|
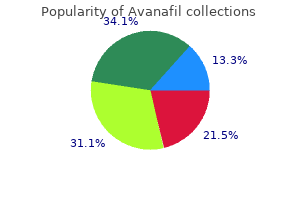
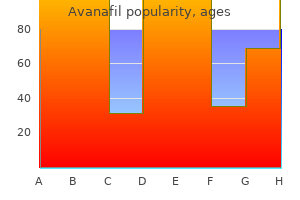
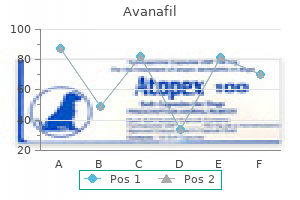
Avanafil dosages: 200 mg, 100 mg, 50 mg
Avanafil packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills
Cheap avanafil online amexThese segmental arteries are known as "segmental anterior medullary arteries" and are important to the spinal injectionist because they represent a direct route for delivery of probably damaging particulate treatment into the parenchyma of the spinal twine. There is a mean total of eight anterior medullary feeder arteries (inclusive of all spinal ranges bilaterally), the largest of which is the great anterior medullary artery or artery of Adamkiewicz. The complete number of anterior medullary feeder arteries varies from 2 to 17 in different people, with a median of three in the cervical area, three within the thoracic region, and two within the lumbar region. The artery of Adamkiewicz usually enters the cord on the left side (77% of specimens) wherever from T7 to L4 (most generally between T9 and T12) and may be the primary blood supply to the lower 2/3 of the spinal wire. In the cervical area, the largest anterior medullary arteries sometimes enter at C4/C5 or C5/C6 [8]. Since the quantity and place of segmental medullary spinal feeder arteries is variable and relatively unpredictable, nice care should be taken with any injection into any intervertebral neuroforamen. The foramina more than likely to include these arteries are in the decrease cervical, lower thoracic, and upper lumbar regions of the spine, although any intervertebral foramen may include a feeding spinal artery. These arteries sometimes anastomose with the anterior spinal arteries and provide direct routes for blood move into the parenchyma of the spinal twine. Any particulate matter (including particulate steroid) has the potential to occlude the distal arterioles of these spinal finish arteries, creating extensive wire infarction within the downstream spinal tissue. There have been numerous instances of paralysis and death associated with inadvertent injection of particulate steroid into intraforaminal segmental spinal feeding arteries during interventional ache procedures [9�13]. It is essential for the spinal injectionist to have an in depth understanding of spinal anatomy. The spinal column is a fancy structure consisting of multiple bones, ligaments, and intervertebral discs, that are functionally built-in to facilitate upright locomotion and to provide safety for the spinal twine. The picture showing on the fluoroscopic monitor is a composite representation of the overlapping tissue densities that lie between the x-ray tube and the picture intensifier. The prototypical vertebra is composed of an anterior cylindrical block of bone called the vertebral body which is connected to the posterior neural arch by the pedicles. The spinal twine begins within the skull, exits the foramen magnum, and ends with the filum terminale at roughly L1/L2, giving rise to 31 pairs of spinal nerves. Schultz Posterior spinal arteries Anterior spinal artery Anterior segmental medullary artery Anterior radicular artery Posterior radicular artery Branch to vertebral physique and dura mater Spinal branch Dorsal branch of posterior intercostal artery Posterior intercostal artery Paravertebral anastomoses Prevertebral anastomoses Thoracic (descending) aorta Section through thoracic stage: anterosuperior view Sulcal (central) branches to right facet of spinal twine Posterior radicular artery Anterior segmental medullary artery Pial arterial plexus Anterior and posterior radicular arteries Anterior spinal artery Right posterior spinal artery Peripheral branches from pial plexus Sulcal (central) branches to left aspect of spinal twine Left posterior spinal artery Posterior radicular artery Arterial distribution: schema Anterior segmental medullary artery Pial arterial plexus Note: All spinal nerve roots have related radicular or segmental medullary arteries. All rights reserved) 7 Anatomy of the Spine for the Interventionalist Crura of diaphragm Posterior longitudinal ligament Psoas 87 Dura Pedicle Aorta Cauda equina Internal vertebral plexus of veins in extradural area Ligamenta flava Interspinous ligament Supraspinous ligament Quadratus lumborum Vein Erector spinae muscle tissue Lumbar artery Intervertebral foramen Intervertebral disc Vertebra Skin Lamina. The intervertebral discs fill the areas between adjoining vertebral our bodies from C2 to the sacrum with a central semiliquid nucleus pulposus surrounded by a circumferential annulus fibrosus. The spinal cord receives its blood provide from three longitudinal arteries including a single anterior spinal artery and two posterior spinal arteries and a variable variety of intraforaminal segmental arteries that pose direct routes of injection into the spinal cord. Cervical transforaminal epidural injections are associated with extremely excessive risk. In distinction, the arteries may be avoided within the majority of the sufferers with alternate strategies. Acknowledgments this guide chapter is modified and updated from a previous book chapter, "Spinal Anatomy for the Interventionalist" by David M. Engel A, King W, MacVicar J, Standards Division of the International Spine Intervention Society. The effectiveness and risks of fluoroscopically guided cervical transforaminal injections. Anatomic dissection that demonstrates the path of the C8 radicular artery (arrowheads) as it follows the inferior aspect of the C8 spinal nerve through the intervertebral foramen to be part of with the anterior spinal artery. This specific vessel is bigger than a 22-gauge needle (shown for scale) of steroids: a scientific evaluation with comprehensive evaluation of the printed data. Latchaw eight Introduction the role of this chapter is to show and discuss pertinent imaging findings, both normal and pathological, that may aid the spinal interventionalist in offering remedy to the patient. This chapter is divided in accordance with presentation; for example, cervical pain situations are mentioned separately from these in the lumbosacral (L�S) backbone; both are subdivided into disc illness, side disease, focal nerve root compression for which nerve root block may be an possibility, and other causes of spinal and radicular pain. Important points relating to the imaging traits of both normal and abnormal conditions are mentioned within the legends to the numerous illustrations.
