|
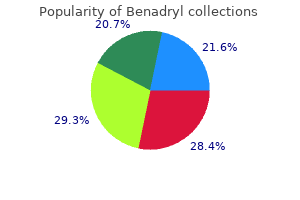
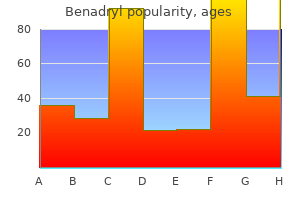
Benadryl dosages: 25 mg
Benadryl packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills
Buy benadryl 25mg amexCombination Ballistic and Ultrasonic Devices Several producers have launched combined ultrasonic and pneumatic gadgets that aim to combine the superior fragmentation capacity of the pneumatic part with the flexibility of the ultrasonic modality to simultaneously evacuate stone fragments. Broadly speaking, the mix devices are used in an analogous fashion because the stand-alone units. The target stone is identified, and steady gentle pressure is applied via the lithotrite, till fragmentation and evacuation occur. A research of more than 5000 sufferers collated via the Clinical Research Office of the Endourological Society found that the lithotrite had no effect (Chu et al. The authors in contrast the Cyberwand, a dual-probe ultrasonic system, the Lithoclast Select, a mix pneumatic and ultrasonic gadget, and the Stone Breaker, a portable pneumatic device. Ultimately, they found no difference in stone clearance charges, and general security and efficacy had been comparable. Perhaps the technology of the lithotrite is of secondary importance to the strategy of the surgeon. The advent of laparoscopic and subsequently robotic renal and ureteral stone elimination procedures has provided the urologist with one other means to circumvent open stone surgical procedure. In sure cases a laparoscopic or robotic method could also be considered a most well-liked therapy. Situations that may profit from a laparoscopic strategy embrace pyeloplasty with pyelolithotomy; sufferers harboring stones in poorly functioning polar areas or with nonfunctioning kidneys; pelvic kidneys containing a big stone quantity, by which laparoscopic techniques can be used to mirror overlying bowel, permitting pyelolithotomy or percutaneous stone removing; and ureterolithotomy for the extremely rare endoscopic failure or large/multiple impacted ureteral calculi. Such procedures could be technically demanding and require a talented laparoscopic/ robotic surgeon to be performed with minimal morbidity. Andressen R, Fedel M, Sudhoff F, et al: Quality of semen after extracorporeal shock wave lithotripsy for lower urethral stones, J Urol 155:1281�1283, 1996. Bohris C, Roosen A, Dickmann M, et al: Monitoring the coupling of the lithotripter remedy head with skin during routine shock wave lithotripsy with a surveillance camera, J Urol 187:157�163, 2012. Chaussy C, Fuchs G: Extracorporeal lithotripsy within the therapy of renal lithiasis. Results from the Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study, Urol Int 91:340�344, 2013. Crum L: Surface oscillations and jet development in pulsating bubbles, J Phys Colloq 40:1979. Delius M, Jordan M, Eizenhoefer H, et al: Biological effects of shock waves: kidney haemorrhage by shock waves in dogs�administration price dependence, Ultrasound Med Biol 14:689�694, 1988. Demirci D, Sofikerim M, Yalcin E, et al: Comparison of standard and step-wise shockwave lithotripsy in management of urinary calculi, J Endourol 21:1407�1410, 2007. Eichel L, Batzold P, Erturk E: Operator expertise and adequate anesthesia improve treatment end result with third-generation lithotripters, J Endourol 15:671�673, 2001. Proceedings of the sixteenth International Congress on Acoustics and 135th Meeting of the Acoustical Society of America; 1998. Greenstein A, Matzkin H: Does the rate of extracorporeal shock wave supply affect stone fragmentation Janetschek G, Frauscher F, Knapp R, et al: New onset hypertension after extracorporeal shock wave lithotripsy: age related incidence and prediction by intrarenal resistive index, J Urol 158:346�351, 1997. Rehman J, Monga M, Landman J, et al: Characterization of intrapelvic strain throughout ureteropyeloscopy with ureteral entry sheaths, Urology sixty one:713�718, 2003. Thuroff S, Thorsten B, Chaussy C: Anatomy associated shockwave power using Siemens Lithostar multiline, J Urol 159(Suppl):34, 1988. Traxer O, Thomas A: Prospective analysis and classification of ureteral wall injuries ensuing from insertion of a ureteral entry sheath throughout retrograde intrarenal surgery, J Urol 189:580�584, 2013. Kobayashi M, Naya Y, Kino M, et al: Low dose tamsulosin for stone expulsion after extracorporeal shock wave lithotripsy: efficacy in Japanese male sufferers with ureteral stone, Int J Urol 15:495�498, 2008. Kupeli B, Irkilata L, Gurocak S, et al: Does tamsulosin improve decrease ureteral stone clearance with or without shock wave lithotripsy Liedle B, Jocham D, Lunz C, et al: Five yr follow-up of urinary stone treatment with extracorporeal shock wave lithotripsy, J Endourol 2:157�162, 1988.
