|
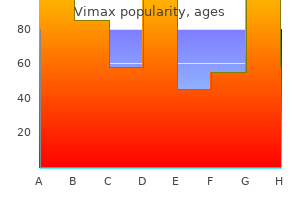
Vimax dosages: 30 caps
Vimax packs: 1 bottles, 2 bottles, 3 bottles, 4 bottles, 5 bottles, 6 bottles, 7 bottles, 8 bottles, 9 bottles, 10 bottles

Buy 30 caps vimax fast deliveryIt starts getting vascularized by formation of recent blood vessels-vasculogenesis in zone of calcification, and as it gets Then because the chondrocytes are eroded, new cells appear-the bone cells creating zone of ossification. It is obvious that at epiphyseal development plate, the cartilage will get destroyed and changed by bone in a gradual manner. Erosion of bone maintain happening by the osteoclast cells, which help in enlarging the marrow cavity. Table 12: Review of skeletal tissues Structure Key components and features Cartilage Hyaline cartilage: most common sort, varieties articular surfaces of synovial joints, function in development of bony skeleton. Features intermediate between hyaline cartilage and dense common connective tissue. Bone Major supporting tissue of the skeleton, composed of cells surrounded by collagenous osteoid matrix which is mineralised by calcium hydroxyapatite deposition. Osteoblasts: on surface of bony trabeculae, synthesise new osteoid, turning into entrapped by this and then named osteocytes. Fine canaliculi inside the bone include interconnecting cytoplasmic processes from the cells. Osteoclasts: giant multinucleate cells, lie in small depressions known as Howship lacunae, involved resorption and remodelling of bone. Woven bone: that is immature bone with randomly oriented collagen fibers, discovered during development, associated with healing and repair, remodelled into lamellar bone. Lamellar bone: this is mature bone by which the collagen fibers are oriented in parallel arrays, aligned to face up to stresses on the skeleton. Cortical bone: parallel columns of bone (osteons) with concentric lamellar round central Haversian canals containing neurovascular bundles Cancellous bone: interconnecting community of bony struts with intervening bone marrow. Two types of bone growth: intramembranous ossification (mainly cranium bones) and endochondral ossification (bone forms on a template of hyaline cartilage). Synovial joints (diarthroses): allow extensive movement between articular surfaces. Surfaces lined by hyaline cartilage, fibrous capsule lined by synovium, lubricated by synovial fluid. Non-synovial joints: restricted motion, bones united by dense collagenous tissues, including dense fibrous tissue (syndesmosis), hyaline cartilage (synchronosis) or fibrocartilage (symphysis). Bands of dense regular connective t problem originating from muscle and inserting into bone to transmit the force of muscle contraction so that motion of joints could occur. The nutrient artery and the epiphyseal arteries enter the bone by way of nutrient foramina. These openings within the bone arise developmentally because the pathways of the principal vessels of periosteal buds. Metaphyseal arteries come up from periosteal vessels that turn into integrated into the metaphysis as the bone grows in diameter. It consists of hyaline cartilage C and is hooked up to the cortical bone B of the head of the femur. Both the glycosaminoglycans and collagen are synthesized and maintained by the chondrocytes. Hyaline cartilage covers the articular surface of synovial joints � Articular cartilage covers the articular surfaces of synovial joints, which is often of hyaline selection (with few exceptions). Fibrocartilage � Articular cartilage in temporomandibular joint is fibrocartilage (and not the usual hyaline variety). It has a rich nerve provide � Articular cartilage of typical synovial joints is devoid of nerves and blood vessels. Intervertebral disc � Costal cartilage and nasal septum contain hyaline cartilage. Epiphyseal plate � it is a slide of hyaline cartilage, which is found in development (epiphyseal) plate. Bone Table 15: Summary of bone varieties and their organization Types of bone Histological features Woven bone, newly calcified Irregular and random arrangement of cells and collagen; lightly calcified Lamellar bone, reworked Parallel bundles of collagen in skinny layfrom woven bone ers (lamellae), with often spaced cells between; closely calcified. Compact bone, ~80% of all Parallel lamellae or densely packed oslamellar bone teons, with interstitial lamellae Cancellous bone, ~20% of all Interconnected thin spicules or tralamellar bone beculae coated by endosteum Major locations Developing and growing bones; hard callus of bone fractures All normal areas of grownup bone Synonyms Immature bone; major bone; bone. All cells except osteoclasts originate from the mesenchymal stem cells, which differentiate into osteoprogenitor cells, osteoblasts, and eventually osteocytes and bone lining cells. Bone-lining cells on external bone surfaces are part of the periosteum, therefore the term periosteal cells.
