrumentation, method or approaches, and fusion levels must be deliberate. Early revision strategies typically involved explantation of the gadget, at instances for migration of the interbody device. The basic principle of revision backbone surgery ought to be saved in mind-if you want to change the outcome, you should do one thing totally different than you probably did the first time. Barrier of fibrin glue or hydrogel sealant posterior to interbody device to seal annulotomy. Spurred on by persistently glorious fusion charges regardless of early reviews of problems, bigger sequence had been reported including one during which a polyethylene glycol hydrogel sealant (Duraseal, Confluent Surgical Inc. Furthermore, "bone resorption inside the vertebral physique led to graft subsidence and lack of radiographic evidence of development toward fusion in multiple circumstances. The question raised was whether osteolysis could also be necessary in the early postoperative period in sufferers with new or continued ache. Histopathology of one of the sufferers revised for symptomatic posterior instrumentation confirmed granulation tissue subsequent to trabecular bone with suggestion of inflammation on the website of osteolysis. In addition, Balseiro and Nottheimer36 reported two circumstances of postoperative pain that confirmed evidence of osteolysis seemingly originating from their preexisting subchondral endplate cysts, citing their preoperative existence as a potential risk factor for subsequent osteolysis. These early stories seemed to counsel affiliation of osteolysis with early unfavorable results with variable longer term implications. They reported minimal associated cage migration or subsidence, though not quantified, and suggested the posterior instrumentation stabilized and negated any potential resultant instability. They calculated imply subsidence as 24% (13�40%) versus 12% (11�14%) within the two teams, respectively. The resultant loss of intrinsic strength of the graft and endplates was followed by subsidence of the graft and loss of intervertebral top. Eight of the 9 (88%) sufferers with cage migration required revision secondary to neurological symptoms. Later revisions found the cages fused in their posteriorly migrated place with each cage and heterotopic bone impingement on neural buildings. Placement of cages/spacers at peripheral locations of interbody house is possibly less prone to subsidence if osteolysis occurs. Preexistence of subchondral endplate cysts may be a threat issue for growing adjacent osteolysis. Osteolysis with related cage migration can be evident at or earlier than 6 weeks postoperative on plain radiographs. Maintaining an elevated awareness of those potential issues when osteolysis is present is critical. Cage migration with ensuing radicular ache typically, however not all the time, requires revision surgery with worse clinical outcomes. Complications of Posterior and Transforaminal Lumbar Interbody Fusion One issue in comparing outcomes of osteolysis is the differing postoperative imaging protocols. No patients required revisions for osteolysis, subsidence, or migration, though no clinical outcomes have been described. Subsequently, reappearance of the ache and incomplete enchancment of the numbness happen. He felt strongly the cause was a traumatic results of overzealous retraction of the nerve roots due to insufficient surgical publicity and advocated a wider publicity with partial facetectomy during nerve root decompression. Pheasant and Dyck54 in their 1982 article on failed lumbar disc surgical procedure, attribute the "battered root" and the resulting arachnoiditis as one explanation for failure. Soon thereafter in 1985, a German group reported successful treatment of the "battered root syndrome" with indwelling spinal twine stimulators. Battered root syndrome warrants further investigation into the incidence, mechanism, prevention, and treatment. On the contrary, one prospective sequence equally reported very high rates of osteolysis, however differed in that cage migration with resultant radiculopathy was additionally found at a high fee. Both revisions discovered a discrete inflammatory mass at time of decompression that exhibited histopathology of "diffuse osteoid and woven bone amidst a fibrovascular stroma densely populated by lymphocytes and eosinophils. They famous a ensuing decrease in the fee of radiculitis from 20 to 5% with use of the sealant.