Order benadryl pills in torontoStents were routinely left in place for 6 to 8 weeks, after which diagnostic studies were performed. With a imply follow-up approaching 1 year, successful fee of 81% was achieved in 16 sufferers. However, two sufferers developed distal ureteral strictures, in all probability resulting from the larger-diameter inflexible instrumentation. Butani and Eshghi (2008) recognized 96% success charges in main procedures with a median 5-year follow-up, though inflexible ureteroscopy and preprocedure stents have been needed. Advances in instrumentation and approach now allow a ureteroscopic approach to be carried out reliably at a single setting (Conlin and Bagley, 1998), and this is now thought-about the standard. Once the ureteroscope has been eliminated, a stent is superior over the remaining wire utilizing fluoroscopic steerage. A Foley catheter is left indwelling, again to obviate the chance of reflux and extravasation at the web site of the endopyelotomy incision and to quickly establish any significant bleeding. Clinical and radiographic followup is then continued at 6- to 12-month intervals for 24 to 32 months. With a imply follow-up of slightly more than 12 months, they achieved a success rate of 87. These investigators combined endoluminal ultrasound with their ureteroscopic strategy to definitively determine crossing vessels or a ureteropelvic septum, which is present in sufferers with high-inserting ureters. The authors believed this helped them definitively web site their endopyelotomy incision. Different modalities were used for the endopyelotomy, including electrocautery and holmium laser. There were no significant bleeding complications, and all sufferers had been discharged within 24 hours of the procedure. Several investigators have reported success rates of 70% to 80% with follow-up out to 5 years using ureteroscopic holmium laser endopyelotomy (ElAbd et al. Improved outcomes (91% success rates) have been reported by Conlin (2002) with retrograde endopyelotomy in patients when culling patients with crossing vessels greater than 4 mm utilizing preoperative ultrasonography. Regardless, one of the best retrograde endopyelotomy success rates nonetheless lag behind those of open or laparoscopic pyeloplasty. Complications of this method have diminished in frequency and severity with the refinement of ureteroscopic instrumentation and the introduction of small-caliber holmium laser fibers. Postprocedural ureteral strictures are uncommon in contemporary sequence, and angiographic embolization and nephrectomy are uncommon when the retrograde method is used. Most complications are minor and relate primarily to urinary leak, stent migration, and an infection (Gerber and Kim, 2000; Tawfiek et al. Ponsky and Streem (2006) reported on 64 patients present process either ureteroscopic endopyelotomy or fluoroscopically guided cautery balloon endopyelotomy and located equivalent success charges with both procedures yet greater main complication rates within the cautery wire balloon endopyelotomy, particularly transfusion and selective embolization. Improved ureteroscopic instrumentation, laser technology, and higher outcomes make ureteroscopic endopyelotomy the present retrograde method of alternative. Another benefit of the ureteroscopic strategy is a decrease in value in contrast with the use of the cautery wire balloon, assuming ureteroscopic tools and electroincision or holmium laser are already obtainable. Moreover, the risks and morbidity of percutaneous access are prevented with the ureteroscopic process. Another examine confirmed endopyeltomies to be less expensive than minimally invase or open pyeloplasty. Open and minimally invasive pyeloplasty approaches were cost impartial, making minimally invasive pyeloplasty the best option when obtainable (Jacobs et al. The indications for a ureteroscopic endopyelotomy embrace functionally important obstruction, as defined earlier. Contraindications include long areas of obstruction and upper tract stones, that are greatest managed simultaneously with various approaches, often percutaneously or laparoscopically. Another consideration is that in patients with vital hydronephrosis, the evidence signifies an antegrade endopyelotomy could additionally be extra efficacious (Lam et al. In males, flexible ureteroscopes are used with ureteral entry sheaths and versatile ureteroscopes for most retrograde endopyelotomies.
