|
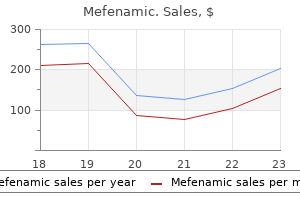
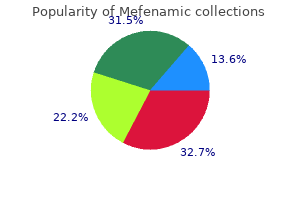
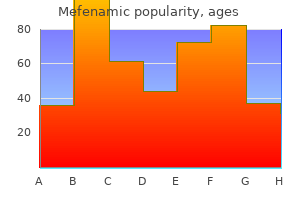
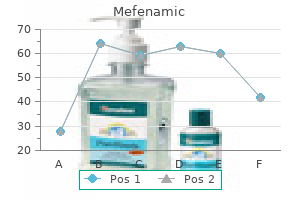
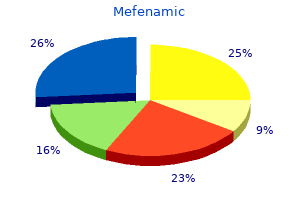
Mefenamic dosages: 500 mg, 250 mg
Mefenamic packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Order mefenamic 250 mg amexTo avoid critical damage the blade of the retractor must not apply traction to the nerve, roots or the brachial plexus. The smallest scalene muscle, if it exists, is divided off the Sibson fascia and the C7 transverse process. The middle scalene muscle is dissected and divided with scissors on the highest stage possible, with a right-angled clamp positioned to hook the muscle. The lengthy thoracic nerve posterior to the center scalene muscle should be recognized and carefully protected. The first rib resection is carried out in an extraperiosteal fashion, except in areas the place the vein or artery may be adherent to the periosteum and prone to tearing, the place subperiosteal dissection is required. The first rib is then freed circumferentially by the periosteal elevator and a blunt-tip right-angled clamp anteriorly and posteriorly With a Roos nerve. A large-angled bone rongeur is used to trim the anterior remaining end of the rib to the sternal joint. The posterior stump of the first rib is additional truncated near the transverse process using a box-shaped bone cutter. Any sharp bony fragments should be recognized with visual inspection or palpation and eliminated. Any further delicate tissue bands crossing the brachial plexus nerve roots are sought and thoroughly divided. The remaining anterior and middle scalene muscular tissues are trimmed further until the stumps are above the neurovascular bundle. A drainage tube connected with closed suction is introduced out via a separate stab wound below the incision. After closure of the subcutaneous tissue, the skin is closed using monofilament polypropylene suture with cosmetic surgery technique. During the efficiency of this operation, sufficient lighting and visualization must be maintained due to the configuration and depth of the operative area. Cautery must not be used after reaching the first rib to avoid injuring the neurovascular buildings. This strategy permits fast exposure of the primary rib without much manipulation of the subclavian vessels or brachial plexus. The incision itself is cosmetically appealing and allows for speedy restoration and most patients depart the hospital on the first postoperative, day Many teams have used this procedure with short- and long-term success. Visualization is thru a long axillary tunnel that have to be adequately lighted to prevent injury which, 43 happens most commonly to the axillary vein or T1 nerve root. A supplementary light source from a headlight is indispensable, and a fiber-optic lighted retractor is paramount for the protected conduct of this operation. Recent addition of high-definition videoendoscopy to assist visualization indicate a significant advance. Supraclavicular Scalenectomy With or Without Rib Resection Procedures carried out via a supraclavicular method embrace anterior and center scalenectomy alone or combined with first rib resection. A simple scalenectomy has been advocated by some and requires division of the muscle close to its origin at the cervical transverse processes. An incision is made within the supraclavicular space approximately 1 to 2cm above and parallel to the clavicle between the interior and exterior jugular veins. Subplatysmal flaps are constructed, and the clavicular head of the sternocleidomastoid may be divided if wanted. The scalene fats pad is mobilized laterally to expose the anterior facet of the anterior scalene muscle and the associated phrenic nerve. It must be dissected away from the anterior scalene muscle by incising the epimysium and connective tissues, which bind these collectively. The apply of inserting a vessel loop around the phrenic nerve to mark its location is controversial because this maneuver might by itself render the nerve more weak. Next, the muscle is transected at a degree near the insertion onto the primary rib, with care to keep away from injuring the underlying subclavian artery the scalene muscle is mirrored.