Larch Arabinogalactan. Avanafil. - Are there any interactions with medications?
- Common cold, flu, liver disease, high cholesterol, earache (otitis media), HIV/AIDS, cancer treatment, dietary fiber supplementation, stimulating the immune system, inflammation, and other conditions.
- How does Larch Arabinogalactan work?
- What is Larch Arabinogalactan?
- Dosing considerations for Larch Arabinogalactan.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96935
Buy avanafil torontoIt is essential that the affected person stay relaxed and immobile as movement might stop aspiration of oocytes and enhance the risk of damage to the encircling organs and vessels. After retrieval is completed within the first ovary, the needle is withdrawn; the other ovary is recognized, and a second puncture is made by way of the vaginal fornix. After all of the follicles have been aspirated, the needle and ultrasound probe are removed. A sterile speculum is then reintroduced into the vagina, and the vaginal wall and cervix are inspected for hemostasis. The most stimulating components of the procedure occur when the vaginal fornix is pierced on each side and when the ovarian follicles are entered for aspiration of the eggs. The general trend is to avoid laparotomies and to perform operations using outpatient laparoscopy and hysteroscopy strategies each time possible. If done by laparotomy, a urethral catheter is inserted to empty the bladder, adopted by the insertion of a transcervical uterine catheter for chromopertubation (dye injection). During the operation, microsurgical methods are adopted intently to minimize trauma. Chromopertubation is then carried out and, if occlusion is present, a new stoma is created using microsurgical instruments and sutures. Tubal reanastomosis, carried out to restore fertility, is similar to fimbrioplasty, with microsurgical methods followed diligently. After the tubal segments have been freed barely from their underlying mesosalpinx, the occluded ends are cut, and chromopertubation is carried out to guarantee patency. At times, the fusion is incomplete, and a septated uterus or bicornuate uterus is shaped. The malformed uterus is associated with an elevated risk for miscarriages and preterm labor. The Strassmann procedure (extremely rare) for bicornuate uteri uses a regular pelvic laparotomy. Following uterine exposure, an incision is made on the medial aspect of every hemicorpus and carried down until the uterine cavity is entered. Septated uteri are normally repaired through a hysteroscopic approach (see Hysteroscopy, p. Proximal tubal cannulation is a process by which proximal tubal occlusion may be repaired through both fluoroscopic or hysteroscopic approach. This process is usually carried out with laparoscopy to observe the progress of the cannulization and to visualize the chromopertubation (see Hysteroscopy, p. These follicles are then punctured with a needle transvaginally to "harvest" the eggs. Usual preop analysis: Infertility; history of multiple spontaneous abortion and preterm labor (For summaries of particular procedures, see Laparoscopy, p. General anesthes Regional anesthe: A T4-6 sensory l061evel is beneficial for pelvic/lower stomach surgery. For laparoscopic procedures, breathing issue can develop as a end result of pneumoperitoneum and Trendelenburg position. No difference in pregnancy rates with the utilization of isoflurane, propofol, N2O, or midazolam has been demonstrated. Tanbo T: Assisted fertilization in infertile women with patent tubes: a comparability of in vitro fertilization, gamete intra-fallopian switch and tubal embryo stage transfer. The vaginal strategy, performed with the affected person in a dorsal lithotomy position, is most well-liked because it provides considerably much less morbidity and mortality. Use of the vaginal strategy could also be limited by such components because the pelvic bony architecture, extreme uterine dimension, pelvic adhesions, or the presence of gynecological cancers, thus requiring an stomach or laparoscopic/robotic strategy. More recently, minimally invasive approaches with laparoscopy and robotic surgical procedure have allowed for decreased morbidity and recovery time when compared to an stomach method. For a complete laparoscopic, laparoscopic-assisted, or robotic-assisted hysterectomy patients are placed in a low lithotomy place, and abdominal entry is confirmed with the laparoscope once the stomach has been insufflated. For a laparoscopic or robotic-assisted hysterectomy, the patient is positioned in a steep Trendelenburg. In these instances, the hysterectomy is commonly accompanied by an anterior/posterior colporrhaphy, vault suspension, and perineoplasty. Variant approaches: Abdominal hysterectomy is carried out through a Pfannenstiel or midline incision, relying on the uterine size and the want to carry out a lymph node dissection for cancer. A Pfannenstiel incision often could be extended with two kinds of muscle-splitting steps: the Maylard, by which the rectus muscle tissue are minimize, or a Cherney rectus muscle detachment performed at the pubic insertion.