Buy hydrea 500mg lineEndoscopic endonasal versus open transcranial resection of anterior midline cranium base meningiomas. Long-term tumor control of benign intracranial meningiomas after radiosurgery in a sequence of 4565 patients. Inducible cyclooxygenase and interleukin 6 gene expressions in nasal polyp fibroblasts: potential implication in the pathogenesis of nasal polyposis. Computed tomography and magnetic resonance analysis of allergic fungal sinusitis. An method to fulminant invasive fungal rhinosinusitis in the immunocompromised host. Fibrous dysplasia and aneurysmal bone cyst of the skull base presenting with blindness: a report of a uncommon domestically aggressive example. Surgery versus watchful waiting in patients with craniofacial fibrous dysplasia�a metaanalysis. The many faces of granulomatosis with polyangiitis: a review of the pinnacle and neck imaging manifestations. Ocular manifestations of systemic disease: antineutrophil cytoplasmic antibody-associated vasculitis. Otolaryngological development of granulomatosis with polyangiitis after systemic therapy with rituximab. Conversion of the mesenchyme into cartilage at the cranium base begins across the 40th day of gestation. The numerous foramina of the skull base are current inside this cartilaginous formation because the primitive nerves develop previous to chondrification and the cartilage develops round them. During the fifth week of gestation, the notochord passes into the basiocciput from the higher cervical vertebral our bodies. It then passes obliquely by way of the basiocciput, exiting ventrally to come in contact with the primitive pharynx, after which again into the basisphenoid and terminates simply caudal to the pituitary fossa at the dural margin. It passes through the basal mesoderm simply cephalad to the tip of the notochord to meet the precursor of the posterior pituitary, which forms from a diverticulum of the diencephalon. More rostrally, the paired presphenoid cartilages fuse to turn into probably the most anterior portion of the sphenoid bone. However, remaining cartilage could be found in varied synchondroses and persists into adult life, mostly in the foramen lacerum and petroclival junction. Skull base chondrosarcomas are thought to mostly come up from remnants of embryonal cartilage. It is bounded anteriorly by the tuberculum sellae and posteriorly by the dorsum sellae. Anterior to the tuberculum sellae is the prechiasmatic sulcus and the planum sphenoidale. The sella turcica is surrounded by four bony projections, the anterior and posterior clinoid processes. The dorsum sellae is contiguous posteroinferiorly with the clivus via the spheno-occipital synchondrosis. The optic canal is positioned above and is separated from the superior orbital fissure by the optic strut, and transmits the optic nerve and the ophthalmic artery. The sphenoid sinus is a variably pneumatized posterior extension of the paranasal sinuses. It is bordered by the ethmoid air cells anteriorly, clivus posteriorly, cavernous sinuses and cavernous inside carotid arteries laterally, sellae turcica and planum sphenoidale superiorly, and the nasopharynx inferiorly. There are a number of anatomic features related to the sphenoid which are important to assess when planning for surgical procedure (Table 2. The sphenoid sinus is split by complete and incomplete bony septations in numerous orientations. Care ought to be taken when surgically eradicating these septations to avoid carotid artery damage.
Purchase hydrea with mastercardMultiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. The relationship between anatomic variations of paranasal sinuses and chronic sinusitis in kids. Variations in paranasal sinus anatomy: implications for the pathophysiology of chronic rhinosinusitis and safety of endoscopic sinus surgery. Remarkable anatomic variations in paranasal sinus region and their clinical significance. Difference in the peak of the right and left ethmoidal roofs: a possible risk factor for ethmoidal surgery. Height and shape of the cranium base as danger components for cranium base penetration throughout endoscopic sinus surgery. Lateral retropharyngeal node metastasis from carcinoma of the upper gingiva and maxillary sinus. Anatomical variation and morphology within the place of the palatine foramina in adult human skulls from Greece. Bilateral nasal squamous carcinoma arising in papillomatosis: report of a case growing after chemotherapy for leukemia. Craniofacial resection for malignant paranasal sinus tumors: report of a global collaborative study. Patterns of dural involvement in sinonasal tumors: potential correlation of magnetic resonance imaging and histopathologic findings. European Rhinologic Society Advisory Board on Endoscopic Techniques within the Management of Nose, Paranasal Sinus and Skull Base Tumours. European place paper on endoscopic administration of tumours of the nose, paranasal sinuses and cranium base. The sinonasal tract: another potential "hot spot" for carcinomas with transcriptionally-active human papillomavirus. Endonasal endoscopic surgery for squamous cell carcinoma of the sinonasal cavities and skull base: oncologic outcomes based on treatment strategy and tumor etiology. Incidence and survival in sufferers with sinonasal cancer: a historic analysis of population-based information. Update on sinonasal adenocarcinoma: classification and advances in immunophenotype and molecular genetic make-up. Sinonasal undifferentiated carcinoma: clinical and pathologic options and a dialogue on classification, mobile differentiation, and differential analysis. Promising outcomes with chemoradiation in patients with sinonasal undifferentiated carcinoma. Salivary adenoid cystic carcinoma in Denmark 1990�2005: outcome and unbiased prognostic components including the good thing about radiotherapy. Sinonasal tract mucoepidermoid carcinoma: a clinicopathologic and immunophenotypic research of 19 instances combined with a complete review of the literature. Multidisciplinary treatment of olfactory neuroblastoma: patterns of failure and management of recurrence. Induction of olfactory neuroepithelial tumors in Syrian hamsters by diethylnitrosamine. Activation of retrovirus in transgenic mice: association with improvement of olfactory neuroblastoma. Perineural unfold of malignant melanoma of the pinnacle and neck: scientific and imaging features. Treatment end result and sample of failure in 77 sufferers with sinonasal natural killer/T-cell or T-cell lymphoma. Osteosarcoma of the jaw/craniofacial area: outcomes after multimodality treatment. Head and neck osteosarcoma in adults: the province of Alberta expertise over 26 years. The role of the human papillomavirus within the pathogenesis of Schneiderian inverted papillomas: an analytic overview of the proof.