Mefenamic 500 mg genericAfter the hemodynamics have been corrected, then native wound care is required for pores and skin closure and therapeutic, and after skin healing happens, the leg have to be protected to forestall the recurrence of superficial ambulatory venous hypertension and eventual reulceration. With our current understanding of persistent venous disease, a compliant patient, and facility with the many remedy options presently available, most sufferers with venous leg ulcers can both heal them and keep healing. The finest screening test for patient with a venous ulcer to determine the therapy choices is: a. The therapy of iliac venous stenosis or occlusion by stenting must be performed: a. Patients who bear ablation of an incompetent saphenous vein for a nonhealing venous ulcer will: a. Endovenous ablation of the saphenous vein for prevention and therapeutic of venous ulcers. Incidence and Risk Factors for iliocaval venous obstruction in patients with lively or healed venous leg ulcers. Gelabert Portal hypertension and variceal hemorrhage are necessary scientific issues in which vascular surgeons may still have a big interest and concern. New developments have altered the once-familiar strategy to this disease, with endoscopic and endovascular approaches having replaced what was as quickly as treated predominantly with open surgical procedures. Orthotopic liver transplantation has also become an important part in treating this disease in appropriately chosen patients. For a surgeon to have a role in treating these sufferers, it is necessary to understand the underlying liver disease, the pathophysiology of portal hypertension, and the alternative administration choices for variceal hemorrhage and portal hypertension. Definition Portal hypertension is a condition in which the traditional circulation of blood within the portal venous system is impeded, resulting in a rise in portal venous strain. Elevation of the portal venous blood pressure leads to a sequence of physiologic alterations, together with ascites, hypersplenism, and variceal hemorrhage. Clinically significant portal hypertension exists when the portal stress is elevated more than 10mmHg above systemic pressure in the inferior vena cava (corrected portal pressure). The natural historical past of patients with portal hypertension differs, relying on the cause of the condition and the stage of presentation. Pathogenesis Physiologically portal hypertension results from both an increase in the portal blood, circulate (rare) or an obstruction to the outflow of blood from the portal circulation (common). Obstructions to the portal circulation have been categorized anatomically based on their location relative to the hepatic sinusoids. Accordingly the obstruction could additionally be, presinusoidal, sinusoidal, or postsinusoidal. Presinusoidal and postsinusoidal obstructions have been subclassified as intrahepatic or extrahepatic (Box 55. Although much less common than other types of obstructive portal hypertension, portal vein thrombosis happens in a major variety of youngsters and also can happen in adults, though the causes are remarkably completely different between youngsters and adults. Portal vein thrombosis in children most commonly happens as a complication of an infectious course of similar to omphalitis and appendicitis, whereas in adults, the most typical cause of portal vein thrombosis is a gradual and relentless decrease in the portal blood move secondary to the high resistance in the hepatic circulation attributable to cirrhosis. Other causes in adults embrace pancreatitis, hypercoagulable states or tumor thrombus, and mechanical obstruction of portal venous circulate. The last may be the outcomes of malignant invasion, lymphadenopathy or caudate lobe compression. Hypercoagulable, situations might result from polycythemia, cancer, or hypovolemia. Sepsis can even result in portal vein thrombosis by a number of mechanisms: low-flow states, hypovolemia, and activation of the coagulation system. Intrahepatic Presinusoidal Obstruction Most causes of intrahepatic presinusoidal obstructive portal hypertension relate to fibrosis and compression of the portal venules, with subsequent restriction of portal circulate. Included among these diseases are congenital hepatic fibrosis, sarcoidosis, continual arsenic publicity, Wilson illness, hepatoportal sclerosis, main biliary cirrhosis, schistosomiasis, and myeloproliferative issues. Schistosomiasis is the most common explanation for portal hypertension in third-world nations. Deposition of ova in the portal vein walls results in a granulomatous inflammatory response, which in flip leads to fibrosis and portal move restriction.