Avanafil 50mg with mastercardAnatomical, technical, and medical variables of stellate ganglion block compared to cervical and thoracic sympathetic blocks individually have led to the impressions that stellate ganglion block may not be the best treatment for higher extremity sympathetic block. Thoracic sympathetic blocks have been assessed in a single randomized double-blind managed trial and two uncontrolled research, exhibiting efficacy with improvement in ache relief at 12-month follow-up, nonetheless, with injection of steroids. Psychological aspects of reflex sympathetic dystrophy: a evaluate of the adult and pediatric literature. Pharmacological approaches to the therapy of persistent pain: new concepts and important points. International affiliation for the study of pain: classification of continual pain: description of continual ache syndromes and definitions of ache terms. Is nociceptor activation by -1 adrenoceptors the wrongdoer in sympathetically maintained ache The plasticity of cutaneous hyperalgesia throughout sympathetic ganglionic blockade in patients with neuropathic pain. Electrical stimulation of the upper thoracic portion of the sympathetic chain in man. Clinical and neurophysiological observations regarding pathophysiological mechanisms of reflex sympathetic dystrophy. Predisposing psychological components within the development of reflex sympathetic dystrophy. Etiopathogenesis of reflex sympathetic dystrophy: a review and biopsychosocial hypothesis. Psychological characteristics of reflex sympathetic dystrophy versus myofascial pain syndromes. Critical review of managed scientific trials for peripheral neuropathic pain and complicated regional ache syndromes. Complex regional ache syndrome sort I: incidence and danger factors in patients with fracture of the distal radius. Complex regional pain syndrome sort I: incidence and prevalence in Olmsted county, a population-based examine. Reflex sympathetic dystrophy: a retrospective epidemiological study of 168 patients. Management of complicated regional pain syndrome type I in upper extremity � evaluation of continuous stellate ganglion block and continuous infraclavicular brachial plexus block: a pilot study. The results of stellate ganglion block with lidocaine and ultrasound in advanced regional pain syndrome: a randomized, double blind, placebo controlled research. Analysis of peak magnitude and period of analgesia produced by local anesthetics injected into sympathetic ganglia of complicated regional ache syndrome sufferers. Intravenous regional block is just like sympathetic ganglion block for ache administration in patients with complicated regional ache syndrome type I. Early thoracic sympathetic block improves the remedy effect for upper extremity neuropathic pain. Stellate ganglion block in reflex sympathetic dystrophy: a double-blind crossover examine. Thermographic evaluation of the sympathetic blockade by stellate ganglion block (2) comparison and analysis A. Comparison of various injectate volumes for stellate ganglion block: an anatomic and radiologic study. Comparison of the efficacy of a lowvolume stellate ganglion block with a "conventional" approach. Radiofrequency lesions of the stellate ganglion in chronic ache syndromes: retrospective evaluation of clinical efficacy in 86 sufferers. Pai, and Laxmaiah Manchikanti 35 Introduction Lumbar sympathetic block is likely one of the most common procedures carried out in managing pain problems of the stomach and decrease extremity. As prognostic indicators, lumbar sympathetic blocks are helpful in identifying the candidates and the potential unwanted effects of patients for neurolytic or surgical sympathectomy. In addition, lumbar sympathetic interventions are applied for treatment of various conditions. A resurgence of curiosity appeared within the 1950s when Bonica [4] and Arnulf [5] described in detail the significance of lumbar sympathetic blockade, especially in relationship to therapy of S. Considering the incidence of genitofemoral neuritis of 5% to 10% following a neurolytic lumbar sympathetic block, Ohno and Oshita [7] advocated a transdiscal strategy. A paradiscal, extraforaminal method to the lumbar sympathetic block additionally has been mentioned as a way of avoiding potential problems as well as attaining the best block [8].