Cheap hydrea amexPosterior migration of cervical spinal twine between break up laminae as a complication of laminoplasty. The utility of somatosensory evoked potential monitoring throughout cervical backbone surgery: how often does it prompt intervention and have an result on end result Outcomes after laminoplasty compared with laminectomy and fusion in patients with cervical myelopathy: a systematic review. Open-door laminoplasty for cervical stenotic myelopathy: surgical technique and neurophysiological monitoring. T-Saw laminoplasty for the management of cervical spondylotic myelopathy: medical and radiographic end result. C5 palsy after decompression surgery for cervical myelopathy: evaluation of the literature. Cervical alignment and range of motion after laminoplasty: radiographical information from more than 500 circumstances with [16] [17] [18] [19] [20] [21] [22] [23] [24] [25] [26] [27] 72 Kim et al. Complications Related to Cervicothoracic Instrumentation 12 Complications Related to Cervicothoracic Instrumentation Addisu Mesfin 12. Due to the transfer from the versatile cervical spine to the rigid section, thoracic spine instrumentation failure can nonetheless be encountered. Indications for an anteriorbased instrumentation would be a disc herniation at C7�T1, unstable fracture, and a main or metastatic lesion on the C7� T1 ranges. Posterior-based instrumentation is indicated when performing a protracted assemble in the cervical backbone corresponding to a C7 osteotomy for chin on chest deformity1 and for long thoracic constructs ending at T1. Need anatomic diagram of Cervicothoracic junction, prior copyrighted work is okay 12. Following a discectomy, a big diameter allograft or two small allografts could be placed. A standalone threaded cage that screws into the disc house followed by posterior-based stabilization can be an choice. In a cadaveric research, a C7 pedicle screw and T1 pedicle screw construct was discovered to be significantly stiffer than a C7 lateral mass construct in axial compression, torsion, bending, and flexion. In certain situations, the domino constructs are simpler to place than the transitional rods. A C5 to T2 construct, consisting of C7 pedicle screws, supplemented with one or two crosslinks was examined. If utilizing a threaded cage, mesh cage, or expandable cage, dislodgment of the cage may also happen. Patton et al reported the function of preoperative metabolic evaluation of the patient and subsequent treatment if deficiencies are famous. Osteoporosis is a vital consideration for proximal junctional kyphosis in sufferers with thoracic constructs ending at T1 or T2. In these cases, problems associated with poor bone quality similar to pedicle screw or lateral mass screw backing out may happen. With a C7�T1 spondylolisthesis and a protracted posterior assemble, it might be advisable to finish the construct at T2 or T3. During the revision, the instrumentation ought to be prolonged a minimum of one stage and supplemented with anterior instrumentation and fusion. Following three-column damage, elevated flexibility with the translaminar screws was noted. Seven years postoperatively, the affected person is doing properly with no changes in his instrumentation. The begin points and placement of those screws would be technically simpler than the present pedicle screws of the subaxial backbone. Cervicothoracic extension osteotomy for chin-on-chest deformity in ankylosing spondylitis. Surgical administration of cervical myelopathy coping with the cervical-thoracic junction. Surgical strategy to the cervicothoracic junction: can a normal Smith-Robinson approach be utilized