Proven benadryl 25mgThis apply helps to minimize the risk of urinoma formation resulting in potential disruption of the suture line, scarring, or sepsis. A traction suture can be placed on the lateral facet of the proximal ureter, under the extent of obstruction. The apex of this lateral, spatulated side of the ureter is then dropped at the inferior border of the pelvis whereas the medial facet of the ureter is dropped at the superior fringe of the pelvis. It additionally permits discount of a redundant pelvis or straightening of a tortuous proximal ureter. The proximal ureter is then dissected cephalad to the renal pelvis, leaving a large amount of periureteral tissue to protect the ureteral blood provide. As discussed earlier, our choice for grownup patients is to routinely carry out the anastomosis over an internal ureteral stent, which is left indwelling. If the renal pelvis is exceptionally redundant, a "discount" pyeloplasty can be performed by excising the redundant portion of the pelvis, but this is usually unnecessary (Morsi et al. The cephalad facet of the pelvis is then closed with running absorbable sutures all the method down to the dependent portion, which will subsequently be anastomosed to the ureter. This incision may be subcostal however is normally carried out through the mattress of the twelfth rib or carried anteriorly off its tip. An anterior extraperitoneal approach is chosen by some because it allows surgical repair with minimal mobilization of the pelvis and proximal ureter. Like the anterior extraperitoneal strategy, posterior lumbotomy is best suited to comparatively skinny patients with out previous ipsilateral surgery. In the arms of the experienced laparoscopic surgeons, it has been proven to present lower patient morbidity, shorter hospitalization, and quicker convalescence, with the reported success rates matching these of open pyeloplasty (90%). Following the similar surgical rules of anatomic dissection and restore used in open pyeloplasty, laparoscopic pyeloplasty has been shown to present success rates surpassing these of endopyelotomy by approximately 10% to 30%. In the identical meta-analysis the authors discovered that in case series containing greater than a hundred patients, laparoscopic pyeloplasty was associated with success charges starting from Chapter 89 94% to 100%, although follow-up intervals tended to be quick (Autorino et al. Preoperative, intraoperative, and postoperative techniques are analagous in these approaches; thus the subsequent section refers to laparoscopic and robotic pyeloplasty. The indications and contraindications for a laparoscopic restore are just like these for either an endourologic or an open operative procedure. Cases requiring the transposition of crossing vessels obstructing the ureteropelvic junction or the size reduction for massively dilated renal pelvis are appropriate for the laparoscopic method. Absolute contraindications to intervene embody the presence of uncorrected coagulopathy, the absence of adequate treatment of lively urinary tract an infection, and the presence of cardiopulmonary compromise unsuitable for surgical procedure. The goal of the laparoscopic surgical procedure is to provide a tensionfree, water-tight restore with a funnel-shaped drainage product to relieve clinical symptoms and to preserve renal perform. For every method, a dismembered Andersen-Hynes pyeloplasty, which is most popular by most surgeons, or one of many nondismembered strategies such as Y-V plasty and flap pyeloplasty (Culp) analogous to those described for the open pyeloplasty can be used. The preliminary transperitoneal method to laparoscopic pyeloplasty was first described by Schuessler et al. This method has been probably the most widely used laparoscopic technique due to its associated large working space and familiar anatomy. Before the laparoscopic portion of the procedure, cystoscopy with retrograde pyelography could additionally be first performed to define the anatomy and ensure the prognosis, followed by placement of a ureteral stent and a urethral Foley catheter. The patient is placed in a 45-degree lateral decubitus place, and access to the peritoneal cavity is obtained through either the Veress needle or the Hassan entry approach. Colonic mobilization to expose the retroperitioneal buildings is the preliminary step of the laparoscopic procedure, though transmesenteric strategy without bowel mobilization has been reported if renal pelvis or ureter may be readily recognized through the descending colonic mesentery (Romero et al. Extensive dissection of the ureter and extreme electrocautery use in close proximity to the ureter ought to be averted to decrease damage to its vascular supply. Transperitoneoscopic view of a affected person present process a proper robotic laparoendoscopic single-site pyeloplasty. The anterior extraperitoneal laparoscopic method to pyeloplasty was first described by Hsu et al. Cystoscopy with retrograde pyelography and ureteral stent placement are first carried out as described earlier. For the anterior extraperitoneal strategy, the medial mobilization of the peritoneal sac containing the bowel contents en bloc. Subsequently, full publicity of the anterior features of the retroperitoneal structures together with the ipsilateral ureter and kidney comes into view. The robotic-assisted laparoscopic pyeloplasty within the experimental setting was first reported by Sung et al.