Purchase avanafil ukPathological findings associated with trigeminal neuralgia caused by vascular compression. From paroxysmal to continual ache in trigeminal neuralgia: implications of central sensitization. Association of trigeminal neuralgia with a quantity of sclerosis: medical and pathological features. Amyloidoma of the gasserian ganglion as a explanation for symptomatic neuralgia of the trigeminal nerve: report of three circumstances. Comparison of percutaneous radiofrequency gangliolysis and microvascular decompression for the surgical administration of tic douloureux. Percutaneous retrogasserian glycerol rhizotomy: predictors of success and failure in remedy of trigeminal neuralgia. Comparison of the long-term outcomes of microvascular decompression and percutaneous trigeminal neurolysis for the treatment of trigeminal neuralgia. Comparison of surgical therapies for trigeminal neuralgia: reevaluation of radiofrequency rhizotomy. Complications of treating trigeminal neuralgia: an analysis of the literature and response to questionnaire. Cerebrovascular accident after percutaneous radiofrequency thermocoagulation of the trigeminal ganglion. Dangerous rises in blood pressure upon heating of trigeminal rootlets: elevated bleeding time in sufferers with trigeminal neuralgia. Occipital Nerve Blocks and Neurolysis Diego Fernandez Garcia-Roves, Boleslav Kosharskyy, and Karina Gritsenko 27 Introduction As per the International Headache Society, occipital neuralgia is a unilateral or bilateral paroxysmal, shooting, or stabbing pain within the posterior part of the scalp, in the distribution of the greater, lesser, or third occipital nerves sometimes accompanied by diminished sensation or dysesthesia within the affected space and commonly associated with tenderness over the involved nerve(s) [1]. The use of occipital nerve block has been propagated in occipital and cervical pain syndromes because the 1970s. Its use was finally established in cervicogenic headache, changing into not only a therapeutic option but additionally part of the diagnostic procedure. Pathophysiology Patients may be divided into those with underlying structural pathology and those with idiopathic causes [1]. Occipital neuralgia is brought on by harm to the aforementioned nerves, and this might be a result of trauma, bodily stress on the nerve, repetitive neck contraction, flexion or extension, tumors (local tumors like osteochondroma or metastatic illness of some tumors to the spine), cerebrospinal fluid leaks, or radiofrequency nerve ablation [2]. The most accepted rationalization relating to the physiopathology of occipital neuralgia is the entrapment of occipital nerves by the posterior neck and scalp muscle tissue [3�5]. The features and assumed etiology discovered in the medical literature have varied significantly over time. Various places had been proposed for the first lesion in the course of the nineteenth century, together with nerve roots, ganglia, trunks, and branches, as properly as the brain and spinal cord. Later in the century, some proposed that it may be an affliction of organs such because the uterus or liver, whereas others classed for the primary time sure complications as neuralgias. The pain is usually located in a single aspect, though bilateral symptoms are possible. Occipital neuralgia has been described as intermittent (paroxysmal) or continuous. In intermittent neuralgia, headache can current as single flashes of ache although a quantity of attacks are extra frequent. Those attacks may be spontaneous or brought on by specific maneuvers applied to the again of the scalp or neck [8]. Acute continuous occipital neuralgia is normally secondary to an underlying illness. Symptoms last for hours, with cold being a standard trigger and infrequent radiating symptoms. Localized spasms of local muscular tissues are regularly current, and so is radiation of pain (especially to the orbital region). Pain is often unilateral, and a historical past of cervical or occipital trauma or arthritic disease is present many of the instances.
Buy avanafil 50mg overnight deliveryThe alternative of injectable treatment that features glucocorticoid with or without native anesthetic, the frequency of injection, and potential problems will likewise be addressed. Needle and Syringe Size the best technique is to use one needle and syringe measurement for the injections to enable the operator to get used to resistance supplied by injecting through the same syringe and needle dimension. This will help recognize greater resistance afforded by injecting by way of a tendon substance. One might choose to use a larger needle such as 20 gauge if using a high viscosity materials like hyaluronate. Too big of a syringe may create too much vacuum, and the alternative holds true for small syringes. However, small-volume tendon sheath injection can finest be accomplished with tuberculin-sized syringe. Sterile Preparation General Technique When performing joint injections, a giant number of things corresponding to needle, syringe size, pores and skin sterilization, and local anesthesia must be taken under consideration. Ultrasonography and fluoroscopy could additionally be of worth to ensure proper needle placement and enhance accuracy [1]. Cleaning the injection site with iodine disinfectant and chlorhexidine prep kit is both acceptable [2, 3]. The generally used preparations are methylprednisolone (Depo-Medrol) and triamcinolone acetonide (Kenalog). Another point of debate was the follow of mixing glucocorticoid with lidocaine as a diluent. The lidocaine serves its role as a pain reliever in addition to providing instant aid. Methylparaben, a bacteriostatic agent in native anesthetic, was found to be the wrongdoer for precipitation of steroid crystals and therefore is normally prevented. There is an absence of definitive data relating to the dose of glucocorticoid and quantity of injection to be used. Again, based mostly on habits alone, 40 mg of steroid injection is used for giant joints similar to shoulders and knees; 30 mg for the wrist, ankle, and elbow; and 10 mg for small areas such as tendon sheaths and metacarpophalangeal joints. The frequency of injection is likewise controversial due to theoretical mechanism for attainable cartilage and tendon injury. Studies have demonstrated the capability of glucocorticoids to inhibit the manufacturing of collagenases and other metalloproteases which may mediate cartilage destruction induced by rheumatoid arthritis or osteoarthritis [5, 6]. Literature varies in their advice from