Cheap vimax 30caps with mastercardEfficacy of fibrin sealant in the management of complicated anal fistula: a prospective trial. Adoption and success rates of perineal procedures for fistula-in-ano: a systematic evaluate. Treatment of fistula-in-ano with fistula plug � a evaluate under particular consideration of the method. Outcomes of major restore of anorectal and rectovaginal fistulas utilizing the endorectal advancement flap. Long-term analysis of the use of transanal rectal development flaps for sophisticated anorectal/ vaginal fistulas. Fibrin glue as an adjunct to flap repair of anal fistulas: a randomized, managed research. Dermal island-flap anoplasty for transsphincteric fistula-in-ano: evaluation of treatment failures. Ano-cutaneous flap restore for advanced and recurrent supra-sphincteric anal fistula. Anorectal problems: experience with primary fistulectomy for anorectal abscess, a report of 1,000 circumstances. The incidence of recurrent abscesses or fistula-in-ano following anorectal suppuration. Anorectal suppuration: the results of therapy and the factors influencing the recurrence price. Comparison between anal endosonography and digital examination in the evaluation of anal fistulae. Value of hydrogen peroxide enhancement of three-dimensional endoanal ultrasound in fistula-in-ano. Vaginal endosonography of the anal sphincter complex is essential in the assessment of faecal incontinence and perianal sepsis. Change in anal continence after surgery for intersphincteral anal fistula: a practical and manometric study. Microbiological evaluation and endoanal ultrasonography for analysis of anal fistula in acute anorectal sepsis. The ultimate evaluation and classification of the surgical therapy of the first anorectal cryptoglandular intermuscular 29. Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. Management of anal fistula by ligation of the intersphincteric fistula tract-a systematic evaluate. The anatomy of failures following the ligation of intersphincteric tract method for anal fistula: a evaluate of 93 sufferers over 4 years. Ligation of intersphincteric fistula tract versus mucosal advancement flap in patients with high transsphincteric fistula-in-ano: a potential randomized trial. Ligation of intersphincteric fistula tract compared with development flap for complex anorectal fistulas requiring preliminary seton drainage. Enteral vs parenteral nutrition in reconstructive anal surgery-a prospectiverandomized trial. Fistula-tract Laser Closure (FiLaC): long-term outcomes and new operative strategies. Closure of fistula-in-ano with laser-FiLaC: an effective novel sphincter-saving process for complex disease. A new technique for sphincter-preserving anal fistula restore using a novel radial emitting laser probe. Practice parameters for the remedy of perianal abscess and fistula-in-ano (revised). Clinical and microbiological characteristics of perianal infections in grownup patients with acute leukemia. Perianal infections in sufferers with leukemia: importance of the course of neutrophil rely.
Order 30 caps vimax with visaLow anterior resection syndrome rating: improvement and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Long-term anorectal dysfunction after postoperative radiotherapy for rectal most cancers. Bowel operate 14 years after preoperative short-course radiotherapy and whole mesorectal excision for rectal cancer: report of a multicenter randomized trial. Why do some patients expertise poor practical results after anterior resection of the rectum for carcinoma To avoid native recurrence, a full-thickness excision of the portion of the bowel wall concerned by the tumor, with a 1-cm adverse margin, is required. Prospective randomized trial comparing J colonic pouch-anal anastomosis and straight coloanal reconstruction. Functional end result after low anterior resection with low anastomosis for rectal cancer utilizing the colonic J-pouch. Prospective, randomized examine comparing clinical outcomes between small and huge colonic J-pouch following coloanal anastomosis. Functional and physiologic assessment of the colonic reservoir or side-to-end anastomosis after low anterior resection for rectal most cancers: a two-year follow-up. Impact of anastomotic leakage on long-term survival of sufferers undergoing curative resection for colorectal cancer. Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Defunctioning stoma in low anterior resection with colonic pouch for rectal most cancers: a comparability between two hospitals with a different policy. Defunctioning loop ileostomy for pelvic anastomoses: predictors of morbidity and nonclosure. The trendy abdominoperineal excision: the following problem after complete mesorectal excision. Perineal wound healing after abdominoperineal resection for rectal most cancers: a scientific evaluation and meta-analysis. Comparison of short- and longterm outcomes after extralevator abdominoperineal excision and standard abdominoperineal excision for rectal most cancers: a systematic evaluate and meta-analysis. Prone or lithotomy positioning during an abdominoperineal resection for rectal cancer leads to comparable oncologic outcomes. Randomized clinical trial evaluating laparoscopic and open surgery in sufferers with rectal most cancers. Incidence of minimally invasive colorectal cancer surgery at National Comprehensive Cancer Network facilities. Hybrid laparoscopic flexure takedown and open procedure for rectal resection is associated with considerably shorter length of stay than equivalent open resection. Robotic versus laparoscopic complete mesorectal excision for rectal most cancers: a meta-analysis. These platforms enable access to lesions positioned within the higher two-thirds of the rectum. Local excision of early rectal most cancers should supply remedy charges corresponding to radical surgical procedure with a objective of improved functional outcomes and decreased morbidity. Appropriate affected person selection is important, and each effort must be made to select patients with minimal threat of lymph node involvement for curative local excision. Lesions bigger than three cm may also be eligible for native excision but have poorer outcomes. Complete pathologic evaluation with substaging of T1 lesions using the Kikuchi classification is critical for correct threat stratification. Lesions that show invasion deeper than the primary third of the submucosa. Strict adherence to these criteria should lead to equal oncologic outcomes for local excision in contrast with radical surgical procedure. Comorbidities, capability to tolerate surgery, and reliability to undergo intensive surveillance must be considered.