Buy mefenamic 250mg lowest priceWarfarin remedy is associated with an elevated risk of hemorrhagic issues. There are five direct thrombin inhibitors at present out there for clinical use: lepirudin, desirudin, bivalirudin, argatroban, and dabigatran. In addition, thrombin serves many different roles, together with the activation of various coagulation elements, platelets, smooth muscle cells, fibroblasts, and endothelium. Hirudin, the primary direct thrombin inhibitor, was originally isolated from the salivary gland of the medicinal leech (Hirudo medicinalis) after it was famous that leech saliva had anticoagulant properties. Argatroban is a synthetic, small-molecule arginine by-product that interacts solely with the active website of thrombin. Melagatran and Ximelagatran (its prodrug) had been the primary oral direct thrombin inhibitors. Although preliminary research had been promising for using Ximelagatran, it has since been removed from medical investigation due to significant hepatotoxicity. They have comparatively brief half-lives, and their effect can therefore be interrupted with missed doses. Dabigatran etexilate is an artificial, nonpeptide, direct thrombin inhibitor that inhibits both circulating and clot-bound thrombin and lowers thrombin-stimulated platelet aggregation. Idarucizumab is a just lately approved reversal agent reversal agent for dabigatran to be used in circumstances such as life-threatening bleeding and emergency surgery sixty nine. Co-administration of dabigatran with different P-glycoprotein transporter substrates such as Rifampin decreases serum concentrations of dabigatran and should decrease its effectiveness. Fondaparinux has been evaluated in multiple trials for stopping deep venous thrombosis in patients present process main hip fracture and knee alternative surgical procedure 80-83. Peak serum focus occurs in 2 to four hours, and it has a half-life of 7 to 11 hours. One-third of the active metabolite is renally excreted, and two-thirds is hepatically metabolized by the cytochrome P450 pathway Strong inhibitors or inducers of the cytochrome P450 pathway can subsequently. Rivaroxaban can be orally administrated, a few times daily, without any monitoring or want for dose adjustment. It is contraindication in extreme liver insufficiency and not recommended in sufferers with severe renal impairment. Adverse reactions with rivaroxaban are associated to bleeding, though they might in reality be decrease than with other anticoagulants. Epidural and spinal hematomas are related to the use of rivaroxaban during neuraxial anesthesia or spinal puncture. As with other agents with this mechanism of action, edoxaban has been associated with an increased danger of bleeding. Idarucizumab is a humanized monoclonal antibody fragment that selectively binds to the energetic web site of dabigatran and its acylglucuronide metabolites, thereby inhibiting their exercise It has an affinity for the active site of dabigatran 350 occasions higher than that of. Once sure, it remains connected to dabigatran, blocking its exercise till the drug may be metabolized. Administration of idarucizumab resulted in full reversal of the effects of dabigatran in 89% of topics. In both teams, the median maximum reversal of the results of dabigatran was 100 percent, with 89% of sufferers achieving full reversal. Reversal of the consequences of dabigatran exposes sufferers to the thromboembolic threat of their underlying medical situation. Hypersensitivity reactions, together with pyrexia, bronchospasm, hyperventilation, rash, and pruritus, have also been reported. The recommended dose of idarucizumab incorporates 4g of sorbitol; therefore individuals with hereditary fructose intolerance are vulnerable to antagonistic events, including demise, after administration of idarucizumab. It is a recombinant derivative of issue Xa, which has been designed to have a better affinity for factor Xa inhibitors than naturally occurring issue Xa. Phase 2 medical trials of the drug had been completed in 2015 and demonstrated that intravenous administration of andexanet resulted in dose-dependent, speedy, and reproducible reversal of anticoagulant results of apixaban, rivaroxaban, edoxaban, and enoxaparin in wholesome volunteers without proof of antagonistic effects.