Purchase discount benadrylThe first investigation in case of a bladder stone is ultrasonography to rule out the presence of concomitant renal or ureteric calculi. In reality, they type secondary to obstruction of urethra at any level of urinary stasis in urethral diverticula. Presence of a foreign physique and urinary an infection present a conducive milieu for stone formation (Rivilla et al. In the presence of infection stones, the generally isolated organisms are Escherichia coli, Proteus spp. Most of these stones are small, spherical, with no core or nucleus, and composed primarily of struvite (magnesium ammonium phosphate), although other sorts corresponding to calcium phosphate and uric acid have been reported (Verit et al. Urethral stricture is the main cause for the formation of urethral stones as mentioned earlier. On the other hand, placement of hairbearing grafts for the administration of urethral stricture or hypospadias has resulted in urethral stones as properly. The hair acts as a nidus for precipitation and inspissation of lithogenic salts and ends in primary calculi in the urethra (Singh and Hemal, 2001). These stones remain adherent to the hair ball and the urethral mucosa, causing partial obstruction and further stone formation. Attempts at epilation before engraftment have decreased however not eliminated the risk: the follicles persist and result in hair growth in 3% to 6% of patients (Singh and Hemal, 2001). The creation of brachytherapy as a remedy modality for carcinoma prostate over the last two decades requires the position of radioactive seeds into the prostate. These seeds can migrate or intrude into the prostatic urethra and may type a nidus for stone formation. Cryoablation causes ischemic necrosis of the gland, and necrosis with persistent inflammation may give rise to stones (Aus et al. In the previous few a long time, the urethral calculi have become a rarity in the industrialized Western societies, although not so uncommon in and endemic regions of Asia and Middle East (Aegukkatajit, 1999; Amin, 1973; Menon and Martin, 2002; Seltzer et al. More latest epidemiologic studies have instructed a declining incidence of lower urinary tract bladder and urethral calculi (Trinchieri, 2008). Urethral calculi have been exceedingly more widespread in males, with a bimodal age distribution. The first peak happens in early childhood, and the second peak incidence happens within the fourth or fifth many years of life (Kamal et al. Shorter size of the feminine urethra and better peak move rates in adolescence and younger age groups might have the protecting effect for the younger demographic age group (Kamal et al. Clinical Presentation and Evaluation the clinical presentation is determined by the kind and location of the stone. Patients with migratory calculi normally have a history of stone disease, earlier surgeries for stone or instrumentation of lower tract, a vague history of flank pain in the previous 1 or 2 weeks, suggesting origin from the upper tracts, and decrease urinary tract signs (Verit et al. More commonly, urethral calculi patients present with acute painful retention of urine from sudden impaction of the stone. Few authors have innovated with the Microperc armamentarium for fragmenting the urethral calculi (Desai and Ganpule, 2017). Open cystolithotomy remains the final choice in the occasion of failure of endourologic maneuvers (Kamal et al. The distance of the stone from the exterior meatus and the surface traits of the stone are the factors to be thought-about earlier than contemplating remedy options. Milking the stone out from the meatus is an choice, however caution relating to urethral harm ought to be exercised (Kamal et al. If the stone is large or the floor is rough and irregular, extraction by milking is to be condemned. Few authors have famous success with simple instillation of lidocaine jelly into the urethra for small distal stones (El-Sharif and El-Hafi, 1991; Kamal et al. In situ lithotripsy is feasible using either electrohydraulic or Swiss lithoclast with a success price of as much as 80% (Kamal et al. For stones positioned in the fossa navicularis and distal urethral stones, manipulation with a forceps underneath anesthesia is successful. A ventral meatotomy helps in controlled removing of the stone and really reduces urethral trauma.