Purchase vimax 30 caps on-lineAn incision is made in the posterior vaginal wall by the introitus, distal to the fistula. Adequate proximal width of the base of the flap is important to ensure good blood provide. The defect within the sphincter is oversewn with absorbable suture, and the flap is sutured down in sections with interrupted suture. This flap has the primary advantage of the usage of healthy, well-vascularized vaginal tissue, avoiding any scar or illness in the anal canal. This could additionally be an especially engaging option within the setting of anal stenosis or in sufferers with Crohn illness. In this process, the fistula is converted to a fourth-degree perineal laceration by dividing all the tissue between the rectum and vagina by way of the perineal body. Cloacal defects represent a extreme form of obstetric trauma with primarily no perineal body, a shortened rectovaginal septum, and a retracted anal sphincter. Repair is carried out by growing the aircraft between the anorectal and vaginal epithelium and figuring out the sphincter muscle on both sides, which is mobilized and subsequently approximated. Kaiser reported 12 sufferers with a cloacal defect who had been handled utilizing an X-flap anoplasty. With a fistula probe traversing the tract, dissection proceeds down within the intersphincteric house. A portion of the intersphincteric fistula tract is excised and the defect in the inner and external sphincter is sutureligated with absorbable suture. The intersphincteric area is then reapproximated with interrupted absorbable suture and the skin incision is closed with interrupted chromic. The restoration of anatomy and sphincter function has the advantage of an autologous tissue flap restore. A perineal incision near the anus is performed and the divided ends of the sphincter are identified and skeletonized laterally. Care should be taken to not prolong the perineal incision more than 180 degrees owing to the chance of injury to the pudendal nerve. The sphincter can also be dissected away from the anal mucosa and mobilized to the midline. The restore could be carried out as an endto-end approach or extra generally as an overlapping method. The overlapped muscle is sutured in place with 20 absorbable interrupted mattress sutures. When used within the context of an development flap, this has been shown to enhance the rate of fistula closure, as high as one hundred pc in one collection, and to restore continence in as many as 70% of patients. This approach employs the benefit of transposing healthy, well-vascularized tissue to buttress repair. It is often utilized in settings of failed previous repairs or within the setting of prior radiation. The mostly used muscle grafts are the bulbocavernosus and gracilis muscular tissues, although other grafts have been used, together with the sartorius and gluteus maximus. This approach may be combined with sphincteroplasty in the setting of known sphincter injury. The Martius flap, which involves harvesting of the bulbocavernosus muscle with the overlying fats within the labia majora, relies on the perineal branch of the pudendal artery. Five sufferers had dyspareunia (31%), whereas only one had complained of dyspareunia preoperatively. Dyspareunia, infrequently reported as an end result variable, is a possible concern with the process. The neurovascular pedicle enters the muscle in a constant location in its proximal third. The muscle may be harvested by way of an open or minimally invasive method and tunneled by way of the subcutaneous tissue at the groin. The distal tip of the muscle is secured into the perineum and sutured over the fistula or sphincter restore. Gracilis repair of rectovaginal and pouch-vaginal fistulas has an general healing fee per affected person of 50% to 92% and successful rate per process of 47% to 85%. A transabdominal strategy may be required for advanced fistulas or those related to a more proximal location of the fistula. Common causes of such fistulas include colovaginal fistula within the setting of complicated diverticulitis in a lady who has had a prior hysterectomy, iatrogenic bowel harm during hysterectomy, rectocele repair, anastomotic leaks after low anterior resection, or prolapse procedures.