Order mefenamic 500 mgTherefore the improved survival within the sclerotherapy group really represents a mixture of sclerotherapy and surgical therapy Teres and colleagues204 discovered no difference in early. In 1989, Burroughs and associates206 concluded a prospective, randomized study comparing staple transection with sclerotherapy for emergency control of variceal bleeding. They discovered no distinction in general mortality and improved management of bleeding with esophageal transection compared with a single injection, but there was an identical incidence of hemorrhage after three injection therapies. Teres and colleagues207 randomized cirrhotic patients with uncontrolled bleeding to portacaval shunt or staple transection in low-risk patients and staple transection or sclerotherapy in high-risk patients. In the low-risk sufferers, portacaval shunt had a larger hemostatic impact however a greater incidence of encephalopathy In high-risk. The authors due to this fact recommended staple transection for low-risk patients and sclerotherapy for the initial administration of high-risk sufferers. Although a consensus has not but been reached, sclerotherapy may symbolize an acceptable various ablative process in selected sufferers with hepatic dysfunction. In comparability research, the charges of efficacy in halting bleeding are comparable between the 2 techniques. There is debate whether or not the incidence of complications with banding is lowered compared with sclerotherapy Clearly the identical major issues attend both. Because of the high mortality related to emergency shunting procedures, variceal sclerotherapy along side octreotide is indicated in the acute management of variceal hemorrhage. Special variations are carried out due to the underlying hepatic illness and the associated dangers. Nasogastric tubes have to be placed in all sufferers; if blood is present in the stomach, then gastric lavage and emergency endoscopy are indicated. This permits verification of the source of the hemorrhage and emergent sclerotherapy if required. Treatment with fluids and blood merchandise ought to be directed at sustaining enough tissue perfusion. If the affected person fails to stop bleeding after injections and balloon tamponade, emergent intervention is indicated. Once bleeding is controlled, sufferers with comparatively good hepatic operate (Child class A or B) should endure long-term sclerotherapy until varices are obliterated. If that is successful, the patient should continue to be noticed, and no further intervention need be deliberate. If the affected person has breakthrough bleeding from noncompliance, gastric varices, or hypertensive gastritis and is an appropriate candidate for an elective shunt, a preoperative analysis must be accomplished (angiography duplex scan) and a shunt is, carried out. Patients with poor hepatic operate should be thought-about for transplantation if they meet the suitable standards. While the affected person is awaiting orthotopic liver transplantation, a peripheral shunt may be needed as a bridge. Child class C sufferers with marked muscle losing and obvious hyaline necrosis have a prohibitively high operative mortality fee and will bear endoscopic sclerotherapy adopted by transplantation. Management of Ascites Ascites predisposes portal hypertensive sufferers to probably deadly issues, including renal failure, peritonitis, variceal hemorrhage, pleural effusions with respiratory insufficiency belly wall hernias, anorexia, and generalized malaise. In, most sufferers, ascites could be controlled with a restricted-salt food regimen and a diuretic regimen. However, a subgroup (5% to 10%) of ascites sufferers have refractory ascites, and that is related to increased mortality 215 Treatment options for these patients embody. Paracentesis can be an effective technique notably when large quantity paracentesis may be tolerated. Although rarely performed, peritoneovenous shunting can additionally be used for the remedy of ascites. It is managed by a one-way valve so that a stress gradient of 5cm H2O suffices to transfer the ascitic fluid from the abdomen to the intravascular house. The Denver shunt, a variation of the LeVeen shunt, incorporates a pump in line with the shunt and is implanted into the subcutaneous tissues within the chest wall. Its proposed profit is the flexibility to clear the shunt of debris by using the pump mechanism. Summary the administration of portal hypertension and its sequelae of ascites, encephalopathy and, recurrent variceal hemorrhage continue to be significant challenges to clinicians. Alcoholic cirrhosis resulting in intrahepatic sinusoidal and postsinusoidal obstruction continues to be the most typical trigger.
Discount 500 mg mefenamic fast deliveryIndolent, persistent ischemic shows with evidence of microembolization, Roth spots, splinter hemorrhages, or digital ulceration might not require emergent revascularization and should enable more time for diagnostic analysis. Imaging Modalities Radiography ought to be accomplished in circumstances of higher extremity acute arterial occlusion to consider the presence of a cervical rib. Noninvasive testing with duplex ultrasound is mostly used to affirm the arterial occlusion and to help set up the extent of arterial thrombosis. Catheter-based angiography permits for diagnosis of aneurysm, stenosis, or occlusion. In the event of acute upper extremity ischemia, the diploma of ischemia and extent of thrombosis want be considered in electing thrombolysis versus open thrombectomy. This lesion is best repaired by reverse vein grafting, with care being taken to keep away from entrapment of brachial plexus components. In sufferers with profound acute limb ischemia, surgical thrombectomy could also be preferable. Once arterial perfusion is restored, imaging is required to determine the source of thromboembolism. Careful evaluation of the entire upper extremity arterial tree should be accomplished with the precise intent to assess the most typical sources of arterial embolization: the subclavian artery at thoracic outlet, the axillary artery across the humeral head, and the humeral circumflex arteries at the neck of the humerus. Imaging of the hand and digits is necessary to assess aneurysmal degeneration of the radial and ulnar arteries. Imaging of digital arterial arcades will usually provide evidence of chronic embolization. The typical findings of persistent embolization embody loss of one or each digital arteries, abrupt lack of arterial segments, and reconstitution of distal arterial segments. Typical