as soon as a month as a lot as 4 injections in a 12 months [7�9]. This usually occurs once the operator encounters a better resistance flow throughout injection and could be very essential to be acknowledged and abort the injection. Once the perineurium is violated, reasonable pain could ensue, accompanied by burning sensation. Minor issues similar to pores and skin atrophy, hypopigmentation, and dystrophic calcification around the joint capsule could happen. Systemic impact of steroids can manifest as ecchymoses, menstrual irregularity, cataract formation, hyperglycemia, osteoporosis, osteonecrosis, and suppression of hypothalamic-pituitary axis. Longer intervals between injections and good glycemic control particularly in diabetic sufferers are advocated. Complications Complications following joint injections are uncommon apart from the inherent risk of an infection, tissue trauma, and bleeding. The opposed outcomes related to glucocorticoid injection are unusual but, if it occurs, could also be catastrophic and oftentimes iatrogenic. Infectious Complication the development of septic joint after injection is comparatively uncommon with an estimated frequency approximately 1 in 2600 procedures [10]. This ought to be distinguished from postinjection flare which usually lasts longer and begins after 48 hours after injection. The affected person may complain of increasing pain depth, fever, malaise, and drainage over the injection website suggestive of iatrogenic septic joint. Shoulder Injection Introduction Noninfectious Complication Injection of an undiluted glucocorticoid near the rotator cuff and/or insertion of the tendons could lead to tendon rupture. This is normally extra common with the posterior method versus the anterior approach on shoulder injection. The shoulder is considered one of the mostly injured sites which will benefit from diagnostic and therapeutic injections.
Proven avanafil 200mgThe superior hypogastric sympathetic plexus resides on the anterior aspect of the vertebral bodies of L5 and S1 and extends throughout the L5/S1 disc, whereas the inferior hypogastric sympathetic plexus resides decrease, anterior to the midline of the sacrum on the stage of S2 to S4 [1]. It is a retroperitoneal construction that extends bilaterally below the aortic bifurcation. It is fashioned by pelvic visceral afferent and efferent sympathetic nerves from branches of the aortic plexus and fibers from the splanchnic nerves [2]. It innervates the vast majority of pelvic viscera (including the bladder, urethra, uterus, vagina, vulva, perineum, prostate, penis, testes, rectum, and descending colon), and therefore block of this plexus can potentially alleviate pain originating from these areas. Percutaneous neurolysis of the superior hypogastric plexus is an environment friendly, relatively simple methodology of management of pain attributable to advanced pelvic most cancers which is immune to the pharmacological treatment. Combining a superior hypogastric block with celiac plexus block is often done to alleviate belly pain secondary to an in depth malignancy. Inferior hypogastric plexus block is used for pelvic ache for organs positioned extra inferiorly within the pelvis with good results [1]. History Initial attempts to performing a hypogastric plexus block go as far again as in 1899 by Jaboulay [3]. Blockade of the superior hypogastric sympathetic plexus was largely pioneered by the work of Plancarte et al. Their work centered on treating pain with a strong visceral component arising from most cancers of the cervix, prostate, and testicle or postradiation cystitis and proctitis. They described a method of using a posterior method with two needles directed medially and caudally to approach the area anterior to the L5/S1 disc. Hypogastric block is technically more challenging to carry out as a outcome of iliac crest or a outstanding transverse course of which can hinder needle development. More recently, in 2007, Schultz described a method for accessing the inferior hypogastric plexus using a transsacral approach with the intent of having the flexibility to present blockade of pain fibers from the genitalia and lower pelvis [1]. Pathophysiology Blocking the transmission of the sympathetic tracts has been extensively used to treat cancer ache. Cancer of the pelvis normally invades the encompassing buildings together with the lymph nodes. Superior hypogastric plexus transmits visceral painful stimulations from the right colon, uterus, cervix, tubes, higher vagina, and bladder [8]. Presacral neurectomy is primarily used to deal with non-oncologic painful circumstances similar to endometriosis. Presacral plexus (superior and inferior hypogastric plexus) may be approached by laparotomy or laparoscopy as 573 B. Visceral ache of the pelvis arising from benign pain syndromes and malignancy of the prostate, testicle, cervix, rectum, and other perineal buildings is communicated by way of afferent nerve fibers that converge on the superior and inferior hypogastric plexuses. Blockade of these afferent fibers by way of native anesthetic and/or neurolysis seeks to interrupt ache transmission from the pelvis. Visceral pain, particularly most cancers pain, is complex and normally involves interplay of neuropathic, visceral, and somatic mechanisms. This explains the shortage of unequivocal information demonstrating efficacy of this block in larger studies. Benign chronic pelvic pain is most probably due to endometriosis, previous pelvic surgery, adhesive disease, and pelvic inflammatory disease. Cancer ache patients complain of diffuse achy ache with poor referral patterns, normally bilateral and never relieved with traditional analgesics. Pancreatic ache is extra viscerally mediated and hence responds to sympathetic block better as in comparability with continual pelvic ache. Outcomes of ache depth by visible analog scale, quality of life, adverse results, and opioid consumption earlier than and after treatment had been measured. At eight weeks, it was seen that early or late neurolytic blocks had been higher than the pharmacological treatment. Traditionally, superior hypogastric plexus block is guided by fluoroscopy with bilateral needles. Also superior hypogastric plexus block has been combined with celiac plexus blocks with some good efficacy to deal with end-stage abdominal malignancies [13�15]. From an evidence-based medicine viewpoint, superior hypogastric plexus block to deal with persistent pelvic ache has not yet been adequately supported by managed studies to treat oncologic ache [16].