Buy vimax torontoOssification centers which appear prenatally (ossified at birth) are: diaphysis of long bones, skull bones, vertebral column, ribs and sternum, few foot bones (talus, calcaneum, cuboid). Primary center of all carpal and tarsal bones (except talus, calcaneum and cuboid) seem after delivery. The flat bones of the skull and face, the mandible, and the clavicle develop by intramembranous ossification. Secondary ossification facilities seem within the epiphyses Ossification is spreading quickly from the ossification facilities and varied bones have gotten ossified Bone of higher limbs and scapulae turning into fully ossified Bone of the decrease limbs and os coxae become utterly ossified Bone of the sternum, clavicles, and vertebrae become fully ossified Nearly all bones are completely ossified Growing End the growing ends of bones in upper limb are upper finish of humerus and decrease ends of radius and ulna. In decrease limb, the decrease end of femur and upper finish of tibia are the rising ends. The higher epiphysis (growing end) has not yet fused with the diaphysis Blood Supply Nutrient artery enters the diaphysis (shaft) through the nutrient foramen, runs obliquely by way of the cortex, and divides into ascending and descending branches within the medullary cavity. Each department divides into a variety of small parallel channels which terminate in the adult metaphysis by anastomosing with the epiphysial, metaphysial and periosteal arteries. Upper end of tibia � Secondary facilities round knee joint (distal femur and proximal tibia) seem during final weeks of intrauterine life (or instantly after birth). Long bones � Long bones develop by endochondral ossification, whereas bones of skull; facial skeleton; mandible; clavicle bone develop by membranous ossification. Towards metaphysis � Nutrient artery enters the shaft (diaphysis) of the bone, divides into ascending and descending branches, which run in course of and terminate within the grownup metaphysis by anastomosing with the epiphyseal, metaphyseal and periosteal arteries. Epiphysis There are 4 kinds of epiphysis: Pressure epiphysis are the components of bone concerned in weight transmission (and are intracapsular) for. Examples of traction epiphyses are tubercles of the humerus (greater tubercle and lesser tubercle), and trochanters of the femur (greater and lesser). For example, the epiphysis on the head of the first metacarpal bone, posterior tubercle of talus (as trigonum). Trochanter of femur � Trochanter of femur is an instance of traction epiphysis and is extracapsular. Greater (and lesser) tubercles in humerus and greater (and lesser) trochanter in femur. For instance, the epiphysis at the head of the first metacarpal bone and at the bases of different metacarpals. Traction � Traction epiphysis are present at the ends of bones and develop because of traction by the hooked up muscle tissue (and are subsequently extracapsular). It is the strongest a part of bone � the strongest part of bone is diaphysis (not metaphysis). Growth exercise is negligible here � Metaphysis is the epiphyseal end of the diaphysis. Osteoblasts give rise to osteocytes � Osteoblasts that get trapped in Haversian lamellae turn into osteocyte and assume the function of bone upkeep. Sesamoid bone � Sesamoid bones develop in certain tendons and cut back friction on the tendon, thus defending it from extreme wear. Ethmoidal � Pneumatic bones have air spaces inside them and are current across the nasal cavity. Joints Union between bones can be in one of three sorts: by fibrous tissue; by cartilage; or by synovial joints. Classification Synarthrosis (immovable) Amphiarthrosis (slight mobile) Diarthrosis (freely mobile) Fibrous joints Cartilaginous joint Synovial joints Fibrous joints occur the place bones are separated only by connective tissue and movement between them is negligible. Examples of fibrous joints are the sutures that unite the bones of the vault of the skull and the syndesmosis between the lower ends of the tibia and fibula. Types of fibrous joint Suture Gomphosis Syndesmosis Examples Spheno-vomerine joint (schindylesis) Tooth and socket joints Middle radioulnar joint Inferior radioulnar joint Cartilaginous joints are of two varieties, main and secondary. Primary Cartilaginous Joints (synchondroses) are united by hyaline cartilage and permit no movement however development within the size. A main cartilaginous joint (synchondrosis) is one the place bone and hyaline cartilage meet. Thus all epiphyses are major cartilaginous joints, as are the junctions of ribs with their very own costal cartilages.