Buy cheap benadryl 25 mgGeramoutsos I, Gyftopoulos K, Perimenis P, et al: Clinical correlation of prostatic lithiasis with chronic pelvic ache syndromes in young adults, Eur Urol 45:333�337, 2004. Grasso M: Experience with the holmium laser as an endoscopic lithotrite, Urology 48:199, 1996. Hahnfeld L, Nakada S, Sollinger H, et al: Endourologic remedy of bladder calculi in simultaneous kidney�pancreas transplant recipients, Urology fifty one:404, 1998. Harada K, Igari D, Tanahashi Y: Gray scale transrectal ultrasonography of the prostate, J Clin Ultrasound 7:45�49, 1979. Hayashi Y, Yasui T, Kojima Y, et al: Management of urethral calculi related to hairballs after urethroplasty for extreme hypospadias, Int J Urol 14:161�163, 2007. Hegele A, Olbert P, Wille S, et al: Giant calculus of the posterior urethra following recurrent penile urethral stricture, Urol Int 69:160�161, 2002. Hussain I: Primary extracorporeal shock wave lithotripsy in management of large bladder calculi, J Endourol eight:183�186, 1994. Isen K, Em S, Kilic V, et al: Management of bladder stones with pneumatic lithotripsy by using a ureteroscope in youngsters, J Endourol 22:1037�1040, 2008. Kilciler M, Sumer F, Bedir S, et al: Extracorporeal shock wave lithotripsy therapy in paraplegic patients with bladder stones, Int J Urol 9:632�634, 2002. Kim H, Cheigh J, Ham H: Urinary stones following renal transplantation, Kor J Int Med sixteen:118, 2001. Steinmetz R, Barrett W: Urethral stone formation after permanent radioactive seed implant for prostate most cancers, Am J Clin Oncol 29:424�425, 2006. Subbarao P, Lal R, Bhatnagar V, et al: Multiple urethral calculi in youngsters: report of two cases, Jpn J Surg 28:1210�1212, 1998. Takasaki E: A 4 year retrospective research of urolithiasis, Dokkyo J Med Sci 6:one hundred twenty, 1979. Terai A, Arai Y, Kawakita M, et al: Effect of urinary intestinal diversion on urinary danger factors for urolithiasis, J Urol 153:37�41, 1995. Thomas R, Lee S, Salvatore F, et al: Direct percutaneous pouch cystostomy with endoscopic lithotripsy for calculus in a continent urinary reservoir, J Urol a hundred and fifty:1235�1237, 1993. Trinchieri A: Epidemiology of urolithiasis: an update, Clin Cases Miner Bone Metab 5(2):one hundred and one, 2008. Tugcu V, Polat H, Ozbay B, et al: Stone formation from intravesical hem-o-lok clip migration after laparoscopic radical prostatectomy, J Endourol 23(7):1111�1113, 2009. Valyasevi A, Van Reen R: Pediatric bladder stone illness: current status of research, J Pediatr seventy two:546�553, 1968. Verit A, Savas M, Ciftci H, et al: Outcomes of urethral calculi sufferers in an endemic area and an undiagnosed primary fossa navicularis calculus, Urol Res 34:37�40, 2006. Lipke M, Schlusinger D, Sheynkin Y, et al: Endoscopic remedy of bladder calculi in post-renal transplant sufferers: a 10-year experience, J Endourol 18:787�790, 2004. Millan Rodrigues F, et al: Treatment of bladder stones with out associated prostatic surgical procedure: outcomes of a prospective research, Urology sixty six:505�509, 2005. Miyazawa K, Matoba M, Minato H, et al: Seed migration after transperineal prostate brachytherapy with I123 free seeds: evaluation of its risk elements, Jpn J Radiol 30:635�641, 2012. Muezzinoglu B, Gurbuz Y: Stromal microcalcification in prostate, Malays J Pathol 23:31�33, 2001. Ord J, Lunn D, Reynard J: Bladder administration and risk of bladder stone formation in spinal twine injured sufferers, J Urol one hundred seventy:1734�1737, 2003. Parladidius N, Tsiamis C, Diamantis A, et al: Methods of lithotripsy in historic Greece and Byzantium, J Urol 178:1182�1183, 2007. Peabody Christopher, Mailhot Thomas, Perera Phillips: Ultrasound diagnosis of urethral calculi, West J Emerg Med 13(6):515, 2012. Phillippou P, Moraitis K, Masood J, et al: the administration of bladder lithiasis within the fashionable period endourology, Urology seventy nine:980�986, 2012. Rivilla F, Luis A, Llanos D, et al: Giant urethral calculus in a 6-year-old-girl, J Pediatr Urol four:469�471, 2008. Selli C, Barbagli G, Carini M, et al: Treatment of male urethral calculi, J Urol 132:37�42, 1984.