findings include focal arterial deficits brought on by impingement on the thoracic outlet. Cervical spine imaging has a excessive chance of figuring out the presence of cervical ribs. Surgical targets are complicated: the embolic source is identified, and the underlying arterial lesion is repaired along with decompression of the thoracic outlet. Repair of the arterial lesions usually requires reconstruction of the subclavian artery. Usually decompression surgery, together with rib resection and scalenectomy should be performed later to scale back the danger of, hemorrhage. Vessels with aneurysmal adjustments or poststenotic dilation of greater than 2cm must be resected and reconstructed with autogenous saphenous vein or synthetic prosthesis utilizing the supraclavicular method with an infraclavicular incision. An arterial lesion less than 2cm may be left alone, and only rib resection and scalenectomy ought to be performed using the transaxillary method. Dorsal sympathectomy may be performed through the axillary incision or under thoracoscopic steerage. Generally excellent outcomes, 83,84 can be expected with timely diagnosis and treatment. Vascular Disease of the Upper Extremity the upper extremities are subject to quite a lot of unique intrinsic arterial and venous issues, as properly as the peripheral manifestations of systemic collagen vascular ailments. Patients creating arterial insufficiency of the upper extremities typically show considered one of three totally different scientific patterns: (1) attacks of Raynaud disease symptoms, (2) digital ischemia and gangrene, or (3) crampy pain with exercise, usually referred to as claudication. The preliminary examination of the upper extremity should start with inspection, palpation, and auscultation. Noninvasive vascular testing, similar to segmental systolic stress measurement with Doppler move detector, digital plethysmography and duplex, scan, can be used to further document the dysfunction. Afflictions of the Major Vascular Structures Approximately 50% of cases of acute arterial insufficiency of the upper extremity are secondary to embolization; of the remainder, 25% are the end result of main arterial thrombosis and 25% are iatrogenic in origin, including arterial blood stress monitoring, sampling of arterial blood gases, and creation of an arteriovenous fistula for dialysis. Brachial artery catheterization is a well-documented cause of higher extremity ischemia. The vast majority of embolic arterial occlusions in the upper extremity are of cardiac origin, however brachiocephalic aneurysmal illness sometimes leads to embolic episodes.
Discount 250mg mefenamic with visaA smaller patient group treated by rheolytic thrombectomy was reported by Kasirajan and associates,25 who demonstrated that mechanical thrombectomy alone was less effective than the mixed pharmacomechanical approach. The efficacy of high-pressure supply of the plasminogen activator solution into the thrombus was reported by Chang and colleagues. Following the pulse-spray infusion, the catheter was eliminated and the patient returned to their hospital room. Patients had repeat venograms the following day and extra pulse spray infusion if indicated. Significant or complete lysis was observed in 92% (11/12), with the remaining patient having 50% to 70% lysis. Bookstein and colleagues27 reported the good factor about forceful pulse-sprayed plasminogen activator in thrombosed arteries and dialysis entry grafts. This calls consideration to the importance and effectiveness of the plasminogen activator penetrating the thrombus and of the plasminogen activator penetrating the thrombus and binding to fibrin-bound plasminogen with subsequent production of intrathrombus plasmin. Complete lysis (90%) was noticed in 70% of sufferers and total lysis (complete or partial) in 91%. The median infusion time was 22 hours, and 4% of sufferers had main complications, which were basically puncture web site hematomas. Engelberger and his colleagues from Bern, Switzerland carried out the "Bernutiful Trial" designed to answer the question, "Does intravascular high frequency low energy, ultrasound facilitate decision of thrombus throughout catheter-directed thrombolysis The study end level was the quantity of thrombolysis at 15 hours assessed by readers blinded to the treatment group. Between these two balloons, a plasminogen activator is infused and a dispersion wire causes the intraballoon section of the catheter to assume a spiral configuration. Liquefied and fragmented thrombus can be aspirated and remedy success evaluated by repeat segmental phlebography If thrombus is resolved, the catheter is repositioned and additional. If residual thrombus persists, a second treatment is performed or repeat remedy of another applicable intervention (rheolytic thrombectomy balloon angioplasty stenting) is carried out. Venoplasty and stenting had been used to appropriate underlying stenoses, and all received longterm therapeutic anticoagulation. There was an inclination toward more full thrombus decision with the pharmacomechanical techniques. The finest predictor of reflux within the treated limb was reflux within the contralateral, uninvolved limb. Eighty-six % of sufferers at 6 years had patent veins and usually functioning valves. The greater the quantity of residual thrombus, the worse the postthrombotic syndrome as measured by the validated Villalta scale. Patients who had 90% or extra clot decision primarily had no postthrombotic morbidity. This was studied by Aziz and colleagues,35 who reported that residual thrombus at the end of lysis correlated with recurrence. Patients with more than 50% (mean 65%) residual clot had a considerably higher recurrence price than sufferers with lower than 50% (mean 16%) thrombus remaining. It seems evident that residual thrombus is largely liable for recurrent thrombosis. Pharmacomechanical methods have increased treatment success, decreased remedy time, and lowered dose of plasminogen activator. All sufferers were handled with normal therapeutic anticoagulation and received 30 to 40mmHg ankle-gradient compression stockings. Objective evaluation of vein patency and venous valve perform had been carried out with venous duplex examinations. All however one major bleed occurred in sufferers over 65 years, and one hundred pc of main bleeds occurred in sufferers >60 years of age. Important extra analyses are underway that may help physicians on properly selecting sufferers for methods of thrombus removal and counseling patients on what to anticipate from outcomes of treatment.