Syndromes - 4 ounces of cooked lean fish, poultry, or meat
- Phenytoin
- Dementia
- X-ray of the abdomen
- Nurse practitioners (NPs) or physician assistants (PAs), who focus on heart and vascular diseases
- Hematoma (blood accumulating under the skin)
- Regrowth of NF tumors
- Weak cry
- Drink at least 1 cup of liquid every time you have a loose bowel movement.
Buy 30caps vimaxAngiodysplasia- an uncommon explanation for colonic bleeding: colonoscopic analysis of 1050 patients with rectal bleeding and anaemia. Changing epidemiology of gastrointestinal angiodysplasia with rising recognition of clinically milder circumstances: angiodysplasia tends to produce mild continual gastrointestinal bleeding in a examine of forty seven consecutive patients admitted from 1980�1989. The function of colonoscopy and radiological procedures in the management of acute lower intestinal bleeding. Scintigraphic detection of gastrointestinal bleeding: a evaluate of present strategies. Use of endoclips to obliterate a colonic arteriovenous malformation earlier than cauterization. Ischaemic proctitis and adventitial fibromuscular dysplasia of the superior rectal artery. Age-related modifications within the colonic blood supply: their relevance to ischemic colitis. Patients with irritable bowel syndrome or constipation have an increased threat for ischemic colitis. Ischaemic colitis in a affected person treated with Glypressin for bleeding oesophageal varices. Ischaemic colitis and immune complexes during gold therapy for rheumatoid arthritis. Colite ischemique et thromboses veineuses recidivante par deficit familial en proteine S [letter]. Anatomic patterns, affected person characteristics, and scientific outcomes in ischemic colitis: a examine of 313 cases supported by histology. Ischemic colitis has a worse prognosis when isolated to the right facet of the colon. Ischemic colitis incidence following abdominal aortic reconstruction: a prospective study. A potential research of clinically and endoscopically documented colonic ischemia in 100 sufferers present process aortic reconstructive surgical procedure with aggressive and direct pelvic revascularization: comparison with historic controls. Colonic ischemia complicating open vs endovascular belly aortic aneurysm repair. Risk elements and outcomes of postoperative ischemic colitis in modern open and endovascular belly aortic aneurysm repair. Today, many of the commonly understood tenets of diverticulitis are being reconsidered. For instance, the understanding that diverticulitis represents discrete episodes of acute colon inflammation followed by a return to an asymptomatic state is being re-evaluated. It is unclear how the continual manifestation of this illness is any completely different than those with more episodic illness. Lastly, patient education is a critical space of want because the supplies available to patients, whether or not in print or on-line, continue to misrepresent the reality about diet and therapy indications for diverticulitis. They may be false diverticula involving the mucosa and muscularis mucosae or true diverticula, involving all layers of the bowel wall. In Western nations, diverticula are commonest in the sigmoid and left colon (95%), and symbolize false diverticula. In Asia, diverticula are extra frequent on the best side of the colon and generally characterize true diverticula. Diverticulosis is usually rare in populations under age 30, however will increase in prevalence with age to embrace nearly all of people by age eighty. In industrialized nations, diverticulosis seems to be equally prevalent in men and women. The growth of bleeding occurs with damage to a diverticulum resulting in intimal thickening, scarring, and irritation of the vasa recta. This sequence leads to bowel lining rupture, with bleeding into the colon lumen rather than into the belly cavity. The situation manifests as left decrease quadrant abdominal pain, malaise, low-grade fevers, and proof of leukocytosis. At that time, an infection can spread systemically through the bloodstream to cause bacteremia or sepsis. At instances, a large abscess can erode into the encircling organs inflicting a fistula. Some sufferers experience lingering signs which are attributable to diverticulosis regardless of decision of inflammation on imaging.