Syndromes - Diarrhea
- Demand attention by fussing
- Bone marrow aspiration and biopsy
- Nerve blocks
- Diarrhea or constipation
- Difficulty walking or shuffling gait
- Severe illness
- Some medicines can alter your ability to smell and taste things. Changing your medicine may improve this.
- Weakness
Buy cheap avanafil 200mg on-lineAcknowledgments this guide chapter is modified and updated from a previous guide chapter, "Fluoroscopy in the Interventional Pain Unit: A Physician Perspective" by David M. Interventional strategies 9 Fluoroscopy in Interventional Pain Management in persistent spinal pain. Risk of complete body radiation exposure and protecting measures in fluoroscopically guided interventional techniques: a potential evaluation. Radiation exposure of the spinal interventionalist performing fluoroscopically guided lumbar transforaminal epidural steroid injections. Radiation exposure to the doctor performing fluoroscopically guided caudal epidural steroid injections. Epidural steroids for treating "failed again surgery syndrome": is fluoroscopy actually essential The role of fluoroscopy in cervical epidural steroid injections: an analysis of contrast dispersal patterns. The development of interventional pain management within the new millennium: a important evaluation of utilization in the Medicare population. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a potential, descriptive report. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective analysis of epidurography distinction patterns and anatomical review of the epidural house. Contrast circulate traits in the cervical epidural area: an analysis of cervical epidurograms. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Acute radiation dermatitis following radiofrequency catheter ablation of atrioventricular nodal reentrant tachycardia. Radiation-induced pores and skin damage after percutaneous transluminal coronary angioplasty: case report. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Occupational radiation exposure to interventional radiologists: a prospective study. Effectiveness of protective measures in reducing risk of radiation exposure in interventional pain management: a prospective evaluation. Fluoroscopy radiation security for backbone interventional ache procedures in university teaching hospitals. Schultz 10 Introduction Placing needles and other instruments of interventional pain management safely into the physique requires superior tactile expertise, complete knowledge of anatomy, and expertise with fluoroscopy [1]. Specialists throughout the new specialty of interventional ache management come from various backgrounds including anesthesiology, radiology and physiatry. Practitioners with an anesthesiology background often begin interventional pain follow with glorious tactile expertise honed from years of performing "blind injections" for regional anesthesia but might lack experience in the usage of fluoroscopic imaging. Those with radiology background could additionally be skilled in using fluoroscopy but may not have developed the learned tactile techniques of regional anesthesia. Physical drugs physicians could have an excellent understanding of anatomy and bodily analysis with little expertise in regional anesthesia or fluoroscopy. The aspiring interventional pain specialist doctor must develop expertise in regional anesthesia, radiological imaging, and anatomy to have the ability to turn out to be an effective and secure practitioner. The following step-by-step outline for performing interventional pain procedures is based on the premise that consistency and preparedness within the preinjection routine fosters effectivity, effectiveness, and security. Set Up the Room Prior to performing injection procedures, the procedure room should be thoughtfully arrange for optimum effectivity and security. Facilities that present interventional therapies must have on-site nursing staff skilled in resuscitation strategies and resuscitation tools together with a whole crash cart with D. Orient the Fluoroscope Prior to performing the process, the practitioner should first orient the fluoroscope. Schultz from a well-known place and viewing an image with related orientation each time, the brain will type associations that improve hand-eye coordination and facilitate fast and environment friendly needle placement. Once the fluoroscope is powered up and its picture oriented, the injectionist might start with the procedure.