Buy benadryl cheapThe innermost is the mucosa, the middle muscular layer is the muscularis, and the outer layer is the adventitia. The mucosa consists of transitional epithelium, which has four to six layers of cells when the ureter is contracted. The mucosa also incorporates many longitudinal folds that give the empty ureter a characteristic stellar outline. The muscular wall of the ureter consists of two longitudinal layers separated by a center round layer that may not be distinct from each other, particularly in the stomach phase of the ureter. Mostly, these muscle fibers appear to be spirally organized by the light microscopy. However, within the distal ureter, the inner spirals are steep and the outer spirals are horizontal, thus showing as inner longitudinal and outer round layers in cross section. These smooth muscle layers are contiguous with the sleek muscle covering the minor renal calyces, where the pacemaker is positioned to initiate the rhythmic peristalsis to deliver urine. The outermost layer, the adventitia, consists of a dense network of collagen and elastic fibers, together with many blood vessels and unmyelinated nerve fibers among them. Endoscopic Anatomy of the Ureter and Pelvicalyceal System Once the cystoscope is inside the bladder neck, the trigone can be seen as a raised, clean triangle. The apex of that triangle is situated on the bladder neck, and its base is formed by the interureteral ridge or Mercier bar, extending between the 2 ureteric orifices. The interureteral ridge is more outstanding in males than females, and the ureteric orifices are symmetrically located alongside it, roughly 1 to 2 cm from the midline. The trigone is probably the most vascular a part of the bladder and is fashioned by an extension of the longitudinal muscle fibers of the ureters over the detrusor muscle. Therefore it appears cystoscopically to be extra deeply colored than the remainder of the bladder. However, it could seem like a slit that might be identified with solely meticulous examination. It is pushed out laterally throughout bladder filling and should differ in place and appearance. In a normal bladder, the ureteric orifices are often surrounded by prominent mucosal vessels (Bagley et al. The ureteric orifices are categorized according to their place or configuration. However, they might be situated on the lateral wall of the bladder or at its junction with the trigone (position C) or in between positions A and C (position B) (Lyon et al. In phrases of configuration, grade zero signifies a standard ureteric orifice that looks like a cone or a volcano. Grades 1, 2, and three describe stadium, horseshoe, and golf-hole orifices, respectively. The intramural ureter represents the narrowest a half of the ureter, with an average diameter of 3 to 4 mm. Being the narrowest ureteral segment, the intramural ureter could have to be dilated before ureteroscopy. The pulsating iliac vessels could be seen endoscopically as the ureters cross the pelvic brim and angulate posteriorly within the proximal portion. Therefore, during ureteroscopy, the tidal volume could be decreased to minimize renal excursions during respiration. Moreover, the physiologic ureteral contractions or peristalsis may be noticed endoscopically. It is essential to wait for the ureter to relax before pushing the ureteroscope to keep away from mucosal trauma (Andonian et al. An extrarenal pelvis is usually larger and has longer major calyceal infundibula than an intrarenal pelvis. In the renal pelvis, the flexible ureteroscope first faces the ostia of the most important calyces, which look like round openings separated by carinae. Then the flexible ureteroscope enters a long tubular infundibulum that branches into the minor calyces. For a versatile ureteroscope to move from the axis of the higher ureteral section to the axis of the decrease infundibulum, it ought to deflected 140 (104 to 175) levels at the ureteroinfundibular angle (Bagley and Rittenberg, 1987). A round muscle layer extends around the base of the papilla to assist expel urine jets from papillary ducts. The renal papillae seem endoscopically as protruding discs surrounded by calyceal fornices, paler in color than the pink friable epithelium masking the papillae.