Cheap vimax online visaAbove the superior fovea sulcus limitans presents a flattened gray space called locus ceruleus. Cerebral aqueduct � Cerebral aqueduct of Sylvius is a cavity within the mesencephalon (midbrain), connects the third ventricle within the diencephalon to the fourth ventricle throughout the region of mesencephalon. Ependymocytes � Ependymocytes are cuboidal or columnar in form with tuft of cilia on their luminal surfaces and constitute nearly all of the ependymal cells that line the ventricles of the mind and central canal of the spinal wire. Corpus callosum � the anterior horn of the lateral ventricle lies anterior to its central half, the 2 being separated by an imaginary vertical line drawn at the level of the interventricular foramen. Posterior wall of third ventricle � the posterior boundary of the ventricle is marked by a suprapineal recess, the habenular commissure, a pineal (epiphyseal) recess, which extends into the pineal stalk, and by the posterior commissure. Anterior pituitary � Floor of third ventricle has infundibular recess, which extends into the pituitary stalk (not anterior pituitary). Stria terminalis � Abducent (6), vestibular (8), vagus (10), hypoglossal (12) nuclei are on the ground of 4th ventricle. Vagal triangle � Floor of 4th ventricle has areas related to Abducent (6), vestibular (8), vagus (10), hypoglossal (12) nuclei. Pons � Facial colliculus is a rounded elevation seen within the flooring of 4th ventricle, on the posterior facet of decrease pons. Sixth � Facial colliculus is raised as a result of the axons of facial nerve winding around the abducent nucleus. Risorius � Facial colliculus is a rounded elevation formed by the axons of facial nerve (and not by the abducent nucleus deep to it). Cerebrum Cerebrum is the highest and largest part of brain to control and modulate emotions, character, hearing, vision, and voluntary activities. It is made up of the two cerebral hemispheres having the outer layers of cortex (grey matter) and the underlying areas of axons (white matter). Cerebral cortex is folded into ridges (gyri) and furrows (sulci) to increase the surface area. The two cerebral hemispheres are separated from each other by a deep fissure called the longitudinal fissure. Cerebral hemisphere is split into six lobes: frontal, parietal, occipital, temporal, insular and limbic lobes. Frontal, parietal, temporal, and occipital lobes named upon their overlying neurocranial bones. Dominant hemisphere is liable for propositional language consisting of grammar, speech and calculations. Allocortex itself is two sorts: � Archicortex which incorporates the hippocampus and the dentate gyrus. Sulci in Cerebrum Central sulcus (of Rolando) begins by slicing the superomedial border of the hemisphere about 1cm behind the midpoint between the frontal and occipital poles. It runs sinuously downwards and forwards at an angle of 70� and ends simply above the lateral sulcus. It is the boundary between the frontal motor space and the parietal sensory space posteriorly. Lateral sulcus (of Sylvius) begins as a deep cleft on the inferior floor of the cerebral hemisphere at the anterior perforated substance. It extends laterally between the temporal pole and the posterior a part of the orbital surface of the hemisphere. It continues posteriorly and slightly upwards across the lateral surface and ends in the inferior parietal lobule by an upturned posterior finish. It begins beneath the posterior end of the splenium a part of corpus callosum and follows an arched course with a convexity upwards to the occipital pole and extends upon the superolateral floor. They are longitudinally infolded (as seen in the posterior a half of calcarine sulcus of the visual cortex). Limiting sulci develop along planes separating cortical areas, which differ in the functions. Operculated sulcus is just like a limiting sulcus in that it separates structurally and functionally different areas but the transition occurs on the lip and never the floor.
Buy vimax paypalPercutaneous drainage can take a transabdominal or transgluteal strategy but could result in an extrasphincteric fistula in ano if an anastomotic leak is current. In cases of uncontrolled sepsis or failure of nonoperative management, abdominal exploration with pelvic washout is required. Prompt prognosis and treatment are important to reduce inflammation and the fibrosis that finally leads to pouch dysfunction or loss. This pressure may be alleviated by choosing a more proximal phase of bowel as the site of diverting stoma. Pouch sepsis resulted in increased stool frequency, the necessity for antidiarrheal medication, day and nighttime incontinence, decreased stool/gas discrimination, and sexual dysfunction. Among those patients capable of be treated with a nonoperative strategy, operate is acceptable in more than 90%. The web site of hemorrhage is most frequently intraluminal alongside staple traces or on the ileostomy. Hemorrhage can also occur at an extraluminal web site within the pelvis or peritoneal cavity. The vast majority of staple line bleeding is self-limited, and website of bleeding is often difficult to establish. When minor bleeding or a quantity of points of bleeding are encountered, endoscopy and clipping or cautery of the bleeding site or irrigation of the pouch with a dilute epinephrine answer is efficient in 80% of cases. An examination underneath anesthesia may reveal foci of anastomotic dehiscence that can be managed with transanal drain placement or oversewing as tissue integrity permits. In severe circumstances, packing of the pelvis or detachment of the pouch and careful inspection may be required to management the bleeding. However, use of a small-diameter round stapler can create a slim round opening that can additionally be vulnerable to stenosis because it heals. Larger diameter staplers are less incessantly related to the long-term development of an anastomotic stricture. Symptoms of an anastomotic stricture embrace incomplete evacuation with straining, defecatory urgency, and frequent watery