Purchase hydrea 500mg lineAlternatively, they may be reconstructed with a pedicled or free tissue flap with vascularized osseocutaneous or osseomyogenous flaps (such as a scapula free flap, fibular free flap, or iliac crest free flap) and subsequently be rehabilitated with a denture or implantretained prosthesis. The determination to obturate or reconstruct with a free flap depends on surgeon choice, in addition to patient factors. Local problems similar to bleeding might occur after maxillary surgical procedure because of the highly vascular pterygoid plexus and due to harm of the sphenopalatine and/or internal maxillary arteries. Postoperative bleeding from maxillectomy cavities may be initially managed with packing or operative ligation of offending vessels. Other native issues would include secondary mucocele formation and sinusitis. Orbital complications include postoperative hematoma in addition to injury to the nasolacrimal duct. Other potential orbital complications embrace enophthalmos, diplopia, extraocular muscle injury, and orbital abscess. Sparing the eye in craniofacial surgery for superior nasal vault malignant neoplasms: evaluation of profit. Extended inferior turbinate flap for endoscopic reconstruction of skull base defects. Beyond the nasoseptal flap: outcomes and pearls with secondary flaps in endoscopic endonasal skull base reconstruction. Prosthodontic guidelines for surgical reconstruction of the maxilla: a classification system of defects. Free tissue transfer for cranium base reconstruction evaluation of issues and a classification scheme for outlining cranium base defects. These tumors also require an equally sophisticated approach to intervention and imaging assessment. Singlemodality treatment with surgical procedure or radiation is the mainstay for the therapy of early-stage head and neck cancer. In the remedy of skull base cancers, both open craniofacial and endonasal approaches can be utilized independently or in concert. The postoperative imaging in these cases is notoriously difficult because of the alteration of the conventional anatomy, the surgical defects, and any reconstructions. Moreover, a wide range of tissue grafts and synthetic materials could additionally be utilized in these reconstructions. The false-positive cases are primarily the end result of treatmentrelated irritation. The false-negative circumstances are the outcomes of radiation and chemotherapy vascular compromise to the tumor mattress and the suppression of glucose transporters in the tumor. The problem in assessment of those pictures lies within the often-extensive modifications to regular anatomy that result from reconstruction, radiation therapy, and scarring. Clinically, recurrence could additionally be asymptomatic and never come to attention until its bulk has brought on gross distortion or is distinctly palpable. Imaging is therefore important within the posttreatment surveillance of head and neck most cancers. Skull base surgical procedure requires intricate reconstructions which are regularly essential to each preserve unfavorable histopathological margins from a large native excision and afford the affected person minimal morbidity whereas closing the surgical defect. In the native flap technique, neighboring tissue is repositioned geometrically to accommodate the surgical defect. The pedicle flap method differs in that donor tissue is rotated to fit the defect. Finally, free flap techniques might employ either a easy free flap or composite free flap. Either variant requires microvascular anastomosis of the vascular pedicle of the free flap to the local recipient vascular supply within the area of the reconstruction. In the easy variant, only one sort of tissue is incorporated into the flap, whereas the term composite belies the usage of multiple tissue types. The most typical forms of the latter are myocutaneous, fasciocutaneous, free jejunal interposition, and osseous composite flaps. It is really helpful that imaging and a physical examination be carried out each 3 to 4 months for the primary 2 years and each four to 6 months in years 2 to 5. A wide array of imaging modalities is available to contribute to the evaluation of the postoperative cranium base.