Order avanafil canadaAgents used to deal with ache include morphine and different opioids, ziconotide, a drug that acts on the calcium channels, and adjuvants such as local anesthetic (bupivacaine), and medicines that work on the alpha receptors (clonidine). Baclofen has been accredited by the Food and Drug Administration to treat persistent spasticity. The use of intrathecal drugs for pain may lead to a reduction of the need for oral or transdermal opioids and subsequently might scale back the variety of controlled substances in the community. Patients ought to be thought-about for an intrathecal pump if pain is either refractory to acceptable medical therapy or dose-limited due to significant unwanted side effects. The intrathecal methodology allows for a decrease equipotent dose as in comparability with different supply routes and may cause decrease systemic effects secondary to both lower blood ranges of both the drug and related metabolites. Conversions for intrathecal to epidural to systemic opioids are controversial for continual pain patients. Systematic literature evaluation and meta-analysis of the efficacy and security of prescription opioids, together with abuse-deterrent formulations, in non-cancer pain administration. Reply to commentaries on "Randomized medical trial of an implantable drug supply system compared to complete medical administration for refractory cancer pain: influence on pain, drug-related toxicity, and survival". Accuracy and efficacy of intrathecal administration of morphine sulfate for treatment of intractable ache utilizing the Prometra programmable pump. Randomized scientific trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impression on ache, drug-related toxicity, and survival. Polyanalgesic consensus conference-2012: suggestions on trialing for intrathecal (intraspinal) drug delivery: report of an interdisciplinary expert panel. Comparison of surgical wound an infection after preoperative skin preparation with 4% chlorhexidine [correction of chlohexidine] and povidone iodine: a prospective randomized trial. Comprehensive consensus primarily based guidelines on intrathecal drug delivery techniques within the treatment of pain attributable to most cancers ache. The surgeon ought to have applicable fellowship training or further continuing schooling previous to doing the surgery. Psychological evaluation ought to be carried out on noncancer pain sufferers to assess appropriateness and psychological stability. In finish of life care, the psychologist may be useful in demise and dying discussions and correct counseling. Prior to implant, the patient ought to undergo a proper medical evaluation, laboratory testing, imaging, and training relating to the remedy. Trialing for intrathecal therapies are controversial and are done in a spread methods. The use of medications can predict outcomes for a pump together with both intrathecal and epidural administration, single shot and steady dosing, and inpatient and outpatient clinical settings. At this time, no long-term studies exist to predict the end result of trialing or eliminating the trial for the clinical process. Evidence-guided drug choice algorithms have been developed primarily based on best practices. When treating sufferers in an efficacious and protected manner, these algorithms must be considered, and accompanying security precautions ought to be adopted to improve outcomes. Opioids in chronic low back ache: a scientific evaluate and meta-analysis of efficacy, tolerability and safety in randomized placebo-controlled studies of no less than 4 weeks duration. Polyanalgesic consensus convention 2012: suggestions for the management of ache by intrathecal (intraspinal) drug delivery: report of an interdisciplinary expert panel. Device-related issues of long-term intrathecal drug therapy by way of implanted pumps. Polyanalgesic consensus conference-2012: recommendations to scale back morbidity and mortality in intrathecal drug supply in the therapy of persistent ache. Case of spinal cord compression syndrome by a fibrotic mass presenting in a patient with an intrathecal ache management pump system. Polyanalgesic consensus conference-2012: consensus on prognosis, detection, and remedy of catheter-tip granulomas (inflammatory masses). Cede�o forty six Introduction Electrical stimulation of nerves has become the main alternative to many neuroablative therapies for the remedy of chronic ache.
Order avanafil on lineThis scenario produces short-term blindness with reversible brokers or everlasting blindness with neurolytic brokers [33]. Retrobulbar hematoma and hematoma in cheek: Retrobulbar hematoma might develop if the needle is superior to the retrobulbar house. Infection: In the collection by Sweet, there were 24 cases of meningitis in 7000 cases. Defects in other cranial nerves: Ocular motor paralysis and cavernous sinus fistula are a risk [39]. Intracranial hemorrhage: Intracranial hemorrhage has been reported to be deadly [40]. Misplacement of needles into incorrect cranium base foramina can lead to vascular injury and secondary hypertension that, in turn, can lead to bleeding [41]. Precautions � Trigeminal neuralgia is usually diagnosed by the standard affected person history, a negative neurologic exam, and response to a trial of carbamazepine (Tegretol). Imaging research ought to be considered if the diagnosis is unsure or neurologic abnormalities are noted. The affected person have to be conscious between each coagulation application so that sensory testing of the face can take place. Trigeminal neuralgia is clinically identified by the key feature of a sudden and severe lancinating ache that normally lasts from a couple of seconds to 2 min within the 460 C. Demyelination of trigeminal sensory fibers throughout the proximal nerve root is likely the pathology of idiopathic trigeminal neuralgia and is most likely attributable to the compression from an overlying blood vessel on the root entry zone. Fluoroscopy is critical to get hold of each enough submental and lateral views with the assistant biplane intersection of three anatomic landmarks: beneath the medial aspect of the pupil, 2. The use of a curved needle is beneficial to improve entry to the foramen and to decrease the chance of complications. The endpoint of thermocoagulation is reached when the specified division of the trigeminal nerve has become barely analgesic however not anesthetic to reduce the risks of dysesthesia or anesthesia dolorosa. It is beneficial for 6 min at forty five V, with a pulse width of 10 ms and a pulse frequency of 4 Hz. Block of the terminal branches of the trigeminal nerve is primarily based on landmarks by palpation of the foramina. Incidence and medical options of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Die Leitungsanesthesie und Injektionsbehandlung des Ganglion Gasseri und der Trigeminusaeste. A strategy of injection into the gasserian ganglion under roentgenographic management. Controlled thermocoagulation of trigeminal ganglion and rootlets for differential destruction of ache fibers. Trigeminal neuralgia handled by the injection of glycerol into the trigeminal cistern. Arterial compression of the trigeminal nerve on the pons in patients with trigeminal neuralgia. Since sensory input from the upper cervical nerve roots converges into the trigeminal nucleus, patients with occipital neuralgia could present autonomic signs (nausea, vomiting, photophobia, diplopia, ocular and nasal congestion, tinnitus, and vertigo) [9]. Differential Diagnosis Includes Possible Sources of Pain � Median atlantoaxial, lateral atlantoaxial, and atlantooccipital joints � C2�C3 zygapophyseal joint � Suboccipital and upper posterior neck muscle tissue � Upper vertebral muscles � Spinal and posterior cranial fossa dura mater, vertebral arteries, C2�C3 intervertebral disc. Also structural or infiltrative lesions have been identified as attainable causes (meningioma, schwannoma, arteriovenous fistula, vascular compression, myelitis, multiple myeloma, and pyomyositis). Characteristically neurologic examination of the head, neck, and upper extremities is regular. Diagnosis can be confirmed when ache is transiently relieved by an area occipital anesthetic block [10]. Pain is situated within the distribution of the greater, lesser, and/or third occipital nerves. Pain has two of the following three traits: � Recurring in paroxysmal attacks lasting from a few seconds to minutes � Severe depth � Shooting, stabbing, or sharp in quality D.