stools. This permits for dilation of stenosis and may detect subclinical anastomotic disruption. If lengthening maneuvers that contain manipulating the mesentery result in ischemia, anastomotic therapeutic shall be compromised. Tension is the commonest and underappreciated threat factor for anastomotic disruption. Short gentle strictures because of an online formation at circular staple strains are adequately dilated in a single session as a result of every day bowel function will help forestall recurrence. Hegar dilators can be used to sequentially dilate the anastomosis in the clinic or operative setting. Dilation alone is profitable in 95% of nonfibrotic strictures and only 45% of fibrotic strictures. Strictures refractory to dilation extra generally occur as a consequence of pelvic sepsis with resultant fibrosis. In a examine of 1884 restorative proctocolectomy patients handled at Mayo Clinic, 11. Excision of a brief segmental stricture with mucosal development was performed in 5 patients, the pouch was redone in three patients, and excision of the pouch with permanent ileostomy was carried out in 9 sufferers. All nine excised pouches have been related to perianastomotic problems, together with abscess, fistula, or pouch retraction. Transvaginal restore was associated with a healing price of 55% when performed as a major procedure, and 40% when carried out as a secondary procedure. However, the good factor about diversion in reducing the extent of pelvic sepsis would counsel a theoretical risk discount of sepsis-related fistulas. Regardless, diversion is usually carried out for advanced fistula repair and partly presents respite from symptoms.
Trusted vimax 30capsThe left posterior cardinal vein beneath the level of the renal vein develops into left inferior vena cava while normal inferior vena cava develops on the right side. Double inferior vena cava may end result as a result of persistence of left supracardinal vein is mentioned by many of the authors. Some authors mention it is due to persistence of each (right and left) subcardinal and supracardinal veins. The cranial part of proper subcardinal vein which usually disappears, persists and carries the blood from the inferior vena cava to the superior vena cava. The hepatic veins immediately open into the right atrium at the website of the inferior vena cava. Supracardinal vein and subcardinal vein � Inferior vena cava develops from a quantity of sources, subcardinal vein having significant contribution, especially the renal phase and the postrenal segment (anastomosis between right supracardinal and subcardinal vein). Coronary sinus � Left sided superior vena cava drains into the coronary sinus and thence into the best atrium (occasionally instantly into the proper atrium). The lymphatic system develops later than the cardiovascular system, originating from the endothelium of veins as 5 sacs: two jugular, two iliac, one retroperitoneal, and one cisterna chyli. Thoracic duct forms from anastomosis of the best and left thoracic ducts, the distal part of the proper thoracic duct, and the cranial part of the left thoracic duct. The right lymphatic duct develops from the cranial a half of the best thoracic duct. The lymphatic system develops at the end of the fifth week, about one week later to that of the cardiovascular system. Development of Thoracic Duct There are three steps in the development of the thoracic duct: 1. Stage I: A network of lymph channels is fashioned in entrance of the thoracic a half of the vertebral column. Now the right longitudinal channel under cross communication and the left longitudinal channel above communication persists and provides rise to the thoracic duct. Both thoracic and right lymphatic ducts open into the junction of the proper lymphatic ducts inner jugular and subclavian vein of the left and proper aspect, respectively. From the left atrium, blood enters the left ventricle and is delivered to fetal tissues via the aorta. Poorly oxygenated and nutrient-poor fetal blood is distributed again to the placenta by way of proper and left umbilical arteries. Some blood in the best atrium enters the best ventricle; blood in the best ventricle enters the pulmonary trunk, however a lot of the blood bypasses the lungs through the ductus arteriosus. Fetal lungs obtain only a minimal amount of blood for growth and growth; the blood is returned to the left ventricle through pulmonary veins. Circulatory system adjustments at delivery are facilitated by a lower in right atrial pressure from occlusion of placental circulation and by an increase in left atrial stress because of increased pulmonary venous return. Changes embody closure of the right and left umbilical arteries, left umbilical vein, ductus venosus, ductus arteriosus, and foramen ovale. Fetal circulation: Oxygenated blood travels from the placenta alongside the left umbilical vein. Most blood by-passes the liver within the ductus venosus joining the inferior vena cava and then travelling to the proper atrium. Most of the blood passes via the foramen ovale into the left atrium in order that oxygenated blood can enter the aorta and reach the mind at earliest. The the rest goes via the best ventricle with returning systemic venous blood into the pulmonary trunk. The unexpanded lungs present excessive resistance to move so that blood in the pulmonary trunk tends to move down the low-resistance ductus arteriosus into the aorta. Blood returns to the placenta through the umbilical arteries (branches of the inner iliac arteries). At birth, when the child breathes, the left atrial strain rises, pushing the septum primum towards the septum secundum and shutting the foramen ovale. Blood circulate by way of the pulmonary artery will increase and becomes poorly oxygenated as it now receives systemic venous blood. Pulmonary vascular resistance is abruptly lowered as lungs inflate and the ductus arteriosus is obliterated over the following few hours to days. Umbilical artery: Lateral umbilical ligament � Umbilical arteries turn out to be medial umbilical ligaments.