Buy generic hydrea 500 mg onlineThe analysis can be made with the swinging flashlight take a look at Transtentorial (uncal) herniation could occur as a outcome of a mind tumor or hematoma (subdural or epidural). Ipsilateral hemiparesis occurs because of stress on the corticospinal tract, which is located within the contralateral crus cerebri. Compression of the posterior cerebral artery, leads to ischaemia in visible cortex, resulting in contralateral homonymous hemianopia. Papilloedema is noninflammatory congestion of the optic disk as a outcome of elevated intracranial strain. It causes medial rectus palsy on tried lateral conjugate gaze and monocular horizontal nystagmus within the abducting eye. When an attempt is made to gaze contralaterally (relative to the affected eye), the affected eye shows no adduction. For instance, if the proper eye is affected the patient develops diplopia on trying to the left. Infratemporal area Infratemporal Fossa is the irregularly shaped cavity, situated under and medial to the zygomatic arch, not totally enclosed by Its boundaries are: Anteriorly is the maxilla bone (posterior surface) and posterior is the temporal bone (styloid and mastoid processes). At the medial boundary is the sphenoid bone (lateral pterygoid plate) and lateral is the mandible bone (ramus and coronoid process). At the roof is bigger wing of the sphenoid and infratemporal crest and the ground is open below. Temporal fossa is the shallow despair on the aspect of the cranium bounded by the temporal traces and terminating below the level of the zygomatic arch. Its boundaries are: Anteriorly is the frontal bone (zygomatic process) and zygomatic bone (the frontal process). The flooring is contributed by elements of the frontal, parietal, temporal, and larger wing of the sphenoid bone. Contents are: Temporalis muscle, the deep temporal nerves and vessels, the auriculotemporal nerve and the superficial temporal vessels. Pterygopalatine Fossa and Ganglion Pterygopalatine fossa is a cone-shaped paired melancholy deep to the infratemporal fossa and posterior to the maxilla on all sides of the skull, located between the pterygoid course of and the maxillary tuberosity, close to the apex of the orbit. Head and Neck the boundaries and relations of pterygopalatine fossa: Anterior Wall: Posterior floor of the maxilla bone. The openings and their contents in posterior wall are: Foramen rotundum to center cranial cavity (contains maxillary nerve); pterygoid canal to foramen lacerum (contains nerve of the pterygoid canal); palatovaginal canal to choana (containing pharyngeal branch of the maxillary artery and pharyngeal nerve from the pterygopalatine ganglion). The opening is the sphenopalatine foramen to the nasal cavity, which transmits the sphenopalatine artery and nasopalatine nerve. The opening is the inferior orbital fissure to the orbit which transmits the maxillary nerve. The opening is the larger palatine foramen to the palate, which transmits the higher palatine nerve and vessels. Contents: Maxillary nerve passes by way of foramen rotundum to enter the pterygopalatine fossa, pterygopalatine ganglion, maxillary artery (third part). It sends postganglionic parasympathetic fibers to the nasal and palatine glands and to the lacrimal gland via the maxillary, zygomatic, and lacrimal nerves. It also receives postganglionic sympathetic fibers (by the deep petrosal nerve and the nerve of the pterygoid canal), which are distributed together with the postganglionic parasympathetic fibers. The branches are: Orbital (innervate orbit and posterior ethmoidal and sphenoidal sinuses); pharyngeal department run in palatovaginal canal (supply the roof of the pharynx and sphenoidal sinus); posterior superior lateral nasal branches (supply the nasal septum, posterior ethmoidal air cells, and superior and middle conchae). Clinical Correlates Vidianectomy (carried out for vasomotor rhinitis cases) lesions the nerve of the pterygoid canal and ends in vasodilation; a scarcity of secretion of the lacrimal, nasal, and palatine glands; and a loss of basic and style sensation of the palate. Head and Neck Pituitary Anterior pituitary (or adenohypophysis) is a lobe of the gland that regulates a number of physiological processes (including stress, progress, replica, and lactation). Pituitary gland rests upon the hypophysial fossa of the sphenoid bone within the flooring of the middle cranial fossa and is surrounded by a small bony cavity (sella turcica) lined by a dural fold (diaphragma sellae). Hypothalamo-hypophysial tract consists of nerve fibres arising from the supraoptic and paraventricular nuclei of the hypothalamus and projecting into the posterior lobe of the pituitary gland. Hypothalamo-hypophysial portal system consists of two sets of capillaries: one within the hypothalamus (median eminence) and the opposite in the hypophysis cerebri (sinusoids of pars anterior). The neurons of the hypothalamus produce hormones-releasing factors in the capillaries of the median eminence and upper a part of the infundibulum. Arterial provide: Superior and inferior hypophyseal arteries supply the pituitary gland. Venous Drainage: There are three routes for venous drainage of neurohypophysis: To adenohypophysis by way of lengthy and quick portal vessels; into dural venous sinuses via inferior hypophyseal veins and to hypothalamus by way of capillaries passing to median eminence.