Purchase mefenamic 250 mg amexA 10-year-old boy with a historical past of omphalitis experiences his first episode of variceal hemorrhage. Specific contraindications to peritoneovenous shunts include all of the following besides: a. Technical considerations in favor of performing a distal splenorenal shunt embody which of the next Percutaneous transhepatic coronary vein occlusion is related to a 20% portal vein thrombosis rate. What is the commonest site of obstruction inflicting portal hypertension within the Western world A 40-year-old man with cirrhosis is set to be Child class A; his bleeding has been managed with sclerotherapy and vasopressin. The measurement of hepatic blood move and intrahepatic shunted blood circulate by colloid, warmth denatured serum albumin labeled with I131. Late effects of portal systemic shunting procedures on cardiorespiratory dynamics in man. Selective surgical therapy of the Budd-Chiari syndrome supplies superior survival rates than conservative medical management. Pulsed Doppler flow as a criterion of portal venous velocity: comparison with cineangiographic measurements. Ultrasonography in the analysis of portal hypertension: diminished response of portal vessels to respiration. Portal hypertension, size of esophageal varices and threat of gastrointestinal bleeding in alcoholic cirrhosis. Prophylactic endoscopic sclerosing treatment of the esophageal wall in varices-a prospective managed randomized trial. Prophylactic endoscopic sclerotherapy of esophageal varices: a prospective managed study Lancet. Prediction of the primary variceal hemorrhage in sufferers with cirrhosis of the liver and esophageal varices: a potential multicenter trial. Emergency endoscopy after gastrointestinal hemorrhage in 50 sufferers with portal hypertension. Nitroglycerin improves the hemodynamic response to vasopressin in portal hypertension. Hemodynamic effects of vasopressin alone and together with nitroprusside in sufferers with liver cirrhosis and portal hypertension. A randomized trial of vasopressin and vasopressin plus nitroglycerin in the control of acute variceal hemorrhage. Comparison of intravenous somatostatin and vasopressin infusions in treatment of acute variceal hemorrhage. Effects of somatostatin on hepatic and systemic hemodynamics in patients with cirrhosis of the liver: comparability with vasopressin. Review article: the position of pharmacotherapy for acute variceal hemorrhage within the era of endoscopic hemostasis. Emergency sclerotherapy versus vasoactive drugs for bleeding oesophageal varices in cirrhotic sufferers. Controlled trial of propranolol for the prevention of recurrent variceal hemorrhage in patients with cirrhosis. Prevention of recurrent bleeding in cirrhotics with latest variceal hemorrhage: potential randomized comparability of propranolol and sclerotherapy Hepatology. Propranolol for prevention of recurrent gastrointestinal bleeding in sufferers with cirrhosis. Gastrointestinal bleeding after abrupt cessation of propranolol administration in cirrhosis. Propranolol for prevention of recurrent gastrointestinal bleeding in sufferers with cirrhosis: a prospective research of factors associated with rebleeding. Ligation versus propranolol for the primary prophylaxis of variceal bleeding in cirrhosis. Endoscopic variceal band ligation in contrast with propranolol for prophylaxis of first variceal bleeding.
|