Discount vimax 30 caps with mastercardThe authors discovered that the probability of morbidity and mortality was lowest for Hartmann procedure and highest for primary anastomosis with out diversion. However, stomas remained everlasting in 27% of patients with end colostomy however in solely 8% of patients with anastomosis and fecal diversion. A determination model revealed that the optimum strategy was main anastomosis with proximal fecal diversion because of the high complication price with out diversion. However, Hartmann procedure turned the optimum strategy in very high-risk sufferers with substantial morbidity and mortality. The initial sequence in 1996 included eight sufferers with perforated diverticulitis and purulent peritonitis who underwent laparoscopic lavage as the only therapy with no interval resection. The technique obtained little attention until the publication of a prospective multiinstitutional trial in 2008 of one hundred sufferers with perforated diverticulitis who underwent laparoscopic lavage. From this total, eight sufferers had been discovered to have feculent peritonitis, converted to an open Hartmann resection. Ninety-two sufferers were managed with laparoscopic lavage, and no patient required subsequent resection for diverticulitis. Two patients developed a pelvic abscess within the postoperative period and required drainage, and two patients presented with a subsequent assault of diverticulitis. The morbidity was 4%, and the mortality was 3%, much decrease than what has historically been reported for the Hartmann procedure. Three randomized trials have lately examined the function of laparoscopic lavage within the therapy of patients with perforated diverticulitis. The main end result was extreme postoperative issues within 90 days, which occurred in 30. Lavage resulted in no difference in mortality and morbidity, but was related to shorter working time and shorter hospital stay. For example, which patients should be selected for lavage, ought to patients have subsequent resection after lavage, and what are the long-term outcomes A number of scientific follow tips have been refined to embrace a press release on the role of lavage. The Association of Coloproctology of Great Britain and Ireland states that "laparoscopic lavage may play a job in some sufferers with acute diverticulitis. Hartmann takedown is associated with considerable morbidity and mortality, and up to a third of sufferers, for a selection of reasons, never bear stoma reversal. Hartmann takedown (reversal): After Hartmann resection for perforated diverticulitis, most sufferers are eager to proceed as soon as possible with stoma reversal. These sufferers have typically introduced with free perforation as the preliminary manifestation of diverticulitis and never anticipated requiring a stoma for therapy. Reversal surgical procedure could additionally be undertaken early (<3 months from the initial surgery) or later (>3 months from the preliminary procedure). There are advocates of every strategy and no randomized trials to information suggestions. Proceeding with a Hartmann takedown close to the time of preliminary surgical procedure has several disadvantages, predominantly due to adhesions and the acute inflammatory response after initial surgery, which can result in a difficult dissection, potential enterotomies, and problem with identification of the Hartmann stump. While ready for no much less than three months will presumably permit the patient sufficient time to heal and facilitate identification of the Hartmann stump, ready longer could make identification of the stump more difficult secondary to fibrosis. Prior to reversal, a Gastrografin enema through the rectum is useful to present an assessment of the size and configuration of the rectal section, along with assessing residual sigmoid colon and/or diverticula. Another advantage to this imaging research is that fecal residue may be evacuated, which ultimately helps with passing the round stapler and the sizer. Colonoscopy or barium enema is performed via the stoma, and a mechanical bowel preparation is administered previous to surgery. The affected person is positioned in low lithotomy place or (preferably) on the split-leg desk with the legs kidnapped. Initial dissection is concentrated on lysing adhesions of the small bowel to establish the Hartmann pouch; within the majority of cases this involves lysing the majority of the adhesions from the ligament of Treitz to the ileocecal valve. With few exceptions, there are generally small bowel adhesions or omental adhesions to the highest of the Hartmann pouch. Mobilization of the Hartmann pouch is carried out as wanted to be succesful of cross the sizer.
|