Buy benadryl 25 mg onlineTerakawa T, Miyake H, Muramaki M, et al: Risk components for intravesical recurrence after surgical administration of transitional cell carcinoma of the higher urinary tract, Urology 71(1):123�127, 2008. Varela-Duran J, Urdiales-Viedma M, Taboada-Blanco F, et al: Neurofibroma of the ureter, J Urol 138(6):1425�1426, 1987. Yang M-H, Chen K-K, Yen C-C, et al: Unusually high incidence of upper urinary tract urothelial carcinoma in Taiwan, Urology 59(5):681�687, 2002. Yoo S, You D, Song C, et al: Risk of intravesical recurrence after ureteroscopic biopsy for upper tract urothelial carcinoma: does the situation matter Zigeuner R, Tsybrovskyy O, Ratschek M, et al: Prognostic impact of p63 and p53 expression in higher urinary tract transitional cell carcinoma, Urology 63(6):1079�1083, 2004. Xylinas E, Rink M, Margulis V, et al: Multifocal carcinoma in situ of the higher tract is related to excessive danger of bladder most cancers recurrence, Eur Urol 61(5):1069�1070, 2012. Generally the tumor is biopsied and the therapy is contingent on the patient components together with the biopsy outcomes. Percutaneous entry to the renal pelvis and antegrade ureteroscopy may be required for diagnosis or therapy; examples include sufferers with urinary diversion. Because of the small dimension and shallow depth of ureteroscopic biopsy specimens, a precise correlation with eventual tumor stage is troublesome. Therefore, in predicting the tumor stage, a combination of the radiographic studies, the visualized appearance of the tumor, and the tumor grade provides the surgeon with the most effective estimation for risk stratification. In the previous, treatment suggestions had been primarily based, a minimum of partly, on practical limitations in follow-up and detection of native illness recurrence. Technologic improvements in imaging and, most important, direct endoscopic visualization of all ranges of the urinary tract enable earlier and extra accurate initial analysis and remedy and improved follow-up. Treatment could additionally be primarily based totally on the danger the tumor poses and on the efficacy of a selected treatment quite than on other issues. The least invasive remedy essential for protected management of the tumor is most popular, however by no means at the threat of compromising oncologic management. Thus laparoscopic surgery is ideal, a minimal of for the renal portion of radical nephroureterectomy when the tumor warrants elimination of the whole renal unit. A number of approaches with varied mixtures of laparoscopic and open techniques are employed for distal ureterectomy. Select low-grade noninvasive upper tract tumors may be managed initially by ablative renal-sparing surgical procedure. Retrograde ureteroscopy and ureteropyeloscopy are most well-liked when tumor size, quantity, and access enable full tumor ablation. All patients with low-risk disease must be considered for kidneysparing remedy regardless of the contralateral kidney due to the decrease morbidity of the procedures with out compromising oncologic outcomes. Kidney-sparing surgical procedure can also be considered in select sufferers with higher-risk situations similar to (1) severe renal insufficiency, (2) solitary kidney, (3) bilateral tumors, and/or (4) poor surgical candidate. Certainly the therapy chosen should not significantly compromise oncologic outcomes. The risks of most cancers management have to be weighed in opposition to the preservation of renal perform. In situations of high-grade disease, segmental resection must be thought-about over endoscopic management, which can only reliably treat surface tumors (Seisen, 2016). Radical Nephroureterectomy Indications Radical nephroureterectomy with excision of a bladder cuff is the gold normal for giant, high-grade, suspected invasive tumors of the renal pelvis and proximal ureter (Babaian and Johnson, 1980; Batata and Grabstald, 1976; Cummings, 1980; McCarron et al. Nephroureterectomy is among the few multi-quadrant operations that urologists perform with a wide range of approaches. Care should be taken to guarantee full removing and to keep away from harm to the contralateral ureteral orifice. Unless a midline incision is used, an additional Gibson, low midline, or Pfannenstiel incision is necessary for bladder cuff removal. In male sufferers the genitalia are included within the surgical field in order that the bladder catheter may be accessed in the course of the procedure. The midline strategy provides probably the most optimum exposure to the retroperitoneal lymph nodes and bladder. This incision, nonetheless, could additionally be limiting in exposure of the higher pole of the left kidney, particularly in obese patients. After the white line of Toldt is incised, the ipsilateral colon is mobilized to expose the Gerota fascia.