Purchase generic hydrea lineSuperior thoracic artery � Mammary gland receives blood from the axillary artery branches (lateral thoracic artery, thoracoacromial artery); the posterior intercostal arteries and the inner thoracic (mammary) artery branches. Anatomical Snuff Box the anatomical snuff box is an elongated triangular melancholy seen on lateral side of the wrist immediately distal to the radial styloid process, will get extra prominent when the thumb is fully prolonged. Boundaries Borders � Anterolaterally (Radial) � Tendons of abductor pollicis longus � Extensor pollicis brevis � Posteromedially (ulnar) � Tendon of extensor pollicis longus � Proximal border � Styloid means of the radius � Distal border � Apex of the schematic snuffbox isosceles triangle Scaphoid, trapezium and base of first metacarpal bone* � Skin and superficial fascia � Cephalic vein (subcutaneous) � Radial nerve branches (subcutaneous) Contents Radial artery (pulse) * At the ground, two joints are partly evident - the wrist joint and the primary carpometacarpal joint. Floor Roof Note: the superficial radial nerve, may be rolled from aspect to aspect on the tendon of extensor pollicis brevis. The tendons involved are abductor pollicis longus and extensor pollicis brevis and Finkelstein check turns into positive. Radial Artery � Anatomic snuff field is a triangular interval bounded anterolaterally by the abductor pollicis longus (and extensor pollicis brevis) and posteromedially by the tendon of the extensor pollicis longus. Floor is fashioned by extensor carpi longus and brevis tendons � Abductor pollicis longus and extensor pollicis brevis type the anterolateral wall of anatomical snuff field. It extends from the lateral margin of the radius to the styloid process of the ulna, the pisiform, and the triquetrum and is crossed superficially by the superficial department of the radial nerve. Posterior interosseous nerve runs under which compartment of extensor retinaculum: a. Flexor carpi radialis � the tendon of flexor carpi radialis passes by way of a tunnel created by a fascial slip on the roof of flexor retinaculum. Abductor pollicis longus � First extensor compartment of wrist has two tendons: Abductor pollicis longus and extensor pollicis brevis. The aim is to distinguish infectious tenosynovitis from superficial or localized abscess. Midpalmar longitudinal crease signifies the lateral limit of the hypothenar eminence. Proximal row (lateral to medial): Scaphoid, Lunate, Triquetral, Pisiform Distal row: Trapezium, Trapezoid, Capitate, Hamate Metacarpals are miniature lengthy bones consisting of bases (proximal ends), shafts (bodies), and heads (form knuckles). Capitate begins to ossify within the second month; the hamate on the finish of the third month; the triquetrum in the third yr; and the lunate, scaphoid, trapezium and trapezoid within the fourth yr in females (fifth yr in males). The pisiform begins to ossify in the ninth or tenth 12 months in females, and the twelfth in males. Some authors point out: Lunate-fourth 12 months, Scaphoid and trapezoid-fifth year and trapezium-sixth year 711 Self Assessment and Review of Anatomy Clinical Correlations � Scaphoid is the most commonly fractured carpal bone. A fracture results in osteonecrosis of the scaphoid bone (proximal fragment) � There is tenderness on the flooring of the anatomical snuff box. Major supply from dorsal surface � Major blood supply (~80%) of scaphoid comes via dorsal surface through dorsal branches of radial artery. Trapezium � the capitate bone is the most important of the carpal bones within the human hand, and occupies the center of the wrist. Lies within the proximal row of carpal bones � the carpal bones within the proximal row are scaphoid, lunate, triquetral and pisiform. Epiphysis is at the head � Epiphysis is present on the heads of all metacarpals, besides first metacarpal (epiphysis is on the base). Joints Midcarpal Joint is a airplane synovial plane joint between the proximal and distal rows of carpal bones and allows gliding First Carpometacarpal Joint is a saddle synovial joint between trapezium and the primary metacarpal bone, permitting flexion Plane synovial joints are current between the carpal bones and the medial 4 metacarpal bones, allowing a simple Metacarpophalangeal Joints are ellipsoid (> condyloid) joints that permit flexion and extension, and abduction and Interphalangeal Joints are hinge synovial joints that permit flexion and extension. It has 120� of flexion and extension, about 40� of abduction and adduction, and a few rotation attainable. Fascia Palmar aponeurosis is a triangular fibrous layer overlying the tendons in the palm and protects the superficial palmar arterial arch and palmar digital nerves. Three subgroups of radial (abductor pollicis longus and extensor pollicis brevis), central (abductor pollicis brevis and opponens pollicis) and ulnar (flexor pollicis brevis) muscular tissues are concerned. Lumbricals 1 and a pair of arise from lateral facet of lateral two tendons of the flexor digitorum profundus. Lumbricals three and four take origin from adjoining sides of medial three tendons of the flexor digitorum profundus. The tendons of lumbricals cross the lateral side of metacarpophalangeal joints to be inserted into the lateral side of dorsal digital expansion of the corresponding digit from second to fifth. Patient is asked to tightly hold a card between the fingers while the examiner tries to pull it out. On the index finger and little finger, the enlargement is strengthened by extensor indicis and extensor digiti minimi, respectively, which blends with it. Self Assessment and Review of Anatomy Clinical Correlations � Mallet finger (hammer or baseball finger) is a finger with permanent flexion of the distal phalanx as a end result of an avulsion of the lateral bands of the extensor tendon to the distal phalanx.