Best purchase avanafilIndications While surgical trauma and ensuing neuralgia could also be implicated in a proportion of sufferers affected by anterior belly wall ache, neuralgia in the same distribution may also occur in the absence of surgery. The intercostal nerves traversing the rectus sheath can be entrapped as they course through the lateral side of the rectus abdominis muscle. With contraction of the rectus abdominis, entrapment worsens and ache develops [12]. The affected person is then asked to tense their stomach wall by raising their neck and shoulders from the exam table, and the stomach is examined again. If the pain is originating from the abdominal viscera, the tensed rectus abdominis muscle protects the abdominal contents, and the ache is attenuated in the subsequent examination. If the belly examination is unchanged or worsened by contraction of the rectus muscle, this means the ache generator originates from the stomach wall [14]. The needle is inserted in airplane with the transducer and programs from medial to lateral to keep away from the inferior epigastric vessels which additionally travel within the posterior rectus sheath Anatomy Fibrous extensions of the exterior stomach indirect, inner belly indirect, and transversus abdominis muscular tissues converge at an aponeurosis that envelops the rectus abdominis muscle ventrally. The rami of the T9-T11 are situated in a plane bordered anteriorly by the rectus muscle and posteriorly by the transversalis fascia. In addition to the neural constructions, the inferior epigastric artery and vein also traverse the rectus sheath, located posterolateral to the rectus muscle. Identifying these vascular constructions with ultrasound adds a degree of safety when in comparison with a blind approach. An ultrasound transducer is positioned transversely on the stomach lateral to the umbilicus. Real-time sonography is utilized to visualize the rectus muscle and its aponeurosis. The needle courses in aircraft with the ultrasound probe, passing via the subcutaneous tissue, the anterior layer of the aponeurosis, and into the rectus abdominis muscle. A fascial "pop" may be appreciated when the needle passes by way of the aponeurosis. The ultimate position of the needle tip should lie posterior to the rectus abdominis muscle and anterior to the transversalis fascia. The block is then repeated in an similar method on the contralateral aspect since the linea alba at midline prevents contralateral unfold of the injectate. Additionally, for the explanation that paravertebral space is contiguous with each the intercostal nerves and the epidural space by way of the vertebral foramen, epidural or intercostal block can happen at the facet of the paravertebral block. Precautions Technical Aspects Beginning with a medial needle insertion website and coursing laterally, in aircraft via the rectus muscle avoids a trajectory which may result in vascular damage. Optimizing the ultrasound picture might assist reduce the risk of inadvertent injection into the epigastric artery or vein and forestall the needle tip from passing via the transversalis fascia and into the peritoneal cavity. Several techniques have been described to carry out the paravertebral block utilizing landmarks, loss of resistance, pressure transducer, nerve stimulation, fluoroscopy, and ultrasound [15]. The landmark, or blind method, may be performed sitting, prone, or in a lateral decubitus position. The practitioner first identifies the spinous course of at midline, and an entry level 2. A Tuohy needle is superior to contact the transverse process, and the needle tip is then walked off the superior facet of the transverse course of 1 cm to enter the paravertebral house. As the needle passes through the costotransverse ligament, a "pop" may be appreciated, and the medicine is then injected. Chelly [15] employs a modification to again establish the transverse course of and notes its depth. He then withdraws the needle and marks a distance on his needle 1 cm past the depth of the transverse course of. The needle is then directed at a 45-degree angle by way of the costotransverse ligament with the tip residing within the thoracic paravertebral area. The blind approach can employ a hanging drop to exclude intrapleural needle placement.
|