Purchase benadryl 25 mg with mastercardRecurrence of the urothelial most cancers in the higher urinary tract after the treatment of a bladder tumor takes place in 2% to 4% of the bladder cancer circumstances with a mean interval of 70 months (Herr et al. Nevertheless, these circumstances may be associated to renal insufficiency, which undermines the function of the conservative remedy. The degree of scarring of renal papillae seen in phenacetin abuse has been correlated in a dose-dependent method with the chance of excessive tumor grade and development. Moreover, the event of squamous carcinoma of the renal pelvis has been reported in calcified renal papillae after analgesic abuse (Stewart et al. The widespread metastatic sites are the lungs, liver, bones, and regional lymph nodes. The thin muscle layer of the renal pelvis and ureter may enable for an earlier involvement of surrounding tissue in comparability to the bladder cancer (Cummings, 1980; Richie, 1988). The renal parenchyma may serve as a barrier to the distant unfold of renal pelvis tumors of T3 stage, whereas the periureteral spread is said to a high danger for dissemination of the disease along the periureteral vascular and lymphatic provide. Improved survival of patients with stage T3 renal pelvis tumors versus ureteral tumors has been reported by a number of investigators (Batata and Grabstald, 1976; Guinan et al. This remark was additionally reported from a sequence of 611 patients treated at ninety seven hospitals (Guinan et al. The 5-year survival rates for sufferers with stage T3 tumors of the renal pelvis and ureter had been 54% and 24%, respectively. In a multivariate evaluation, sufferers with ureteral tumors had the next native and distant failure fee than did these with renal pelvis tumors of the identical stage and grade (Park et al. Some have proposed subclassification of renal pelvis tumors into pT3a for infiltration of the renal parenchyma and pT3b Chapter 98 for invasion of peripelvic adipose tissue, because the patients with pT3b have an increased risk of recurrence (Roscigno et al. Optimal tumor staging is achieved by lymph node dissection at the time of radical nephroureterectomy (Lughezzani et al. Depending on the stage and grade of the tumor, up to 40% of patients seem to harbor lymphatic metastases. In a study of sufferers who underwent lymphadenectomy on the time of radical nephrectomy, lymph node density of 30% or extra was associated with poor scientific outcomes (Bolenz et al. Urothelial Tumors of the Upper Urinary Tract and Ureter 2197 Surgical Margins the presence of constructive delicate tissue surgical margin after radical nephroureterectomy has been established as a major factor for developing illness recurrence. When the stage is larger than 2, pathologists ought to examine for and report positive margins on the degree of ureteral transection, bladder cuff, and around the tumor (Colin et al. Current proof is sufficient for the introduction of any of the markers within the day by day medical follow. Microsatellite instability and hypermethylation are rising as key differences between higher and lower tract urothelial tumors. Comparative genomic hybridization confirmed concordance between tumors of the renal pelvis and bladder within the losses at 2q, 8p, 9q, 11p, 13q, 17p, and 18q, and positive aspects at 1q, 6p, 8q, and 17q chromosomes (Rigola et al. Cytogenetic alterations such as +1p36, +6p22, +7, +8q22, -9p21, +11q, -13q, +17,+19q13, and +20q were noted (Zhang et al. Microsatellite instability has been related to an inverted development sample of cancer. A urine-based assay testing for a total panel of 77 markers for microsatellite instability was evaluated in 30 sufferers. Testing for microsatellite instability on resected tumor and normal tissues to display screen for Lynch syndrome is a well-established device for colon most cancers. When the stage and grade had been thought of within the multivariate analysis, no such correlation was confirmed (Zigeuner et al. Expression of Bcl-2 and survivin correlates with advanced cancers, and ranges of survivin are related to disease-specific survival (Jeong et al. Overexpression of Ki-67 has been related to development, decreased disease-specific survival (Jeon et al. On multivariate analysis it outperformed stage and lymph node standing as a predictor of survival (Ohtsuka et al. Snail contributes to the epithelial-mesenchymal transition in cell differentiation. Its overexpression was related to the presence of vascular invasion and recurrence (Scarpini et al. For preoperative choice making, there are two models within the preoperative setting. One of those nomograms is based on solely four variables and was reported to have excessive prognostic accuracy and threat stratification for patients with high-grade urothelial carcinoma of the higher urinary tract after extirpative surgery (Krabbe et al.
|