Buy 500 mg hydrea overnight deliveryThis provides the best evaluation of the esophageal mucosa and allows diagnostic. Upper endoscopy should be the initial check in sufferers with dysphagia as a end result of a meals impaction. If the mucosa seems normal, esophageal biopsies ought to be obtained to evaluate for the presence of eosinophilic esophagitis. A nasogastric catheter with electronic probes is used to measure pressure during esophageal contractions and higher and decrease esophageal body and sphincter responses to swallowing. Manometry is indicated in patients with dysphagia in whom a barium esophagogram or upper endoscopy reveals no abnormality. Combined recordings of esophageal pH ranges and intraluminal esophageal pressure may help in diagnosing sufferers with refluxinduced esophageal spasm. A barium swallow is step one in evaluating patients with signs of esophageal dysphagia especially if an obstructive lesion is suspected. Upper endoscopy is the recommended initial research with acute obstruction corresponding to an impacted meals bolus. Improvement in symptoms means that the dysphagia is expounded to the presence of gastroesophageal reflux (see Table 2. Achalasia and Other Esophageal Motility Disorders Definitive remedy of achalasia is surgical cardiomyotomy with partial fundoplication (Heller myotomy; see Chapter 4). Early outcomes present similar efficacy, although the longterm sturdiness and consequences of endoscopic myotomy continue to be investigated. A trial of nitrates, calcium channel blockers or phosphodiesterase inhibitors could also be useful in sufferers with spastic esophageal problems. Pearls A detailed historical past can help establish the cause of dysphagia in roughly 80% of patients. Intermittent signs and dysphagia to both liquids and strong meals are options that the majority strongly suggest a motility disorder. An 80yearold man presents with progressive dysphagia for strong food over the previous three months. A 65yearold man presents with progressive dysphagia for liquids and solids over the previous few weeks. The finest take a look at to set up the analysis in the affected person introduced in Question 6 is which of the next The greatest diagnostic check to set up the analysis of achalasia is which of the following A 65yearold man with intermittent dysphagia is noted to have an esophageal ring on higher endoscopy. A 21yearold man is seen within the clinic for the analysis of painful swallowing and dysphagia for the previous 2 weeks. His medications include a steroid inhaler for bronchial asthma and doxycycline to deal with reasonably severe pimples. He has occasional heartburn (less than twice per month) and takes ranitidine as wanted. In the setting of a previous longterm history of heartburn, the differential analysis consists of reflux esophagitis, peptic stricture, or adenocarcinoma of the esophagus. B In achalasia, the postganglionic nitric oxidecontaining neurons are lost, thereby resulting in failure of rest of the decrease esophageal sphincter. His symptoms are also according to a benign stricture, given his longstanding reflux signs. This presentation could probably be secondary to stroke, significantly in light of the weak spot on his left aspect. Esophageal cancer is usually associated with weight reduction and progressive dysphagia for stable food. When esophageal dysphagia is suspected, one should carry out a barium esophagogram with or with out an upper endoscopy. In a patient in whom gastroesophageal reflux is a suspected cause of dysphagia, pH testing could also be carried out.
|